Abstract
A 77-year-old man arrived at our hospital with bilateral shoulder pain persisting for several months and headache for 1 month. Giant cell arteritis with polymyalgia rheumatica was suspected. However, considering his medical history of testing positive for syphilis, we submitted a sample for a syphilis serology test, which yielded positive results. The Treponema pallidum hemagglutination assay of cerebrospinal fluid was positive, and a temporal artery biopsy revealed vasculitis, confirming the diagnosis of tertiary syphilis. He was successfully treated for two weeks with penicillin G infusions. Symptoms reminiscent of giant cell arteritis and polymyalgia rheumatica may reveal syphilis, which is called the “great imitator.”
Keywords: giant cell arteritis, tertiary syphilis
Introduction
Giant cell arteritis (GCA) is an inflammatory disease of large blood vessels that can cause headaches, vision loss, and polymyalgia rheumatica (PMR)-like symptoms (1). When GCA is suspected, a temporal artery biopsy is the gold standard for the diagnosis (2). In such cases, we need to exclude prominent differential diagnoses, such as infections, neoplastic diseases, and autoimmune diseases that cause temporal artery inflammation (3).
We herein report a patient with a confirmed diagnosis of neurosyphilis who presented with headache and PMR-like symptoms. In this case, a temporal artery biopsy was performed, which showed inflammatory cell infiltration across all layers of the arterial wall, consistent with a diagnosis of GCA. In addition, the symptoms, physical examination findings, and laboratory data on presentation were suggestive of GCA and PMR. Therefore, including syphilis in the differential diagnosis for GCA was considered necessary.
Case Report
A 77-year-old Japanese man was referred to our hospital with bilateral shoulder pain for 2 months and left-sided headache for 1 month. The joint pain gradually worsened to the point where he could no longer reach objects on high shelves. Morning stiffness and loss of appetite were also observed. A fever, visual disturbance, and jaw claudication were not observed during the course of the disease. He had a history of diabetes, dyslipidemia, and gastric ulcer, for which he was on rosuvastatin 2.5 mg/day and sitagliptin 50 mg/day. No antibiotics had been prescribed since his symptoms had first appeared. He had tested positive for syphilis at another hospital a few years prior without any treatment. Although he denied sexual intercourse in the past few years, he had had intercourse with several people since his wife's death 20 years prior. His vital signs were normal when he came to the hospital, but he had a rubbery nodule in the left pubic region. His left temporal artery was not distended, tender, or pulseless. Due to pain, the shoulder joint range of motion was limited to 150° on the right and 90° on the left. There was no muscle weakness or lymphadenopathy. An ophthalmological examination revealed no evidence of ischemic optic neuropathy or uveitis.
Laboratory tests showed a white blood cell count of 6,970 /μL, a hemoglobin level of 11.3 g/dL, a mean corpuscular volume of 85.5 fL, a C-reactive protein level of 7.83 mg/dL, and erythrocyte sedimentation rate of 61 mm/h, indicating mild normocytic anemia and inflammation. Renal function tests, liver function tests, and electrolytes were all normal. The hemoglobin A1c level was 6.6%. Two sets of blood and urine cultures were negative. Based on his medical history, subsequent results of syphilis serology revealed positive findings for a Treponema pallidum latex agglutination assay (TPLA; SHINO-TEST, Tokyo, Japan) with a titer of 136.0 COI and rapid plasma regain (RPR; SHINO-TEST) with a titer of 2.4 RU. Lumbar puncture was performed, and the cerebrospinal fluid (CSF) TPLA test (Fujirebio, Tokyo, Japan) was positive at 77 U/mL, although his opening pressure was 85 mm H2O. Contrast-enhanced computed tomography (CT) revealed multiple nodules along the right spermatic cord, suggesting gumma; no other abnormal findings were noted (Fig. 1). His left temporal artery biopsy revealed marked intimal thickening, disruption of the internal elastic lamina, and transmural inflammation (Fig. 2). Accordingly, the patient was diagnosed with tertiary syphilis.
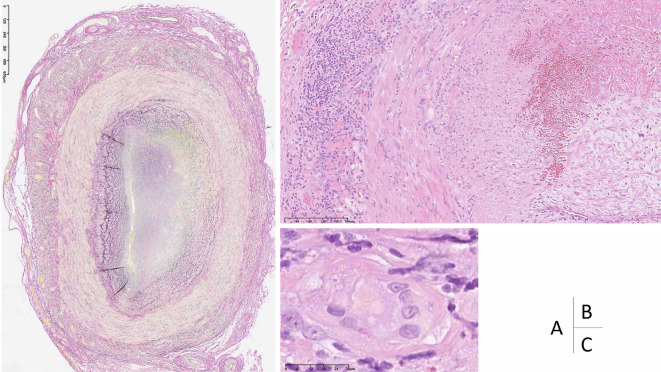
Figure 1.
Contrast-enhanced computed tomography was performed to exclude malignancy. CT revealed multiple nodules along the right spermatic cord, suggestive of gummas. The arrow shows an inhomogeneous soft-tissue-density nodule compatible with a gummatous lesion.
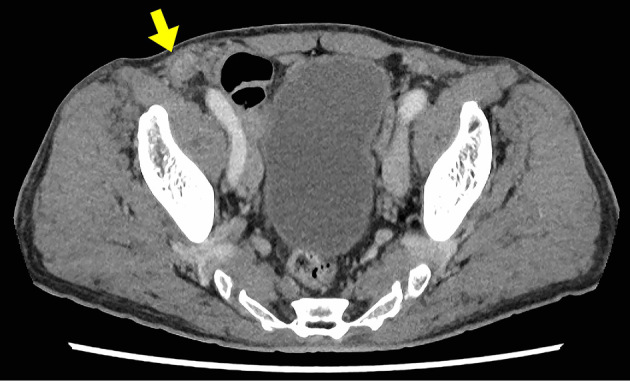
Figure 2.
Left temporal artery biopsy findings. Elastic van Gieson staining highlights disruption of the internal elastic lamina due to inflammation of the artery. The arterial lumen is not clearly visible (A). The arterial wall is infiltrated by chronic inflammatory cells (B), including histiocytes and multinucleated giant cells (C). The intimal layer is markedly thickened, causing luminal narrowing.
Treatment with penicillin G 24 million units per day alleviated his headache and shoulder pain within a few days. Treatment continued for 14 days. As of the writing of this report, three months have elapsed following the completion of his treatment, and his symptoms have not relapsed, although the RPR remained at 2.7 RU.
In this case, the possibility of temporal arteritis caused by syphilis and the combination of GCA and syphilis were considered. We suspected that the temporal arteritis had been caused by syphilis because the symptoms disappeared soon after treatment with penicillin G without relapse. The results of culture tests and imaging studies ruled out the possibility of an infection that could be treated with penicillin.
Discussion
GCA is a common large-vessel vasculitis among older patients (1). Depending on the vessel involved, GCA is classified into two types: cranial GCA, which affects the temporal artery, and large-vessel GCA, which affects the extra-temporal artery (4). Typical symptoms of cranial GCA are new-onset headaches, acute visual disturbances, jaw claudication, and proximal myalgia, which are key symptoms that aid in its diagnosis (1). However, in patients who display atypical manifestations, clinicians should perform a detailed assessment to exclude differential diagnoses. Infectious diseases, such as herpes zoster, salmonella, and tuberculosis; neoplastic diseases, such as lymphoma and chronic myelogenous leukemia; autoimmune diseases, such as Takayasu arteritis, Behçet's disease, and anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis; and IgG4-related diseases should be considered in such cases (3). Syphilitic arteritis is rare but has been reported several times in patients presenting with temporal arteritis (5-10).
Our patient was suspected of having cranial GCA and PMR because of pain and symmetrical range of motion limitation affecting the bilateral shoulder in addition to left-sided headache. He also had morning stiffness with a positive inflammatory reaction. However, he did not exhibit typical features of cranial GCA, such as vision loss or jaw claudication. Given his sexual and medical histories, we performed further investigations. Syphilis serology tests were positive in both serum and CSF, and gummas were observed in the inguinal region on a physical examination and CT, suggesting tertiary syphilis complicated by neurosyphilis. A temporal artery biopsy showed inflammatory cell infiltration. Accordingly, a diagnosis of temporal arteritis due to tertiary syphilis was made.
Syphilis is an infectious disease caused by Treponema pallidum and is known as the “Great Imitator” because of its diverse symptoms (11). If left untreated following infection, patients enter the asymptomatic or latent period. Tertiary syphilis occurs 5 to 30 years or more after the initial infection. Tertiary syphilis is mainly divided into cardiovascular syphilis, such as aortitis and aneurysm; neurosyphilis, such as paralysis and cognitive impairment; and gummatous syphilis (12). Cardiovascular syphilis is an inflammatory reaction to the invasion of Treponema pallidum into the aortic wall, which develops into occlusive endarteritis of the vasa vasorum, resulting in necrosis of elastic fibers and connective tissue in the aortic media (13). With the introduction of penicillin, all forms of tertiary syphilis have become rare. For this reason, most physicians have never encountered a case of tertiary syphilis. However, the incidence of syphilis has increased in recent years (12). In previous reports, syphilis cases presenting with temporal arteritis were first treated using steroids due to the delayed diagnosis (5-8). In the present case, we treated our patient with preceding penicillin based on the history and physical examination findings.
This case report describes a rare case of temporal arteritis caused by tertiary syphilis. Physicians should consider syphilis as a differential diagnosis for temporal arteritis when confronted with atypical symptoms and physical signs.
Written informed consent was obtained from the patient for the publication of this report and associated images.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Hoffman GS. Giant cell arteritis. Ann Intern Med 165: ITC65-ITC80, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Ness T, Bley TA, Schmidt WA, Lamprecht P. The diagnosis and treatment of giant cell arteritis. Dtsch Arztebl Int 110: 376-385; quiz 386, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caspary L. Inflammatory diseases of the aorta. Vasa 45: 17-29, 2016. [DOI] [PubMed] [Google Scholar]
- 4.Lensen KD, Voskuyl AE, Comans EF, et al. Extracranial giant cell arteritis: a narrative review. Neth J Med 74: 182-192, 2016. [PubMed] [Google Scholar]
- 5.Montebello A, Harmsworth D, Cassar PJ, Vella S. Neurosyphilis in a suspected case of giant cell arteritis. BMJ Case Rep 14: e242733, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Narayan N, Bennett P, Chan C, Rhodes B. Secondary syphilis mimicking giant cell arteritis. J Clin Rheumatol 26: 18-20, 2020. [DOI] [PubMed] [Google Scholar]
- 7.Sangesland A, Haugland HW, Næss IA, Stevens DJ. Syphilis with vision loss. Tidsskr Nor Laegeforen 141: 2021. [DOI] [PubMed] [Google Scholar]
- 8.Drew PJ. Secondary syphilis presenting with features of cranial arteritis. Postgrad Med J 57: 712-713, 1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leroux M, Pasquet A, Baclet V, et al. A case of neurological syphilis mimicking Horton's disease and polymyalgia rheumatica. Ann Dermatol Venereol 140: 619-622, 2013. [DOI] [PubMed] [Google Scholar]
- 10.Smith JL, Israel CW, Harner RE. Syphilitic temporal arteritis. Arch Ophthalmol 78: 284-288, 1967. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgerald F. The great imitator, syphilis. West J Med 134: 424-432, 1981. [PMC free article] [PubMed] [Google Scholar]
- 12.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 70: 1-187, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen SE, Klausner JD, Engelman J, Philip S. Syphilis in the modern era: an update for physicians. Infect Dis Clin North Am 27: 705-722, 2013. [DOI] [PubMed] [Google Scholar]