Abstract
Anemia is a frequent complication in pediatric kidney transplant recipients (KTR) with a variable reported prevalence estimated between 20 and 80% depending on how defined. Causes of and risk factors for post-transplantation anemia (PTA) are multifactorial with iron deficiency being the primary cause of early PTA (within the first 6 months after transplantation) and impaired glomerular filtration rate (GFR) commonly responsible for late PTA (after 6 months). Medications, viral infections, chronic inflammation and comorbidities also play a role. PTA has relevant long-term consequences and is a potential risk factor for allograft dysfunction, cardiovascular morbidity and mortality. Thus, an anemia evaluation, approximately three months post-transplantation, is recommended in order to start early treatment and improve prognosis. Iron status, vitamin B12, folate, markers of hemolysis and viral PCR should be checked and medications, in particular combinations of medications, should be carefully evaluated. PTA treatment may be challenging and should be directed to the underlying causes. Iron supplementation and erythropoietin therapy, not extensively used in KTR, may be indicated. Every effort should be made to avoid blood transfusions in the pre-transplant period to avoid allosensitization. Anemia should be corrected to prepare candidates for kidney transplantation in order to reduce the need for peri-operative blood transfusions as well.
Keywords: Anemia, kidney transplantation, iron deficiency, allograft dysfunction, erythropoietin stimulating agents, blood transfusion
Introduction
Erythropoiesis stimulating agents (ESA) and iron supplements remain the primary agents used to treat anemia in children with chronic kidney disease (CKD), both pre- and post-dialysis. Although many children are able to stop ESA treatment after successful kidney transplantation, the prevalence of anemia after transplant may be underestimated [1]. Despite advances in transplant care, anemia is frequently present in kidney transplant recipients (KTR), reported between 20 and 80% at various time points after transplantation [1–8]. Post-transplantation anemia (PTA), which is generally normocytic and normochromic [9], is more common immediately after transplantation, even in the case of early stabilization of graft function [5, 6, 9]. Although erythropoietin dysregulation and iron deficiency may contribute to PTA, there are other unique mechanisms of anemia in transplant recipients, and the approaches to treatment may differ (Figure 1). In this review, we will summarize the risk factors for, and mechanisms of, anemia after kidney transplantation in children, as well as the association between PTA and clinical outcomes including long-term graft function. The approach to prevention, diagnosis and management of PTA will also be reviewed.
Figure 1.
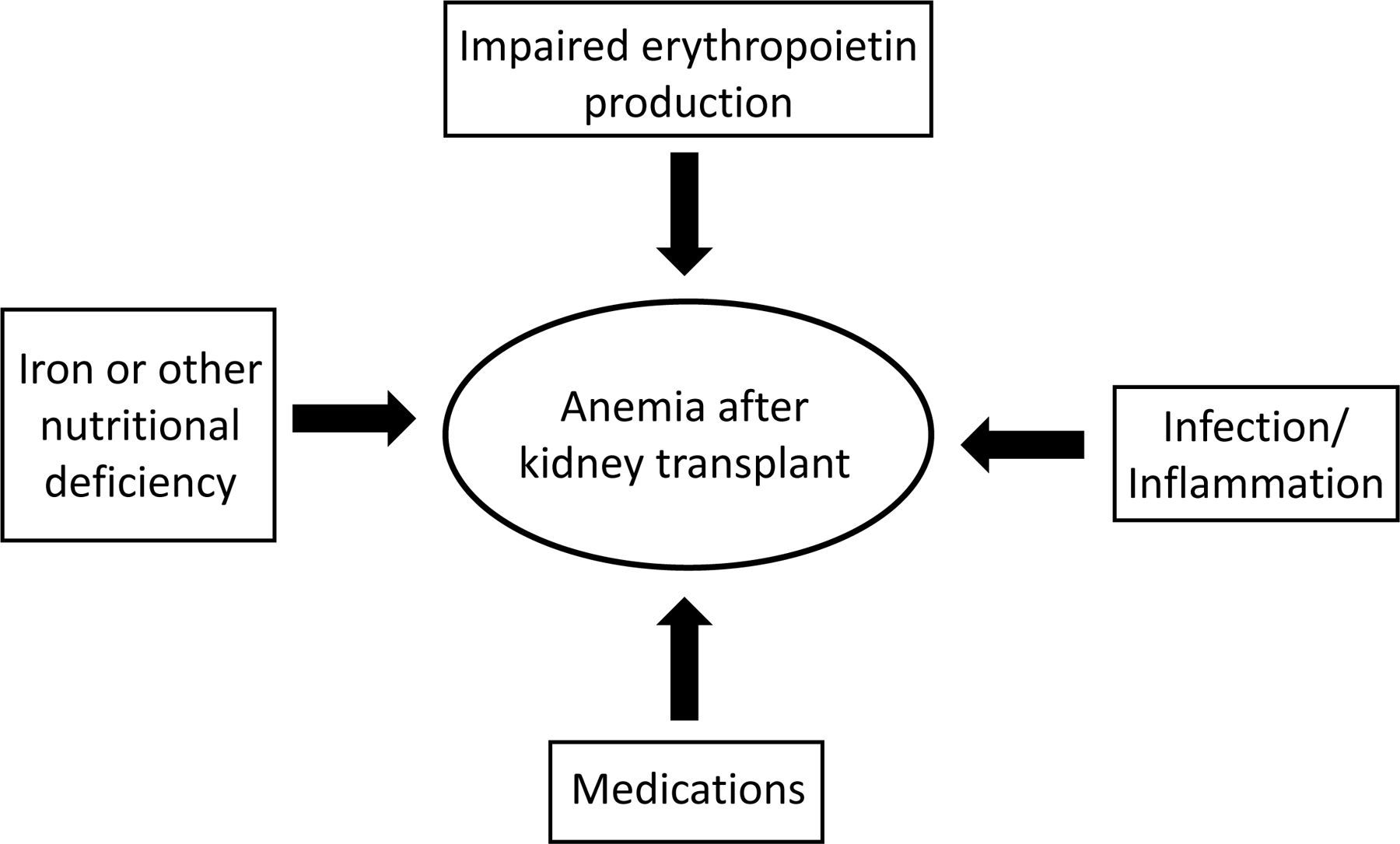
Major contributors to anemia after kidney transplantation
Definition and prevalence of PTA
Early PTA refers to anemia diagnosed within the first 6 months after transplant, while late PTA is diagnosed beyond 6 months [10]. The prevalence, based on time since transplant in pediatric recipients, has been estimated as 80–87% at 1 month, 20–48% at 1 year and 35–57% thereafter [5, 6, 9]. There is some variability in reported PTA prevalence, likely related to the variability in the definitions applied in different studies. Yorgin et al. defined anemia in pediatric and young adult KTA as a hematocrit level of > 2 SD below mean for age from population-based data [5]. Mitsnefes et al. diagnosed anemia in children if hemoglobin < 11 g/dl and severe anemia if hemoglobin < 10 g/dl [6], whereas Kausman et al. considered different hemoglobin cut-off values matching to age [7]. This is in accordance with the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines on anemia management in CKD, which is also intended to guide anemia management in KTR [11]. Based on this, anemia is defined as hemoglobin concentration of < 11 g/dl in children 0.5–5 years, < 11.5 g/dl in children 5–12 years, < 12 g/dl in children 12–15 years, < 13 g/dl in males > 15 years and < 12 g/dl in females > 15 years [11]. Mitsnefes et al. demonstrated in a single-center cohort of children transplanted over a 25-year period that PTA prevalence was lowest before 1986 (7.8%), but increased to 29% after calcineurin inhibitor use became standard of care and to 32% once mycophenolate mofetil was introduced into routine post-transplant immunosuppression regimens in children [6]. Thus, prevalence has changed over time as immunosuppressive agents with mechanisms of action that promote anemia have been introduced.
Risk factors and pathogenesis
Risk factors for PTA are multifactorial and summarized in Table 1. Some of the mechanisms of anemia in CKD in general, such as iron deficiency and impaired erythropoietin (EPO) production, also apply in PTA. In the immediate post-transplant period, iron deficiency is common. In particular, reduced iron stores before transplantation, poor nutritional intake, blood loss during surgery and frequent perioperative blood sample collection may all contribute to iron deficiency and consequently PTA [1, 7]. In addition, endogenous EPO production by the kidney allograft increases with time post-transplantation, and low EPO levels may be documented for at least 8 days, particularly in patients who experience delayed graft function or early acute rejection [12]. Medications are also important contributors to PTA. Both induction immunosuppressive (thymoglobulin) and maintenance immunosuppressive drugs (mycophenolate mofetil, azathioprine) may induce a bone marrow suppression and consequent anemia [13]. Similarly, viral and bacterial infection prophylaxis agents (ganciclovir, trimethoprim-sulfamethoxazole) share the same mechanism and may contribute to PTA [14, 15]. Viral infections, including CMV, EBV, BK virus, Parvovirus B19 can directly cause hematological abnormalities through various mechanisms including production of inhibitory cytokines, decreased production of hematopoietic factors or direct infection of erythrocyte precursors, resulting in maturation arrest at the pro-normoblast stage hematopoietic factors [7, 14, 15]. Finally, some studies also reported that gender and age could be influencers with female and younger patients more frequently anemic, especially in the first months after transplantation.
Table 1.
Risk factors for early and late PTA
| Early PTA (<6 months) | Late PTA (>6 months) |
|---|---|
| Pre-transplant anemia | Early PTA |
| Poor nutrition - Iron deficiency pre-Tx | Impaired GFR |
| - B12 deficiency | Iron deficiency |
| - Folate deficiency | Maintenance immunosuppression (MMF, AZA) |
| Frequent phlebotomy, surgery blood loss | Ace-inhibitors |
| Induction immunosuppression | Acute rejection |
| Virus and bacterial prophylaxis | Infections |
| Infections | Comorbidities |
| Delay graft function | Chronic inflammation |
| Acute rejection | Hyperparathyroidism |
| Hyperparathyroidism | |
| Female gender | |
| Younger age |
Tx transplantation, MMF micophenolate mofetil, AZA azathyoprine
Impaired GFR is the predominant contributing factor of late PTA together with iron, vitamin B12 and folic acid deficiency [1]. Furthermore, chronic inflammation, comorbidities, infections and medications are other determining factors in late PTA [10]. In particular, among drugs, maintenance immunosuppressives as for early PTA but also ACE inhibitors or angiotensin receptor blockers may be responsible for anemia in stabilized transplanted patients [10].
Clinical associations with PTA
Mortality and allograft dysfunction
In adults, anemia after kidney transplant has been identified as a risk factor for cardiovascular disease, allograft dysfunction and loss, and even mortality [16–23]. Severe anemia (hemoglobin < 11 g/dl) was associated with high risk for a composite outcome of graft failure and mortality in adults with milder anemia (hemoglobin 11–12 g/dl) [15]. In addition, iron deficiency has been independently associated with risk for death in adult transplant patients, suggesting that iron deficiency may be a link between anemia and mortality [24]. Other studies conducted in adults showed conflicting results regarding patient mortality but confirmed the significant association between anemia and graft loss [2, 25–29].
In children, analysis of data from the ESPN/ERA-EDTA Registry revealed that low hemoglobin levels (defined as < 9.5 g/dl in children < 2 years, < 10 g/dl in children ≥ 2 years) increased the likelihood of a composite endpoint of kidney transplant graft failure or death. However, low hemoglobin was not significantly associated with the outcome of death only [8]. Similarly, Mitsnefes et al. in a cohort of 231 patients showed that children with early anemia (defined as hemoglobin < 11 g/dl) had significantly worse allograft survival than children without anemia [6]. However, when a Cox proportional hazards model was adjusted for race and transplant era, anemia was no longer an independent predictor of graft failure, suggesting that race may be correlated with anemia in this population, possibly due to increased prevalence of hemoglobinopathies in non-white children [6]. A more recent study performed in 128 pediatric KTR with longitudinal follow-up found that decreased hemoglobin levels (by age and sex-adjusted reference values) preceded decline in glomerular filtration rate (GFR) by several years [9], suggesting that anemia may be an early indicator of kidney allograft dysfunction, and raising the question of whether anemia contributes to allograft dysfunction rather than acting solely as a marker. They did observe an inverse correlation between hemoglobin and serum EPO and erythrocyte sedimentation rate (ESR) level as a marker of inflammation, but no correlation between hemoglobin and hepcidin, interleukin-6, or levels of C-reactive protein [9]. Protocol biopsies in these patients demonstrated that anemia correlated with interstitial fibrosis, and low hemoglobin was observed in 50% of those with significant interstitial scarring but in only 17% of those without [9]. Fibrosis is certainly associated with damage to EPO-producing peritubular fibroblast cells resulting in decreased EPO production and anemia, but the sequence of development of fibrosis and anemia is not entirely clear. One proposed mechanism is that low hemoglobin results in decreased oxygenation of the kidney interstitium, leading to perpetuation of inflammation and fibrosis [30].
Cardiovascular morbidity
Anemia in adult kidney transplant recipients is associated with several adverse cardiovascular outcomes including left ventricular hypertrophy (LVH) and heart failure [31, 32]. Although pediatric kidney transplant recipients have a lower burden of cardiovascular disease than adult recipients overall, some adverse associations with anemia have been observed in children as well. In a study conducted with 73 KTR, LVH was observed in 47.9% of patients and anemia remained a significant risk factor for LVH in multivariate analysis [33].
Diagnostic approach to PTA
KTR should be screened frequently for anemia. Recommendations include frequent hemoglobin monitoring following transplant (weekly for 1–2 months, then every other week for months 3–4, spacing to monthly for months 4–12, and then spacing further as clinically indicated) [34]. Furthermore, a full anemia evaluation at approximately 3 months post-transplantation is recommended in order to optimize anemia detection and treatment (2).
The diagnostic evaluation of PTA is outlined in Table 2. The process should include evaluation of red blood cell indices, reticulocyte count, measurement of biomarkers of iron status, folate, vitamin B12, and testing for the presence of hemolysis if clinical suspicion is high (lactate dehydrogenase, haptoglobin) [2]. If iron deficiency is diagnosed, other nutritional deficiencies should be ruled out and investigation for possible gastrointestinal bleeding performed, if indicated. In a study by Krause et al. comparison of hematologic parameters between pediatric pre-transplant and transplanted patients revealed iron saturation and serum ferritin levels significantly lower in CKD children compared to transplanted and similar EPO levels between the groups [35]. These results may suggest good iron storage and availability and EPO resistance in transplanted patients [35].
Table 2.
Diagnostic work-up of PTA
| Labs | Medications | Viral infections |
|---|---|---|
| Complete blood count Reticulocyte count Serum Iron Percent transferrin saturation Serum ferritin Folate Vitamin B12 LDH Haptoglobin PTH PCR Blood stool test |
Maintenance immunosuppression (MMF, AZA) ACE-inhibitors Angiotensin receptor blockers Viral prophylaxis agents (gancyclovir) Bacterial prophylaxis agents (sulfamethoxazole and trimethoprim) Allopurinol (combined with AZA) |
PCR and IgM, IgG: Parvovirus B19 CMV EBV BK virus Hepatitis B Hepatitis C HIV |
LDH MMF micophenolate mofetil, AZA azathyoprine
Specific attention to medications is also important with regard to immunosuppressive drugs, viral and bacterial prophylaxis agents, and ACE inhibitors or angiotensin receptor blockers. In particular dapsone, used for the prevention of Pneumocystis carinii pneumonia in KTR who cannot receive trimethoprim-sulfamethoxazole. is contraindicated because it can cause methemoglobinemia. In a study of 31 KRT children receiving dapsone, only 41.9% were screened for acquired methemoglobinemia, and of those, 77% tested methemoglobin-positive [36]. Combinations of medications increasing risk for anemia should also be considered. Bone marrow suppression caused by azathioprine (AZA) and allopurinol used in combination has been reported secondary to inhibition of xanthine oxidase by allopurinol and consequent impairment of AZA metabolism [37]. Evaluation for viral infections must be included in the assessment of PTA. Pure red cell aplasia may suggest parvovirus B19 infection, but other viruses including cytomegalovirus (CMV), BK virus, Epstein-Barr virus (EBV), hepatitis B and C, and human immunodeficiency virus (HIV) can cause aplastic anemia. Unexplained anemia with reticulocytopenia or pancytopenia should raise clinical suspicion of viral infection, which requires serologic testing for specific immunoglobulin IgM or IgG and PCR in blood or tissue for diagnosis [38].
Anemia prevention
Special attention should be paid to pre-transplant anemia as a risk factor for early PTA, and early PTA as risk factor for late PTA. Effective anemia treatment before transplant helps to mitigate the effects of surgical bleeding and high-volume fluid administration, reducing the requirement for a packed red blood cell infusion [39]. In a pediatric retrospective cohort study of recipients < 30 kg, pre-transplant hemoglobin was the only independent predictor of post-transplant transfusion, and pre-transplant hemoglobin > 12 g/dl provided protection from transfusion [40]. A study in adults examining 0-hour transplant biopsies found that patients who had interstitial fibrosis and tubular atrophy in > 5% of the sampled area had increased prevalence of anemia at 12 months post-transplant (53%) compared to patients who did not (35%) [41]. The presence of interstitial fibrosis and tubular atrophy may identify patients at high risk for PTA and may require treatment with ESA sooner.
Treatment of PTA
In the absence of specific guidelines for the treatment of anemia after kidney transplant, use of ESA and iron supplements are the mainstay of management [42, 43], although the optimal target hemoglobin level for KTR remains poorly defined. The optimal timing of intervention for anemia is debated, but even mild (hemoglobin between 10 and 11.9 g/dl) anemia in patients > 3 months following successful transplantation has been associated with increased mortality risk in the post-transplant years [22]. Consideration of medications that may be contributing to anemia is critical, as use of alternative drugs, if appropriate, may be helpful in modifying anemia risk. Anemia-associated viral infections, if present, should be treated e.g. with IVIG for parvovirus B19 infection or reduction in immunosuppression for BK virus or EBV [14].
Iron supplementation
Iron deficiency is the one of the most easily treatable causes of anemia. Although there is substantial evidence for the efficacy of iron supplementation in CKD and dialysis patients, data in KTR are more limited. The same criteria to define iron deficiency in CKD children, ferritin < 100 ng/ml and TSAT < 20%, are usually employed in transplant recipients [44]. Using these biomarker thresholds to define iron deficiency, pre-transplant rate of iron deficiency of 20% in children and adolescents with CKD and kidney failure, has been reported, which increased to 80% within 2 weeks post-transplant [45]. Both orally administered or intravenous iron can successfully replete iron stores [46]. In addition, a diet rich in iron should also be encouraged, including iron-fortified whole grains, dried beans, red meats, liver and spinach [47]. Vitamin B12 and folate supplementation may also be required based on results of the laboratory evaluation.
If oral supplementation is adopted, the dose range is 2–6 mg/kg elemental iron daily divided in two doses given on an empty stomach or with vitamin C-containing foods. An interaction between oral iron and mycophenolate mofetil causing a remarkable decrease in mycophenolate mofetil adsorption has been suggested but not confirmed in a larger randomized study [48, 49]. However, gastro-intestinal side effects (especially in case of concomitant therapy with mycophenolate mofetil) may limit oral iron adherence in children, making IV iron supplementation an attractive and relatively safe option [44, 50, 51]. There is some evidence that in iron-deficient women specifically, alternate-day iron supplementation may be associated with enhanced fractional iron absorption compared to a daily supplement regimen, without any difference in reported gastro-intestinal side effects [52]. The proposed mechanism for this effect is that iron ingestion transiently increased serum concentration of the iron-regulatory protein hepcidin, which subsequently blocks enteral iron absorption [53]. However, this modified dosing regimen has not been studied in children or transplant recipients.
A 2019 Cochrane systematic review, examining the efficacy of intravenous iron vs. oral iron therapy for adults and children with kidney disease, did include some studies of KTR and demonstrated superior performance of intravenous iron over oral therapy in terms of iron store repletion, but overall there have been limited studies examining the efficacy of parenteral iron supplementation in transplant recipients specifically [54]. In a retrospective observational study published in 2020, Iorember et al. reported a comparison of 37 children and adolescents who received a single infusion of 1–2 mg/kg IV iron sucrose within 2 weeks of kidney transplantation to a historical control group of 42 pediatric transplant recipients who did not receive parenteral iron therapy [45]. They reported decreased frequency of iron deficiency and low hemoglobin by 3 and 6 months, and lower frequency of transplant dysfunction (defined as eGFR < 60 mL/min/1.73 m2) at 1 and 2 years in those who received post-transplant parenteral iron compared to those who did not [50]. However, safety concerns about intravenous iron in KTR exist including adverse reactions/anaphylaxis associated with hypotension and the consequent risk of graft thrombosis, and the risk of using parenteral iron during active infections due to impairment of neutrophil and T- and B-lymphocyte function [55, 56]. Attention to dosing and rate of infusion may mitigate these risks, but no prospective studies in pediatric KTR have been performed to evaluate the effectiveness and safety of IV iron [54].
Erythropoiesis stimulating agents (ESA)
Optimal management of the anemia of CKD prior to kidney transplantation may help to minimize the need for red blood cell transfusions after transplant. However, although anemia is frequent, ESA use post-transplant is low, used in fewer than 10% of patients [5, 8]. In addition, the optimal timing of ESA initiation and the effectiveness in the peri-transplant period remain unclear. There is evidence from animal studies that erythropoietin given peri-transplant may be protective against ischemia-reperfusion injury but there have been few studies examining this in humans [57]. Proposed mechanisms for this include EPO-induced recruitment of endothelial progenitor cells (required for vascular repair), and promotion of cell survival and anti-apoptosis via JAK2, STAT5, and NFΚB [58]. But concerns about potential adverse effects of ESA used in the peri-transplant period remain. In a meta-analysis of clinical trials conducted in a total of 356 adult KTR which examined efficacy and safety of ESA treatment at the time of transplant, there was no difference in the occurrence of thromboembolic events, acute rejection, or hypertension between patients randomized to receive ESA pre- or intra-operatively and control subjects [57]. Notably, the optimal target hemoglobin level in KTR treated with ESA may be higher than that suggested in pre-transplant kidney disease. In a retrospective study conducted in transplanted adults, lower mortality risk was observed with hemoglobin increase up to 12.5 g/dl [59]. Furthermore, in the Correction of Anemia and Progression of Renal Insufficiency in Transplant patients study in adults, correction of hemoglobin to 13–15 g/dl with epoetin-beta preserved GFR and improved graft survival and quality of life without an increase in cardiovascular events over 2 years of follow-up [60]. According to Purroy et al., recombinant human erythropoietin (rHuEPO) may have immunomodulatory properties with significant impact in transplanted patients. ESA treatment may improve kidney transplant outcomes through regulation of immune tolerance inhibiting conventional T cells and promoting regulatory T cell function [61].
In children, limited data on ESA therapy after kidney transplantation are available. In Yorgin et al., the number of patients receiving ESA after transplantation ranged between 1.5% and 13.3% up to 6 years after transplant, despite anemia severity very similar to that at the time of transplant [5]. ESA use was reported in 15% of patients with PTA at 1-year post-transplant in one single-center retrospective study, and the prevalence of PTA has increased over time, suggesting that secular trends in immunosuppressive agent use contribute to this change [6]. In 2007, Nagarajan et al. reported, in a retrospective case-control study conducted on pediatric KTR, an increased risk of hypertension and renovascular stenosis in children who received ESA treatment for anemia in the first week after kidney transplantation [62]. However, the number of patients studied was small (only 11 children received ESA) and similar observations have not been reported in adults; additional studies would be needed to confirm this [58].
Dose of rHuEPO used to treat PTA has been reported to range from 100–300 IU/kg/week 1–3 times weekly as initial dose and 100 IU/kg/week weekly as maintenance dose [5, 63]. In order to enhance treatment adherence, methoxy polyethylene glycol (MPG)-EPO has been developed. MPG-EPO is a continuous EPO receptor activator with an extended half-life compared to either epoetin or darbepoetin which allows a longer interval between doses. MPG-EPO has been used in PTA treatment with success. In a small study, conducted in 12 pediatric KTR with anemia, a once-monthly intravenous injection of MPG-EPO administered at a median dose of 2.5 μg/kg achieved successfully corrected and maintained hemoglobin over a period of 6 months [64]. To date, there have been no studies evaluating the safety and efficacy of hypoxia inducible factor inhibitors, which induce endogenous erythropoietin production via an ESA-independent pathway, for the treatment of PTA in children.
Physical activity
The benefits of regular physical activity, which include positive cardiovascular and metabolic effects, may extend to improving the biochemical markers of anemia in transplant recipients [65]. In particular, physical exercise may improve peak VO2 (oxygen uptake during peak exercise) which is correlated to the increase in hemoglobin and the prevention of anemia [66]. Recently, a systemic review including 24 studies and more than 600 adult KTR failed to demonstrate a relevant impact on anemia of exercise intervention despite improved quality of life [67]. No data on anemia-related benefits of exercise in pediatric KTR are available.
Blood transfusion after transplantation
In clinical practice every effort to avoid red blood cell transfusion in children with chronic kidney disease is made, but transfusions are common especially in the immediate post-transplant period. Verghese et al. examined blood transfusions after transplant and associated outcomes in children < 18 years in a retrospective analysis. They found that the frequency of transfusions increased over time; 60% of those transplanted 2002–2014 received transfusions compared to 31% transplanted from 1984–1995 and 53% from 1995–2002 [66]. This trend in anemia prevalence may be explained by increased use over time of immunosuppressive medications which cause more severe anemia, including mycophenolate mofetil. Furthermore, of those who received packed red blood cells, 39% were received within 1 month of transplant, 13% from 1–12 months, and 48% beyond 12 months [65]. Reassuringly, there was no observed association between transfusion and the prevalence of donor-specific antibody or acute cell- or antibody-mediated rejection compared to children who did not receive transfusions, although those who received transfusions did demonstrate lower eGFR at 12 months from transplant [68]. Thus, PTA may be a marker of poorer graft function rather than a cause. Similarly, in a retrospective single center study examining 42 transplants, 50% of pediatric KTR 1–17 years of age received blood transfusions in the first week after transplant with most transfusions administered during surgery or within the first 24 h post-transplant [40]. In a cohort of 390 non-HLA sensitized adults transplanted 2008–2012, 64% received a blood transfusion within one year of transplant, with nearly 95% of those requiring a transfusion within the first post-transplant month [69]. Blood transfusion was independently associated with new donor-specific antibody formation (7.2% in transfused patients vs. 0.7% in those without transfusion), but not for antibody mediated rejection [69].
Conclusion
Anemia remains a common complication after kidney transplantation in children, and as in children with pre-transplant anemia, the mainstays of management remain iron supplementation and ESA therapy. Many medications used after transplantation confer additional risk of anemia in this population. Red blood cell transfusion is frequently required after transplant and may be associated with increased incidence of donor-specific antibody. Thus, attention to optimal anemia management prior to transplantation is required to minimize need for transfusion. There have been no clinical trials to assess ESA safety in the immediate post-transplant period in children.
Table 3.
Treatment of PTA
| Treatment | Dosage |
|---|---|
| Oral iron supplementation | 2–6 mg/kg/day of elemental iron in 2–3 doses |
| Vitamin C | 500 mg-2 g/day in 2–3 doses |
| IV iron supplementation | |
| Sodium ferric gluconate (SFG) | 1–1.5 mg/Kg diluted in 50 ml of 0.9% sodium chloride over 60 minutes |
| Iron sucrose | 1–2 mg/Kg diluted in 25 ml of 0.9% sodium chloride over 60 minutes |
| Ferric carboxymaltose | 2–8 mg/Kg in 20 ml of 0.9% sodium chloride over 15 minutes |
| Epoetin alfa | Initial dose: 100–300 IU/Kg/week, 1–3 times weekly Maintenance dose: 100 IU/Kg/week, weekly |
| Darbepoetin | 0.45 mcg/kg/week or 0.75 mcg/kg/every 2 weeks |
| Methoxy polyethylene glycol-EPO | 0.6 mcg/Kg ever 2 weeks, or based on manufacturer’s conversion factor if converting from other ESA |
| Folic acid | 5–10 mg/day |
| Vitamin B12 | 0.5–1 mg/week |
Key summary points.
Anemia is a frequent and underestimated complication of kidney transplantation
PTA has been associated with increased morbidity and mortality in KTR, in particular with allograft dysfunction
Despite a high prevalence of PTA, the number of patients receiving ESA therapy in the post-transplant period is very low and there are no contraindications to its use
Multiple choice questions (answers provided following the reference list).
- Early post-transplant anemia is defined as anemia diagnosed
- Within 12 months after kidney transplant
- Within 6 months after kidney transplant
- Within the first month after kidney transplant
- At the 3 month post-transplant visit
- Any time after transplant
- Which of the following is NOT a risk factor for post-transplant anemia?
- Pre-transplant anemia
- Delayed graft function
- Iron deficiency
- Corticosteroids
- Viral infection
- Post-transplant anemia has been associated with a variety of clinical outcomes in adults including
- All-cause mortality
- Allograft dysfunction
- Left ventricular hypertrophy
- Congestive heart failure
- All of the above
- The initial diagnostic evaluation for PTA in children should include all of the following EXCEPT
- Measurement of biomarkers of iron status including ferritin and transferrin saturation
- Review of medications to identify those associated with increased risk for anemia
- Measurement of reticulocyte count
- Ultrasound to assess for intra-abdominal hematoma
- Testing for the presence of hemolysis if clinical suspicion is high
- The optimal post-transplant hemoglobin level in children
- Has not been defined
- Is the same as the optimal hemoglobin level in adult kidney transplant recipients
- Depends on the dose of erythropoiesis stimulating agent they are treated with
- Is lower for those receiving iron supplementation
- Is > 11 g/dl
Answers.
1. b; 2. d; 3. e; 4. d; 5. a
Footnotes
Competing interests IG declares no competing interests. MAA is a member of the editorial board of Pediatric Nephrology.
References
- 1.Galutira PJ, Del Rio M (2012) Understanding renal posttransplantation anemia in the pediatric population. Pediatr Nephrol 27:1079–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gafter-Gvili A, Gafter U (2019) Posttransplantation Anemia in Kidney Transplant Recipients. Acta Haematol 142:37–43 [DOI] [PubMed] [Google Scholar]
- 3.Gafter-Gvili A, Ayalon-Dangur I, Cooper L, Shochat T, Rahamimov R, Gafter U, Mor E, Grossman A (2017) Posttransplantation anemia in kidney transplant recipients: a retrospective cohort study. Medicine 96:e7735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vanrenterghem Y, Ponticelli C, Morales JM, Abramowicz D, Baboolal K, Eklund B, Kliem V, Legendre C, Morais Sarmento AL, Vincenti F (2003) Prevalence and management of anemia in renal transplant recipients: a European survey. Am J Transplant 3:835–845 [DOI] [PubMed] [Google Scholar]
- 5.Yorgin P, Belson A, Sanchez J, Al Uzri A, Sarwal M, Bloch D, Oehlert J, Salvatierra O, Alexander S (2002) Unexpectedly high prevalence of posttransplant anemia in pediatric and young adult renal transplant recipients. Am J Kidney Dis 40:1306–1318 [DOI] [PubMed] [Google Scholar]
- 6.Mitsnefes M, Subat-Dezulovic M, Khoury P, Goebel J, Strife CF (2005) Increasing incidence of post-kidney transplant anemia in children. Am J Transplant 5:1713–1718 [DOI] [PubMed] [Google Scholar]
- 7.Kausman JY, Powell HR, Jones CL (2004) Anemia in pediatric renal transplant recipients. Pediatr Nephrol 19:526–530 [DOI] [PubMed] [Google Scholar]
- 8.Krischock LA, van Stralen KJ, Verrina E, Tizard EJ, Bonthuis M, Reusz G, Hussain FK, Jankauskiene A, Novljan G, Spasojevic-Dimitrijeva B, Podracka L, Zaller V, Jager KJ, Schaefer F; ESPN/ERA-EDTA Registry (2016) Anemia in Children Following Renal Transplantation-Results From the ESPN/ERA-EDTA Registry. Pediatr Nephrol 31:325–333 [DOI] [PubMed] [Google Scholar]
- 9.Miettinen J, Tainio J, Jahnukainen T, Pakarinen M, Lauronen J, Jalanko H (2017) Anemia and low-grade inflammation in pediatric kidney transplant recipients. Pediatr Nephrol 32:347–358 [DOI] [PubMed] [Google Scholar]
- 10.Yorgin PD, Scandling JD, Belson A, Sanchez J, Alexander SR, Andreoni KA (2002) Late post- transplant anemia in adult renal transplant recipients. An under-recognized problem? Am J Transplant 2:429–435 [DOI] [PubMed] [Google Scholar]
- 11.KDIGO Anemia Work Group (2012) KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int (Suppl 2):279–335 [Google Scholar]
- 12.Sun CH, Ward HJ, Paul WL, Koyle MA, Yanagawa N, Lee DB (2018) Serum erythropoietin levels after renal transplantation. N Engl J Med 321:151–157 [DOI] [PubMed] [Google Scholar]
- 13.Khalil MAM, Khalil MAU, Khan TFT, Tan J (2018) Drug-Induced Hematological Cytopenia in Kidney Transplantation and the Challenges It Poses for Kidney Transplant Physicians. J Transplant 2018:9429265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yabu JM, Winkelmayer WC (2011) Posttransplantation anemia: mechanisms and management. Clin J Am Soc Nephrol 6:1794–1801 [DOI] [PubMed] [Google Scholar]
- 15.Schechter A, Gafter-Gvili A, Shepshelovich D, Rahamimov R, Gafter U, Mor E, Chagnac A, Rozen-Zvi B (2019) Posttransplantation anemia: causes, severity and their association with graft and patient survival. BMC Nephrol 20:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gafter-Gvili A, Cohen E, Avni T, Grossman A, Vidal L, Garty M, Leibovici L, Krause I (2015) Predicting the emergence of anemia – A large cohort study. Eur J Intern Med 26:338–343 [DOI] [PubMed] [Google Scholar]
- 17.Heinze G, Mitterbauer C, Regele H, Kramar R, Winkelmayer WC, Curhan GC, Oberbauer R (2006) Angiotensin-converting enzyme inhibitor or angiotensin II type 1 receptor antagonist therapy is associated with prolonged patient and graft survival after renal transplantation. J Am Soc Nephrol 17:889–899 [DOI] [PubMed] [Google Scholar]
- 18.Imoagene-Oyedeji AE, Rosas SE, Doyle AM, Goral S, Bloom RD (2006) Posttransplantation anemia at 12 months in kidney recipients treated with mycophenolate mofetil: risk factors and implications for mortality. J Am Soc Nephrol 17:3240–3247 [DOI] [PubMed] [Google Scholar]
- 19.Garrigue V, Szwarc I, Giral M, Soulillou JP, Legendre C, Kreis H, Kessler M, Ladriere M, Kamar N, Rostaing L, Morelon E, Buron F, Daguin P, Mourad G (2014) Influence of anemia on patient and graft survival after renal transplantation: results from the French DIVAT cohort. Transplantation 97:168–175 [DOI] [PubMed] [Google Scholar]
- 20.Chhabra D, Grafals M, Skaro AI, Parker M, Gallon L (2008) Impact of anemia after renal trans- plantation on patient and graft survival and on rate of acute rejection. Clin J Am Soc Nephrol 3:1168–1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ichimaru N, Obi Y, Nakazawa S, Yamanaka K, Kakuta Y, Abe T, Kaimori J-Y, Imamura R, Nonomura N, Moriyama T, Takahara S (2016) Post-Transplant Anemia Has Strong Influences on Renal and Patient Outcomes in Living Kidney Transplant Patients. Transplant Proc 48:878–883 [DOI] [PubMed] [Google Scholar]
- 22.Majernikova M, Rosenberger J, Prihodova L, Jarcuskova M, Roland R, Groothoff JW, van Dijk JP (2017) Posttransplant anemia as a prognostic factor of mortality in kidney transplant recipients. Biomed Res Int 2017:6987240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Molnar MZ, Czira M, Ambrus C, Szeifert L, Szentkiralyi A, Beko G, Rosivall L, Remport A, Novak M, Mucsi I (2007) Anemia is associated with mortality in kidney-transplanted patients – a prospective cohort study. Am J Transplant 7:818–824 [DOI] [PubMed] [Google Scholar]
- 24.Eisenga MF, Minovic I, Berger SP, Kootstra-Ros JE, van den Berg E, Riphangen IJ, Navis G, van der Meer P, Bakker SJL, Gaillard CAJM(2016) Iron deficiency, anemia, and mortality in renal transplant recipients. Transpl Int 29:1176–1183 [DOI] [PubMed] [Google Scholar]
- 25.Winkelmayer WC, Chandraker A, Alan Brookhart M, Kramar R, Sunder-Plassmann G (2006) A prospective study of anaemia and longterm outcomes in kidney transplant recipients. Nephrol Dial Transplant 21:3559–3566 [DOI] [PubMed] [Google Scholar]
- 26.Huang Z, Song T, Fu L, Rao Z, Zeng D, Qiu Y, Wang X, Xie L, Wei Q, Wang L, Lin T (2015) Post-renal transplantation anemia at 12 months: prevalence, risk factors, and impact on clinical outcomes. Int Urol Nephrol 47:1577–1585 [DOI] [PubMed] [Google Scholar]
- 27.Gheith O, Wafa E, Hassan N, Mostafa A, Sheashaa HA, Mahmoud K, Shokeir A, Ghoneim MA (2009) Does post-transplant anemia at 6 months affect long-term outcome of live-donor kidney transplantation? A single-center experience. Clin Exp Nephrol 13:361–366 [DOI] [PubMed] [Google Scholar]
- 28.Kamar N, Rostaing L, Ignace S, Villar E (2012) Impact of post-transplant anemia on patient and graft survival rates after kidney transplantation: a meta-analysis. Clin Transplant 26:461–469 [DOI] [PubMed] [Google Scholar]
- 29.Freiberg M, Chiurchiu C, Capra R, Eckhardt A, De La Fuente J, Douthat W, De Arteaga J, Massari PU (2013) [Associated factors and clinical implications of post transplant renal anemia]. Medicina (B Aires) 73:136–140 [PubMed] [Google Scholar]
- 30.Nangaku M (2006) Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J Am Soc Nephrol 17:17–25 [DOI] [PubMed] [Google Scholar]
- 31.Rigatto C, Parfrey P, Foley R, Negrijn C, Tribula C, Jeffery J (2002) Congestive heart failure in renal transplant recipients: risk factors, out- comes, and relationship with ischemic heart disease. J Am Soc Nephrol 13:1084–1090 [DOI] [PubMed] [Google Scholar]
- 32.Rigatto C, Foley R, Jeffery J, Negrijn C, Tribula C, Parfrey P (2003) Electrocardiographic left ventricular hypertrophy in renal transplant recipients: prognostic value and impact of blood pressure and anemia. J Am Soc Nephrol 14:462–468 [DOI] [PubMed] [Google Scholar]
- 33.El-Husseini AA, Aheashaa HA, Hassan NA, El-Demerdash FM, Sobh MA, Ghoneim MA (2004) Echocardiographic changes and risk factors for left ventricular hypertrophy in children and adolescents after renal transplantation. Pediatr Transplant 8:249–254 [DOI] [PubMed] [Google Scholar]
- 34.Kasiske BL, Vazquez MA, Harmon WE, Brown RS, Danovitch GM, Gaston RS, Roth D, Scandling JD, Singer GG (2000) Recommendations for the outpatient surveillance of renal transplant recipients. J Am Soc Nephrol 15:S1–S86 [PubMed] [Google Scholar]
- 35.Krause I, Davidovits M, Tamary H, Yuctis M, Dagan A (2016) Anemia and markers of erythropoiesis in pediatric kidney transplant recipients compared to children with chronic renal failure. Pediatr Transplant 20:958–962 [DOI] [PubMed] [Google Scholar]
- 36.Hindka A, Huynh D, Verghese PS (2021) Dapsone-induced methemoglobinemia in pediatrics post-renal transplant. Pediatr Transplant 25:e13921. [DOI] [PubMed] [Google Scholar]
- 37.Venkat Raman G, Sharman VL, Lee HA (1990) Azathioprine and allopurinol: a potentially dangerous combination. J Intern Med 228:69–71 [DOI] [PubMed] [Google Scholar]
- 38.Khameneh ZR, Sepehrvand N, Sohrabi V, Ghasemzadeh N (2014)The seroprevalence of Parvovirus B19 among kidney transplant recipients: a single-center study. Saudi J Kidney Dis Transpl 25:16–21 [DOI] [PubMed] [Google Scholar]
- 39.Lukaszewskia M, Kosiorowskab K, Banasikc M, Koscielska-Kasprzakc K, Krajewska M (2020) Assessment of hemoglobin levels in patients qualified for kideny transplantation in the perioperative period and its impact on the occurrence of delayed graft function. Transplant Proc 52:2059–2061 [DOI] [PubMed] [Google Scholar]
- 40.Richards KM, Spicer RA, Craig E, Kennedy SE (2018) Prevalence and predictors of blood transfusion after pediatric kidney transplantation. Pediatr Nephrol 33:2177–2184 [DOI] [PubMed] [Google Scholar]
- 41.Tsuchimoto A., Masutani K, Haruyama N, Nagata M, Noguchi H, Okabe Y, Kitada H, Tanaka M, Tsuruya K, Kitazono T (2013) Renal Interstitial Fibrosis in 0-hour biopsy as a predictor of post-transplant anemia. Am J Nephrol 38:267–274 [DOI] [PubMed] [Google Scholar]
- 42.EBPG Expert Group on Renal Transplantation (2002) European best practice guidelines for renal transplantation. Section IV: long-term management of the transplant recipient. IV.9.1. Haematological complications. Nephrol Dial Transplant 17(Suppl 4):48. [DOI] [PubMed] [Google Scholar]
- 43.KDOQI (2007) Clinical Practice Guideline and Clinical Practice Recommendations for anemia in chronic kidney disease: 2007 update of hemoglobin target. Am J Kidney Dis 50:471–530 [DOI] [PubMed] [Google Scholar]
- 44.Nampoory MRN, Johny KV, Al-Hilalin SMS, Kanagasabhapathy AS (1996) Erythropoietin deficiency and relative resistance cause anemia in post-renal transplant patients with normal renal function. Nephrol Dial Transplant 11:177–181 [PubMed] [Google Scholar]
- 45.Iorember F, Aviles D, Bagbola O (2020) Impact of immediate post-transplant parenteral iron therapy on the prevalence of anemia and short-term allograft function in a cohort of pediatric and adolescent renal transplant recipients. Pediatr Transplant 24:e13787. [DOI] [PubMed] [Google Scholar]
- 46.Mudge DW, Tan KS, Miles R, Johnson DW, Badve SV, Campbell SB, Isbel NM, van Eps CL, Hawley CM (2012) A randomized controlled trial of intravenous or oral iron for posttransplant anemia in kidney transplantation. Transplantation 93:822–826 [DOI] [PubMed] [Google Scholar]
- 47.Fishbane S (2003) Safety in iron management. Am J Kidney Dis 41:18–26 [DOI] [PubMed] [Google Scholar]
- 48.Morii M, Ueno K, Ogawa A (2000) Impairment of mycophenolate mofetil absorption by iron ion. Clin Pharmacol Ther 68:613–616 [DOI] [PubMed] [Google Scholar]
- 49.Mudge DW, Atcheson B, Taylor PJ (2004) The effect of oral iron administration on mycophenolate mofetil adsorption in renal transplant recipients: A randomized, controlled trial. Transplantation 77:206–209 [DOI] [PubMed] [Google Scholar]
- 50.Yorgin P (2005) Intravenous iron therapy in pediatric transplant recipients: What do we really know? Pediatr Transplant 9:1–3 [DOI] [PubMed] [Google Scholar]
- 51.Gillespie RS, Symons JM (2005) Sodium ferric gluconate for post-transplant anemia in pediatric and young adult renal transplant recipients. Pediatr Transplant 9:43–46 [DOI] [PubMed] [Google Scholar]
- 52.Stoffel NU, Zeder C, Brittenham GM, Moretti D, Zimmerman MB (2020) Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient women. Haematologica 105:1232–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kaundal R, Bhatia P, Jain A, Nampoothiri RV, Mishra K, Jandial A, Goni D, Sandal R, Jindal N, Meshram A, Sharma R, Khaire N, Singh C, Khadwal A, Prakash G, Das R, Varma N, Varma S, Malhotra P, Lad DP (2020) Randomized controlled trial of twice-daily versus alternate-day oral iron therapy in treatment of iron-deficiency anemia. Ann Hematol 99:57–63 [DOI] [PubMed] [Google Scholar]
- 54.O’Lone EL, Hodson EM, Nistor I, Bolignano D, Webster AC, Craig JC (2019) Parenteral versus oral iron therapy for adults and children with chronic kidney disease. Cochrane Database Syst Rev 2:CD007857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yorgin P (2005) Intravenous iron therapy in pediatric transplant recipients: what do we really know? Pediatr Transplant 9:1–3 [DOI] [PubMed] [Google Scholar]
- 56.Ishida JH, Marafino B, McCulloch CE, Dalrymple LS, Dudley RA, Grimes BA, Johansen KL (2015) Receipt of intravenous iron and clinical outcomes among hemodialysis patients hospitalized for infection. Clin J Am Soc Neph 10:1799–1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xin H, Ge YZ, Wu R, Yin Q, Zhou LH, Shen JW, Lu TZ, Hu ZK, Wang M, Zhou CC, Wu JP, Li WC, Zhu JG, Jia RP (2015) Effect of high-dose erythropoietin on graft function after kidney transplantation: a meta-analysis of randomized trial. Biomed Pharmacother 69:29–33 [DOI] [PubMed] [Google Scholar]
- 58.Briscoe DM, Pal S (2008) Assessing the vascular effects of early erythropoietin use in pediatric renal transplant recipients. Nat Clin Pract Nephrol 4:136–137 [DOI] [PubMed] [Google Scholar]
- 59.Heinze G, Kainz A, Hörl WH, Oberbauer R (2009) Mortality in renal transplant recipients given erythropoietins to increase haemoglobin concentration: cohort study. BMJ 339:b4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Choukroun G, Kamar N, Dussol B, Etienne I, Cassuto-Viguier E, Toupance O, Glowacki F, Moulin B, Lebranchu Y, Touchard G, Jaureguy M, Pallet N, Le Meur Y, Rostaing L, Martinez F; CAPRIT study investigators (2012) Correction of post kidney transplant anemia reduces progression of allograft nephropathy. J Am Soc Nephrol 23:360–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Purroy C, Fairchild RL, Tanaka T, Baldwin WM, Manrique J, Madsen JC, Colvin RB, Alessandrini A, Blazar BR, Fribourg M, Donadei C, Maggiore U, Heeger PS, Cravedi P (2017) Erythropoietin receptor-mediated molecular crosstalk promotes T cell immunoregulation and transplant survival. J Am Soc Nephrol 28:2377–2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nagarajan S, Mansfield E, Hsieh S, Liu R, Hsieh F, Li L, Salvatierra O Jr, Sarwal MM (2007) Transplant reno- vascular stenoses associated with early erythropoietin use. Clin Transplant 21:597–608 [DOI] [PubMed] [Google Scholar]
- 63.Aufricht C, Marik JL, Ettenger RB (1998) Subcutaneous recombinant human erythropoetin in chronic renal allograft dysfunction. Pediatr Nephrol 12:10–13 [DOI] [PubMed] [Google Scholar]
- 64.Wedekin M, Ehrich JHH, Pape L (2011) Effective treatment of anemia in pediatric kidney transplant recipients with methoxy polyethyleneglycol-epoetin beta. Pediatr Transplant 15:329–333 [DOI] [PubMed] [Google Scholar]
- 65.Lima PS, Campos ASD, Correa CS, Dias CJM, Mostarda CT, Amorim CEN, Garcia AMC (2018) Effects of chronic physical activity on glomerular filtration rate, creatinine and the markers of anemia of kidney transplantation patients. Transplant Proc 50:746–749 [DOI] [PubMed] [Google Scholar]
- 66.Painter PL, Hector L, Ray K, Lynes L, Dibble S, Paul SM, Tomlanovich SL, Ascher NL (2002) A randomized trial of exercise training after renal transplantation. Transplantation 74:42–48 [DOI] [PubMed] [Google Scholar]
- 67.Calella P, Hernandez-Sanchez S, Garofalo C, Ruiz JR, Carrero JJ, Bellizzi V (2019) Exercise training in kidney transplant recipients: a systemic review. J Nephrol 32:567–579 [DOI] [PubMed] [Google Scholar]
- 68.Verghese P, Gillingham K, Matas A, Chinnakotla S, Chavers B (2016) Post-transplant blood transfusions and pediatric renal allograft outcomes. Pediatr Transplant 20:939–945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ferrandiz I, Congy-Jolivet N, Del Bello A, Debiol B, Trébern-Launay K, Esposito L, Milongo D, Dörr G, Rostaing L, Kamar N (2016) Impact of early blood transfusion after kidney transplantation on the incidence of donor-specific anti-HLA antibodies. Am J Transplant 16:2661–2669 [DOI] [PubMed] [Google Scholar]


