To the Editor: The COVID-19 pandemic has caused a paradigm shift in health care delivery worldwide. There has been a consequent surge in telehealth usage,1 including Singapore.2 Dermatology is well-suited for telemedicine due to the visual diagnostic nature of the specialty. The pandemic also drove an unprecedented acceleration in the demand and use of teledermatology.3 This letter looks at Singapore’s experience with teledermatology over the years, before and through the pandemic.
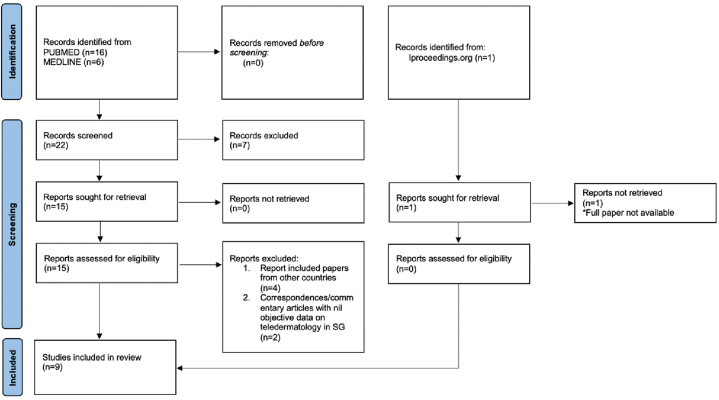
We examined a total of 9 studies exploring teledermatology in Singapore. A systematic search was performed on PUBMED, MEDLINE, and iProceedings with both the keywords “teledermatology” and “Singapore” inclusive (Fig 1).
Fig 1.
Summary of systematic review performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines.
Prior to the pandemic, 3 studies looked at the use of teledermatology in 2 special populations—nursing home residents and long-term institutionalized psychiatric patients (Table I). It often involves significant manpower and costs to bring these patients to specialist visits, explaining the potential role that teledermatology can play in these settings. These prospective studies have shown largely positive feedback from health care providers, without compromising diagnostic concordance compared to face-to-face visits. Teledermatology also reduced turnaround time and costs. Compared to these patients; however, the general public will still more likely opt for in-person consults due to easy accessibility. Chow et al explored perspectives of family physicians, dermatologists, and patients involved in a teledermatology service in 2019; which saliently identified the advantages and disadvantages of teledermatology, while providing suggestions on how to improve its implementation in Singapore’s primary care landscape.
Table I.
Studies reporting on Teledermatology in Singapore
| Study/type/period | Population involved | Number of participants | Mode of delivery | Outcome evaluation measures | Findings | Limitations |
|---|---|---|---|---|---|---|
| Lavanya et al1 Phase I of trial Prospective study October 2005 to July 2006 |
Nursing home residents from a selected NHSC in Singapore, elderly aged 65 and above | 12 patients and 5 nurses 2 dermatologists |
Store-and-forward | Online questionnaire for both nurses and doctors involved Multiple choices formatted analyzed using a multipoint scale weighted from 0 to 100. System usage/user activities monitored by examining server log in and database assess activities since beginning of system employment. Diagnosis module evaluated based on effectiveness of treatment made by dermatologists. |
System usage Total numbers of logins 30, 4% independent. Average duration for specialists to provide diagnosis was 4 days. Survey results 100% of nurses found an overall improvement in quality of health care with PHIMS but 60% would prefer patients to personally visit the specialist. Both dermatologists agreed that there was an improvement in quality of health care after using DPHIMS but one mentioned that medical care received using the system was not as good. Nurses felt most patients were not referred to dermatologists as they obtained concise diagnoses which led to improvement in skin conditions when resident doctors are able to prescribe relevant medications as suggested |
Small study population Responses were largely anecdotal feedback and experiences. |
| Lavanya et al2 Phase II of trial Prospective study August 2006 to July 2007 |
Nursing home residents from a selected NHSC in Singapore, elderly patients, with an average age 82 y 84% women |
50 patients registered by end of phase 2 11 died from causes not related to skin disorders during introductory phases 2 dermatologists 5 nurses (from phase I) 9 nursing aides |
Store-and-forward | User online surveys administered to nurses, nursing aide, and dermatologists to gauge level of satisfaction and experience | Monetary incentive allowed more active participation of matron in phase 2, which increased acceptance of DPHIMS. 78% of nurse aids expressed good agreement about overall improvement in quality of health care compared to an ordinary clinic visit. 100% of nurse aids were satisfied with the overall concept and performance of the system. Dermatologists were limited by the inability to touch and feel the patient, perform laboratory tests, and difficulty in building rapport with patients. System can save unnecessary visits to dermatologist and help obtain early treatment and regular follow-up at low costs, but the existing workflow of target users must be studied to ensure minimum workflow disruption. |
Small study population Possible bias from monetary incentive |
| Seghers et al3 Prospective study 18-month period, year not stated |
Long-term institutionalized psychiatric patients from Institute of Mental Health with chronic skin diseases on regular follow-up with National Skin Centre | 25 patients met recruitment criteria but only 13 recruited due to difficulties in obtaining consent 27 paired patient visits |
Synchronous Patient will be assessed via interactive telemedicine by consultant dermatologist then within 1 week reviewed by another consultant dermatologist FTF. Interphysician diagnosis and treatment plan agreement evaluated by independent consultant dermatologist |
(1) Interphysician clinical assessment and diagnosis (2) Interphysician treatment or management plan (3) Adverse events or outcomes (4) Total costs and turnaround time of each consultation Degree of agreements: (1) Complete agreement (2) Partial agreement (3) Disagreement |
All patients recruited were male schizophrenics with a mean age of 64.6 years. High level of agreement between teledermatology and FTF consult. 100% for history taking and physical examination. 96% for investigations, diagnosis, management plan, and treatment. 90% reduced turnaround time for teledermatology compared to FTF consult with a greater proportion of PTAT (66% vs 2%) spent with dermatologist in consultation. Total cost could be 56% lower for teledermatology due to reduction in manpower and transportation |
Unclear if blinding of third independent consultant dermatologist with regards to which dermatologist made respective diagnoses could have bias toward certain colleagues Small number of patients and patient visits Selection bias for male patients as most long stay patients at IMH are male |
| Chow et al4 Qualitative study, investigative report March-July, 2019 |
Family physicians and dermatologists who participated in teledermatology service established between National Healthcare Group Polyclinics and National Skin Centre. | 15 family physicians and 10 dermatologists. | Store-and-forward Qualitative review via FTF semi structure interviews. Digital audio recordings entered into NVivo. Data analysis followed Burnard’s structure approach to thematic content analysis. |
Explore doctors’ experiences of teledermatology, and refinements needed to improve the patient and professional experience | 6 themes identified: (1) Satisfaction with teledermatology service Both family physicians and dermatologists were positive and supported introduction of the service. (2) Perceived benefits for patients Doctors recognized that teledermatology offered patients convenience, saving them money and time travelling to specialist center Immediate availability of expert opinion reduced patient anxiety and enabled effective management to begin promptly. (3) Rationale for teledermatology Family medicine (FM): Reduction in number of cases referred for specialist care and reduction on skin center workload; better understand case-mix of skin problems in the community Dermatologists: Reduction in number of “inappropriate”, “Unwarranted” referrals. (4) Educational impact FM: Reinforce and improve diagnosis and management skills for common skin conditions. (5) Challenge of virtual consultations Dermatologists: Photographic quality can impact validity of diagnosis and advice, lack of ability to palpate or perform dermatoscopic examination. (6) Service refinements for the future FM: expand polyclinic formulary and services to include medications and treatments eg, cryotherapy recommended by dermatologists. |
Selection bias as not all doctors using teledermatology agreed to be interviewed. Did not capture perceptions of other members of the team including managers, nurses, and pharmacists who contribute to the maintenance of the system. |
| Chow et al5 Qualitative study, investigative report March-July, 2019 |
English speaking patients who had undergone teledermatology service established between National Healthcare Group Polyclinics and National Skin Centre. | 21 | Store and forward FTF semi-structured interviews conducted by researcher drained in qualitative interview techniques. |
Explore patients’ experiences of teledermatology service and how it could be improved for others. | 3 major themes (1) Positive perceptions of teledermatology Convenience by minimizing transport costs and loss of earnings Care in a familiar setting Timely consult Expert involvement Reassurance Better prepared for outpatient appointment Speed of specialist response Consultation with specialist without the cost. (2) Concerns about teledermatology Waiting time Apparent unsophistication of equipment used Unavailability of recommended medication in the polyclinic. (3) Suggestions for improving the patient’s teledermatology journey Dedicated facility to minimize time spent preparing for teledermatology referral Allow patients to leave polyclinic after their clinical data is transmitted and to be contacted later with details of management plan Expand teledermatology not just within polyclinics but also private GPs |
Monetary compensation could have caused selection bias. Small population |
| Tan et al6 Prospective study July 1 to October 1, 2020 |
All formal inpatient referrals to dermatology service for patients from isolation wards in Singapore General Hospital. | 65 4 Specialist dermatologists. |
Store and forward | Degree of agreement between teledermatology and FTF bedside diagnosis. | Inpatient store and forward teledermatology has 89.2% diagnostic concordance when compared to bedside consultations. | Study population restricted to acute respiratory illness or suspected COVID-19 cases influences the generalizability to entire inpatient population. |
| Choi et al7 Convergent parallel (Simultaneous qualitative and quantitative) mixed method study conducted on patients or their caregivers June 2020 to April 2021 |
Patients from an academic tertiary dermatologic center in Singapore | 942 participants | Hybrid teledermatology | Quantitative component utilized a questionnaire to assess reasons for use or non-use of teledermatology and user experience. Qualitative component involved in-depth one-on-one semistructured interviews to explore perceptions of teledermatology. |
Quantitative analysis Increased willingness to use dermatology during the pandemic compared to before. More willing for a routine follow-up compared to 1st visit Declining willingness to use teledermatology with eating of COVID-19 movement restrictions. Reducing need for transportation and waiting time was most common reason for use. Concern about visual clarity most common reason for non-use. Data privacy concerns were not significant in this sample. Qualitative analysis (4 themes) (1) Pragmatic considerations Diagnostic and treatment capability Strength of recommendation by physician Infection risk Costs Convenience Logistical and physical means Familiarity with technology (2) Emotional considerations Affective communication Novelty seeking (3) Data privacy (4) Patient’s purpose for consult Perception of disease severity Need for diagnosis |
Lack of comparable data prior to COVID-19. Did not seek insights and perspective from health care providers. |
| Seah et al8 Prospective study June-August, 2022 |
Close contact of monkeypox patients who received postexposure prophylaxis in the form of ACAM2000 live Vaccinia virus. | 13 | Synchronous Limited details on the exact system or platform used. | Objectives highlighted: (1) screen for symptoms consistent with monkeypox infection (2) Assess for successful inoculation via direct visualization of vaccination site morphological progression. (3) Detect serious reactions arising from PEP administration. (4) Evaluate for deterioration in mental health status during quarantine period. Also used to visually assess all exposed areas to confirm absence of skin lesions suggestive of monkeypox infection and ascertain fitness for rescindment of quarantine order, 1 day prior to exiting quarantine. |
Out of 13 patients who were vaccinated, 12 were assessed via telemedicine to have normal postvaccination reactions. One patient with poor “take” as noted but resolution of initial vaccine reaction without blistering was able to be promptly escalated for review by infectious disease physician. | Small study population Sensitive areas like perigenital and perianal regions required patients to perform self-assessment and only assessed via video conference if patient reported abnormalities or consented for a review via telemedicine. |
| Tian, B9 Prospective study Published 2022 Duration of study 6 months, exact dates not mentioned |
Aesthetic medicine patients recruited via GP referrals. | 102 | Store-and-forward Patients examined FTF by a doctor before start of study and monthly after Patient would then submit their photos via online system which were then interpreted by another independent doctor on the back end. |
Comparison of diagnoses made by FTF and teledermatology doctor. Level of satisfaction of patients with teleconsultation. |
High level of concordance (95.5%) in diagnosis between both doctors Discordance and missed diagnoses by teledermatology doctor attributed to insufficient quality of photographs. High level of satisfaction with teleconsultation (>80% agree or strongly agree). |
Details on what kind of online system was used, not explained Diagnosis made by FTF doctor assumed to be correct. |
D-PHIMS, Distributed personal health information management system; FM, Family medicine; FTF, Face-to-face; IMH, Institute of Mental Health; NHSC, Nursing home for senior citizens; PTAT, Patient turnaround time.
Through a more large scale mixed method study that offered hybrid teledermatology to patients, Choi et al explored reasons for use and non-use of teledermatology in the face of the COVID-19 pandemic. It has shown that while there is increased willingness to use teledermatology during challenging times, a multitude of concerns ranging from confidence in diagnostic and treatment abilities to data privacy, might still drive patients to opt for in-person consultations once movement restrictions relax. This reflects deeply entrenched health seeking behaviors in the local population, where face-to-face consultations are still deemed the gold standard.
Two other studies explored the use of teledermatology in managing patients with transmissible diseases, which demonstrated the applicability of teledermatology in the face of pandemics. Seah et al looked at the surveillance of postexposure prophylaxis in monkeypox close contacts, highlighting the advantages of teledermatology in the preservation of limited acute health care resources from clinical triaging, prevention of further disease transmission, and infection risk reduction for health care workers. Tan et al looked at teledermatology for patients isolated for respiratory symptoms or COVID-19 in a tertiary hospital and also showed a high level of concordance between teledermatology and in-person diagnoses.
In conclusion, logistical and infrastructural limitations, privacy concerns, and patient preferences, remain as common hurdles preventing teledermatology from becoming the mainstay of care. Clarity regarding legal and ethical issues, including safeguarding physicians making diagnoses online and confidentiality of patient data, must be established. Moving ahead, as a country with high smartphone penetration,4 smartphone teledermatology is an area of development that can potentially help improve ease of use, overcome logistical limitations, and make teledermatology more ubiquitous than before.
Key suggestions to improve teledermatology services:
-
1.
Use of smartphone teledermatology to improve on demand ease of use.
-
2.
Provision of medication delivery services after teleconsultation for the convenience of patients.
-
3.
Reduction of consultation fee for teledermatology to increase user uptake.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not required as per institutional guidelines of Singapore General Hospital.
References
- 1.Bestsennyy O., Gilbert G., Harris A., Rost J. Telehealth: a quarter-trillion-dollar post-covid-19 reality? McKinsey & Company. 2022. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
- 2.Nittari G., Savva D., Tomassoni D., Tayebati S.K., Amenta F. Telemedicine in the COVID-19 era: a narrative review based on current evidence. Int J Environ Res Public Health. 2022;19(9):5101. doi: 10.3390/ijerph19095101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loh C.H., Chong Tam S.Y., Oh C.C. Teledermatology in the COVID-19 pandemic: a systematic review. JAAD Int. 2021;5:54–64. doi: 10.1016/j.jdin.2021.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Statistic Singapore, infocomm and media - latest data. https://www.singstat.gov.sg/find-data/search-by-theme/industry/infocomm-and-media/latest-data