Abstract
Background
Severe aortic valve stenosis inhibits renal perfusion, thereby potentially worsening renal function, in particular in elderly patients most often assigned to transcatheter aortic valve implantation (TAVI). Pre-TAVI diagnostics and the procedure itself may adversely impact renal function, however renal perfusion and function may also improve post-procedure. This study aimed to clarify the impact of TAVI planning and procedure on kidney function
Methods
In this retrospective study, kidney function of patients who underwent transfemoral TAVI at a tertiary university hospital between 2016 and 2019 was analyzed. The present study investigated kidney function at baseline, after computed tomography (CT) was performed for evaluation of TAVI, after TAVI, at discharge and at follow-up.
Results
Among 366 patients, the prevalence of acute kidney injury (AKI) was 14.5% after TAVI. Independent predictors of AKI were arterial hypertension, baseline creatinine, AKI post CT and coronary intervention during pre-procedural diagnostics. At discharge and follow-up, 2.1% and 3.4%, respectively had sustained relevant impairment of kidney function (defined as creatinine/baseline creatinine > 1.5 or renal replacement therapy). Patients with known chronic kidney disease showed no higher rates of short- and long-term impairment, but higher rates of improvement of renal function after TAVI.
Conclusions
In most cases TAVI does not worsen renal function. A sustained impairment after TAVI was found in only a few cases. This was independent of reduced baseline kidney function. Transfemoral TAVI can thus be planned and performed even in patients with higher stages of chronic kidney disease.
Keywords: kidney function, transcatheter aortic valve implantation, computed tomography, acute kidney failure
Introduction
Chronic kidney disease (CKD) is common and associated with an increased risk of cardiovascular events [1]. Besides coronary artery disease, valvular heart disease also affects survival in these patients. Prevalence of aortic valve stenosis is higher and is associated with significantly higher mortality [2].
Transcatheter aortic valve implantation (TAVI) is an established minimally invasive method for treating patients with severe aortic stenosis [3]. While patients with CKD are at increased risk for short- and long-term mortality among high-surgical-risk patients undergoing TAVI, there is no association between CKD and mortality in low- to intermediate-risk patients [4]. Publications analyzing the risk of acute kidney injury (AKI) after TAVI are also inconclusive [5–9]. Since publications focus on AKI after TAVI, little is known about the impact of aortic valve stenosis, the total workflow of pre-procedural TAVI diagnostics and the procedure itself on short- and long-term renal function. On the one hand, the need for contrast agent or complications during TAVI procedure may lead to impairment of kidney function; on the other hand, hemodynamic improvement of kidney perfusion after TAVI may even improve renal function.
Apart from the periinterventional risk, preprocedural diagnostics are also under discussion as possibly impairing kidney function: First, contrast enhanced computed tomography (CT) with contrast agent application is used to evaluate anatomy of the aortic valve and aorta, providing valuable information for pre-procedural planning [10]. Second, coronary angiography is indicated for the assessment of coronary artery disease [11]. Interestingly, there is little literature analyzing CKD and AKI after CT prior to TAVI [12], while no data exists on the impact of AKI on long-term renal function after TAVI. However, it is a frequent clinical question whether a TAVI can safely be planned and performed in patients at risk for impaired renal function.
In order to clarify the impact of TAVI on renal function we investigated acute and chronic renal failure over the complete TAVI process, including pre-procedural diagnostics and the intervention itself. Furthermore, risk factors for the development of renal failure are identified.
Methods
Study population
Medical records of patients who underwent CT for evaluation of TAVI, and who underwent transfemoral TAVI (TF-TAVI) at a tertiary university hospital between 2016 and 2019 were retrospectively analyzed. Only patients with severe aortic valve stenosis were included for further analyses.
The indication for TAVI treatment was made by an interdisciplinary heart team consisting of cardiologists, heart surgeons, and anesthesiologists. Analysis was blinded to patient identity and was covered by an ethics approval committee (Ethics Committee of Albert-Ludwigs University of Freiburg, file number EK 29/11).
Pre-procedural screening and intervention
All contrast-enhanced CT examinations were performed on a second-generation dual-source CT scanner (DSCT, Somatom Definition Flash, Siemens Healthineers) according to current guidelines. A scout view of thorax and abdomen was obtained to plan data acquisitions. Coronary angiography was routinely performed before TAVI. If TAVI was the only possible therapeutic intervention, coronary angiography could be performed during the TAVI procedure. Percutaneous coronary intervention (PCI) was performed, if necessary based on current guidelines of the European Society of Cardiology. For TAVI, valvuloplasty was left to the discretion of the treating physician. Several types of valves were individually selected (Edwards Sapien 3/XT, Medtronic Evolute R/Pro, DirectFlow, Symetis Acurate neo) and implanted by an experienced team of interventional cardiologists, cardiac surgeons, and anesthesiologists.
Renal function
Baseline renal function was calculated as estimated glomerular filtration rate (eGFR) of mean creatinine levels before the first application of contrast agent using the Modification of Diet in Renal Disease (MDRD) GFR equation. An eGFR < 60 mL/min (CKD stage ≥ III Kidney Disease: Improving Global Outcomes [KDIGO]) was considered as relevant CKD. AKI was defined as increase of serum creatinine of ≥ 0.3 mg/dL or to ≥ 1.5 times baseline, according to the acute kidney injury network criteria [13]. Creatinine levels were measured at the discretion of the treating physician and considered to be associated with the procedure if the increase occurred within 7 days. If TAVI was performed earlier than 7 days after the last contrast agent application, creatinine levels were distributed manually to TAVI or pre-TAVI diagnostics, depending on the clinical setting.
Data collection
All patients who underwent transfemoral TAVI were identified. By manual case by case review, patients were excluded if they met one or more of the exclusion criteria, which were chronic renal replacement therapy (RRT), shock or cardiopulmonary resuscitation in short period to diagnostics/TAVI, and conversion to surgical valve replacement. Since patients with transplanted kidneys were very rare (2/368), we decided to exclude this patient collective as well. All outcome variables were evaluated by manual search of medical and patient records.
Statistical analysis
For data analysis, SPSS (version 26, IBM Statistics) and Prism (version 5, GraphPad) were employed. For statistical analysis, the students t-test, the Fisher exact test and the χ2 test were used when appropriate, and a p value of < 0.05 was considered statistically significant. Multivariate regression binary analysis was performed for predictors of AKI and impairment of kidney function (p < 0.05) to check for interactions and to estimate the magnitude of the predictor. A possible collinearity may be present concerning AKI post CT and AKI post TAVI. Results are given as odds ratio ([OR], 95% confidence interval [CI]). Again, a p-value of < 0.05 was considered statistically significant. Data are given as number (%), mean ± standard deviation or OR with 95% CI if not stated otherwise. For missing variables in multivariate binary analysis, multiple imputation was applied. All analyses were exploratory in nature. As a result, p-values and 95% CIs were not corrected for multiple comparisons and inferences drawn from them may not be reproducible.
Results
Patient characteristics
Within the observed time period, TF-TAVI was performed in 394 patients. A total of 28 patients were excluded from analysis (15 on chronic RRT; 2 with transplanted kidneys; 5 with shock or cardiopulmonary rescuscitation in short period to diagnostics/TAVI, 5 with conversion to surgical valve replacement, 1 patient with missing data after TAVI). Therefore, 366 patients could be evaluated. Of these, 37 patients had no creatinine measurements after CT, mainly because of early hospital discharge (Suppl. Fig. 1).
Mean age was 81.1 ± 5.9 years, 200 (54.6%) patients were female. Baseline creatinine was 1.16 ± 0.44 mg/dL. A total of 176 (48.1%) patients had relevant CKD with an eGFR < 60 mL/min (Table 1).
Table 1.
Baseline characteristics of all patients and all patients with or without acute kidney injury (AKI) after transcatheter aortic valve implantation (TAVI).
| All patients (n = 366) | No AKI (n = 313) | AKI (n = 53) | P | |
|---|---|---|---|---|
| Age | 82.1 ± 5.9 | 81.8 ± 5.9 | 84.1 ± 5.4 | 0.007 |
| Female | 200 (54.6%) | 169 (54.0%) | 31 (58.5%) | 0.543 |
| Weight [kg] | 73.2 ± 15.3 | 73.8 ± 15.6 | 70.2 ± 13.0 | 0.118 |
| Comorbidities | ||||
| STS-Score [%] | 7.4 ± 4.6 | 7.0 ± 4.5 | 9.8 ± 4.3 | 0.001 |
| NYHA class | 2.3 ± 1.2 | 2.3 ± 1.2 | 2.5 ± 1.2 | 0.192 |
| CCS class | 0.9 ± 1.3 | 0.8 ± 1.2 | 1.2 ± 1.4 | 0.095 |
| Atherosclerosis | 26 (73%) | 224 (71.6%) | 43 (81.1%) | 0.147 |
| Atrial fibrillation | 156 (42.6%) | 129 (41.2%) | 27 (50.9%) | 0.185 |
| Hypertension | 300 (82%) | 250 (79.9%) | 50 (94.3%) | 0.011 |
| Diabetes mellitus | 107 (29.2%) | 94 (30%) | 13 (24.5%) | 0.415 |
| Smoking | 74 (20.2%) | 65 (20.8%) | 9 (17%) | 0.526 |
| Syncope | 62 (16.9%) | 53 (17.2%) | 8 (17%) | 0.976 |
| History of stroke/cerebral bleeding | 56 (15.3%) | 48 (15.3%) | 8 (15.1%) | 0.964 |
| Pulmonary disease | 75 (20.5%) | 65 (20.8%) | 10 (18.9%) | 0.751 |
| Malignancy | 110 (30.1%) | 90 (28.8%) | 20 (37.7%) | 0.187 |
| Alcohol abuse | 9 (2.5%) | 8 (2.6%) | 1 (1.9%) | 1.000 |
| ACEI/sartan | 263 (71.9%) | 220 (73.8%) | 43 (81.1%) | 0.258 |
| Metformin | 5 (13.9%) | 47 (15%) | 4 (7.5%) | 0.147 |
| Baseline characteristics | ||||
| Mean AV gradient [mmHg] | 42.2 ± 13.9 | 42.5 ± 13.8 | 40.1 ± 14.8 | 0.250 |
| AV opening area [cm2] | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.735 |
| Mitral valve insufficiency | 1.3 ± 0.6 | 1.2 ± 0.5 | 1.4 ± 0.6 | 0.157 |
| Ejection fraction [%] | 50.8 ± 10.3 | 51.0 ± 10.0 | 49.6 ± 12.1 | 0.357 |
| Baseline-creatinine [mg/dL] | 1.16 ± 0.44 | 1.10 ± 0.39 | 1.48 ± 0.55 | 0.001 |
| eGFR [mL/min] | 62.8 ± 22.7 | 65.4 ± 22.3 | 47.5 ± 19.1 | 0.001 |
| eGFR < 60 mL/min | 176 (48.1%) | 139 (44.4%) | 37 (69.8%) | 0.001 |
| Procedural characteristics | ||||
| AKI post CT diagnostics | 22 (6.7%) | 13 (4.7%) | 9 (17.3%) | 0.003 |
| PCI | 177 (46.0%) | 144 (46.0%) | 33 (62.3%) | 0.029 |
| CT TAVI in different stays | 112 (30.6%) | 97 (31%) | 15 (28.3%) | 0.694 |
| Coronary angiography on TAVI day | 125 (23.2%) | 100 (31.9%) | 25 (47.2%) | 0.031 |
| Contrast agent TAVI [mL] | 222.7 ± 88.1 | 219.9 ± 86.5 | 244.2 ± 95.3 | 0.055 |
| General anaesthesia | 86 (23.5%) | 68 (21.7%) | 18 (34%) | 0.052 |
| CRP max [mg/dL] | 61.7 ± 60.3 | 54.3 ± 53.5 | 105.2 ± 77.8 | 0.001 |
| Renal replacement therapy after TAVI | 3 (0.8%) | 0 (0%) | 3 (5.7%) | 0.003 |
| Mortality | 8 (2.2%) | 3 (1%) | 5 (9.4%) | 0.002 |
| Hospital stay [days] | 13.9 ± 7.1 | 12.8 ± 5.7 | 20.4 ± 10.8 | 0.001 |
| ICU stay [days] | 2.7 ± 2.3 | 2.5 ± 2.2 | 3.4 ± 2.7 | 0.010 |
| Pacemaker implantation necessary | 83 (22.7%) | 64 (20.4%) | 19 (35.8%) | 0.013 |
Data are given as mean ± standard deviation or number of patients (percent of all patients in group). ACEI — angiotensin converting enzyme inhibitor; AV — aortic valve; CCS — Canadian Cardiovascular Society; CRP — C-reactive protein; CT — computed tomography; eGFR — estimated glomerular filtration ratio; ICU — intensive care unit; NYHA — New York Heart Association; PCI — percutaneous coronary intervention; STS-Score — Society of Thoracic Surgeons — Score for mortality
Renal function during TAVI diagnostics, TAVI and after TAVI
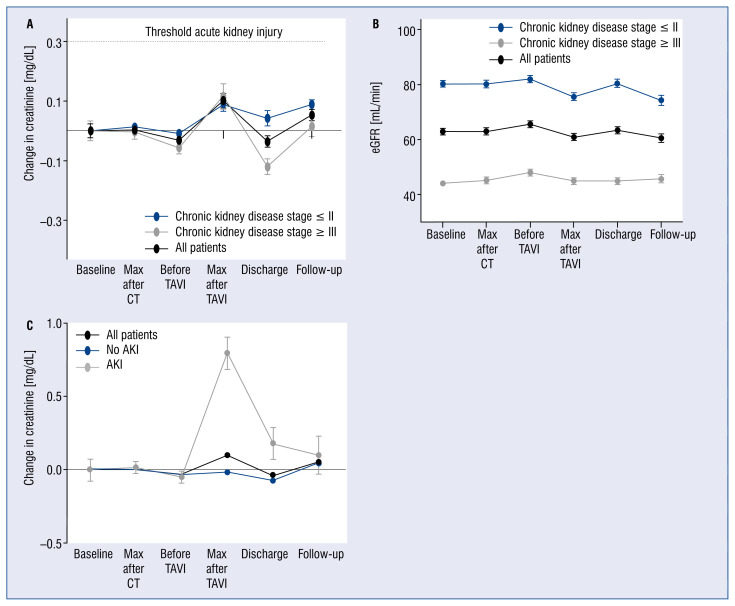
Creatinine levels were analyzed during the complete workflow including baseline-creatinine, creatinine after CT, before/after TAVI, at discharge, and in follow up examinations (161 ± 87 days). In relation to baseline creatinine, the mean creatinine after CT minimally deteriorated (+0.004 ± 0.230 mg/dL) and peaked after TAVI (+0.101 ± 0.455 mg/dL). At discharge, creatinine marginally improved (–0.03 ± 0.358 mg/dL) in all patients. The group with higher CKD stages showed a significant improvement in renal function compared to patients with lower CKD stages (–0.121 ± 0.346 mg/dL vs. +0.042 ± 0.352 mg/dL, p < 0.001). Analyzing the long-term data at follow up (n = 183, 1 patient with RRT, 88 with initial CKD ≥ III), creatinine-levels in relation to baseline-creatinine increased slightly in both CKD ≥ III and CKD ≤ II patients (+0.014 ± 0.310 mg/dL vs. +0.088 ± 0.152 mg/dL, p = 0.039), but were under the threshold for AKI of +0.3 mg/dL increase of creatinine (Fig. 1A). Levels of eGFR were stable throughout the whole procedure (Fig. 1B).
Figure 1.
Kidney function during pre-procedural planning, transcatheter aortic valve implantation (TAVI) and after TAVI. Differences to baseline-creatinine (A) and estimated glomerular filtration ratio (eGFR; mL/min) (B) are shown in all patients and patients with and without pre-existing chronic kidney disease. Creatinine differences are shown in patients developing an acute kidney injury (AKI) after TAVI (C). Data are given as mean ± standard error of the mean; CT — computed tomography.
Patients developing AKI are at risk for long-term kidney failure. Therefore, we extracted patients with AKI post TAVI (n = 53, 14.5%). Naturally, patients with AKI post TAVI showed their highest creatinine levels after TAVI (in total 2.28 ± 1.06 mg/dL vs. 1.09 ± 0.38 mg/dL; in relation to baseline creatinine +0.80 ± 0.81 mg/dL vs. −0.02 ± 0.19 mg/dL). Creatinine levels improved and showed slightly impaired levels at discharge in relation to baseline creatinine (+0.18 ± 0.78 mg/dL vs. −0.07 ± 0.20 mg/dL), with stable levels on follow up examinations (‘n’ at follow up = 183) (Fig. 1C).
Risk factors for AKI after CT
In order to identify patients at risk for AKI during TAVI planning, creatinine levels and risk factors after CT were analyzed. Of all 329 patients with documented creatinine levels after CT, 22 (6.7%) patients had AKI after CT. All patients had KDIGO stage I of AKI and no RRT was necessary after CT. CKD was more present in patients with AKI (77.3% vs. 22.7%, p = 0.006). No correlation was identified between amount of contrast agent and AKI (AKI 113.7 ± 4.4 mL vs. no AKI 113.2 ± 4.2 mL; p = 0.586). No independent predictors of AKI post CT were identified with a multivariate binary logistic regression analysis, whereas baseline creatinine showed a positive trend (OR 2.13 [0.92–4.90], p = 0.076) (Suppl. Fig. 2).
Risk factors for AKI after TAVI
The TAVI procedure itself may worsen renal function due to hemodynamic impairment or contrast agent. After TAVI, 53 patients suffered from AKI (14.5%): 44 had KDIGO stage I (83% of patients with AKI), 6 (11%) had KDIGO stage II and 3 (5%) had KDIGO stage III and needed RRT. Patients with AKI were older, had higher creatinine levels and more often CKD stage ≥ III. Mortality was higher in patients with AKI (9.4% vs. 1.0%, p = 0.002; Table 1).
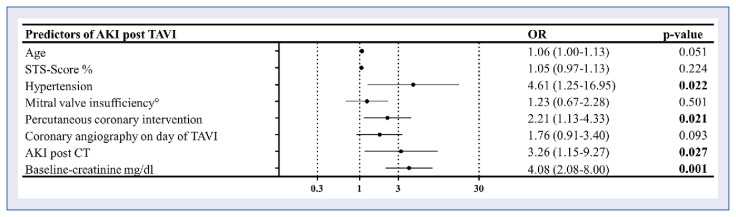
Univariate (Suppl. Table 1) and multivariate binary logistic regression analysis to identify independent predictors of AKI after TAVI were performed. Independent predictors of AKI post TAVI were arterial hypertension, baseline-creatinine and coronary intervention during pre-procedural diagnostics. Patients with AKI after CT showed higher risk for AKI after TAVI as well (Fig. 2).
Figure 2.
Multivariate analysis of risk factors for acute kidney injury (AKI) after transcatheter aortic valve implantation (TAVI). Predictors of impaired kidney function after TAVI. Figure shows multivariate logistic regression analysis with odds ratio (OR) (95% confidence interval) of different predictors for AKI after TAVI. OR > 1 marks positive predictors, OR < 1 marks negative predictors; CT — computed tomography; STS-Score — Society of Thoracic Surgeons — Score for mortality.
Incidence and risk factors for renal impairment at discharge
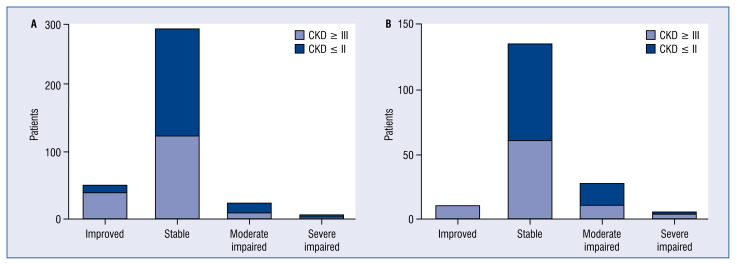
Testing the hypothesis that renal function could recover, creatinine levels were analyzed during follow up by creating three groups with different changes in short-term kidney function: One group with improved kidney function (creatinine < < 0.8 times baseline), one group with stable kidney function (creatinine 0.8–1.2 times baseline) and one group with impaired kidney function (creatinine > > 1.2 times baseline). The group with impairment of kidney function was further divided into moderate and severe impairment (moderate: creatinine 1.2–1.5 times baseline; severe: creatinine > 1.5 times baseline or RRT). Most patients had stable or improved kidney function independent of the CKD stage (89.5% in CKD ≤ II, 92.6% in CKD stage ≥ III). While 33 (9%) patients had impaired kidney function at discharge, only 8 (2.1%) patients showed severe impairment of kidney function (Fig. 3A). In patients with CKD stage ≥ III, impairment of kidney function did not occur more often than in patients with CKD stage ≤ II (7.4% vs. 10.5%, p = 0.295). Patients with CKD stage ≥ III showed higher rates of improved kidney function (22.7% vs. 5.8%, p < 0.001).
Figure 3.
Long-time renal impairment. Patients were divided in four groups with different changes in renal function: One group with improved renal function (creatinine < 0.8 times baseline), one group with stable renal function (creatinine 0.8–1.2 times baseline), one group with moderately impaired renal function (creatinine 1.2–1.5 times baseline) and one group with severely impaired renal function (creatinine > 1.5 times baseline or renal replacement therapy); A. The proportion of patients at discharge; B. The proportion at follow-up (161 ± 87 days); CKD — chronic kidney disease.
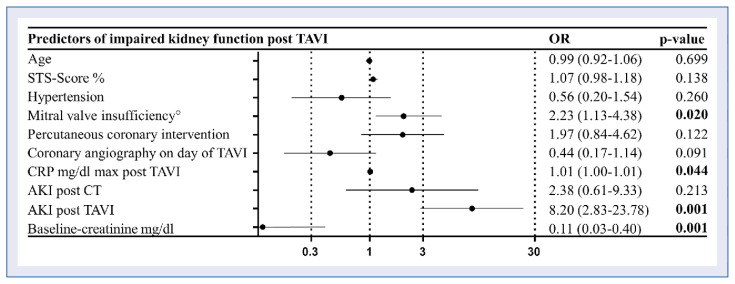
Univariate (Suppl. Table 2) and multivariate binary logistic regression was performed to identify independent predictors of impaired kidney function after TAVI. Multivariate logistic regression showed that baseline-creatinine is no predictor of impaired kidney function after TAVI. Higher baseline creatinine rather negatively correlates to impaired kidney function. In contrast, AKI post TAVI, C-reactive protein (CRP, mg/dL) and grade of mitral valve insufficiency before TAVI were positive predictors (Fig. 4).
Figure 4.
Mulitvariate analysis of risk factors for short term renal function. This figure shows multivariate logistic regression analysis with odds ratio (OR) (95% confidence interval) of different predictors for impaired short-term renal function after transcatheter aortic valve implantation (TAVI). OR > 1 marks positive predictors, OR < 1 marks negative predictors; AKI — acute kidney injury; CRP — C-reactive protein; CT — computed tomography; STS-Score — Society of Thoracic Surgeons — Score for mortality.
Incidence and risk factors for renal impairment at follow up
At follow up, 19.1% of all patients had impaired renal function, including 3.4% patients with severe impaired kidney function with no differences concerning CKD stage (Fig. 3B). Improvement of kidney function occurred more often in patients with CKD stage ≥ III (p < 0.001).
Discussion
Renal function during the complete TAVI workflow including pre-procedural diagnostics, TAVI itself, renal function at discharge and at postinterventional follow up were analyzed. We were able to demonstrate several points: First, we showed that AKI after CT for TAVI evaluation is rare and leads only to moderate stages of AKI. Second, we showed that renal function after AKI recovers almost fully in most cases. Third, we demonstrated that patients with CKD showed no higher rates of short- and longterm impairment, but higher rates of improvement of renal function after TAVI.
AKI post CT
There is only little data concerning AKI after intravenous contrast agent injection for CT in patients with severe aortic stenosis. Jochheim et al. [12] showed an incidence of AKI of 10.5%. Risk for AKI was increased only in patients with impaired baseline renal function who received volumes > 90 mL [12]. The incidence we demonstrated is lower (6.7%) and is in the range of recently published studies on patients undergoing CT for other reasons (~6.4%) [14]. We were not able to identify patients with an increased risk for AKI, although baseline creatinine showed a positive trend. Additionally, no correlation to the amount of injected contrast agent was seen, which agrees with the data of a meta-analysis using propensity score matching, which showed no difference in rates of AKI, RRT and mortality between patients receiving iodinated intravenous contrast agent and those receiving no contrast agent [15]. Most importantly, shown herein, is that the stage of AKI is low and no RRT was needed after CT. Furthermore, AKI after CT is no independent predictor for impaired kidney function after TAVI. Since mortality of severe aortic valve stenosis is high, a CT for planning TAVI should not be generally rejected due to concerns of renal impairment.
AKI post TAVI
Acute kidney injury is a frequent complication after TAVI due to impaired hemodynamics during implantation and the use of a contrast agent. Incidence ranges from 8.3% to 58% [16]. This high range might partly be explained by different study populations and different definitions of AKI. A multicenter study showed an incidence of 20.7% with a reduced incidence at increasing stages (stage I: 15%: stage II or III: 6%) [17]. By using the updated Valve Academic Research Consortium (VARC)-2 criteria, recommending that the timing for the diagnosis of AKI should be 7 days [18], we report an incidence of AKI of 14.5% with very low incidences of higher stages (stage II or III: 2.5%) and high rates of stage I (12.0%), which are not associated with an increased 1-year mortality according to previous studies [19].
Studies analyzing risk factors for AKI post TAVI are heterogenous. Referring to preexisting CKD, there are publications proposing an association with baseline-creatinine levels and AKI post TAVI [5–7, 9], while others did not find any association between patients with or without CKD [8]. In the present analysis, a high correlation of baseline-creatinine and AKI post TAVI was reported. AKI post CT was also identified as an independent predictor of AKI post TAVI. According to available research, this study is the first to report this correlation. However, at follow-up patients suffering from AKI during TAVI workflow showed only slightly impaired levels.
Renal function after TAVI
Although there is a lot of data on AKI after TAVI, less is known about the effect of the treatment of aortic valve stenosis on short- and long-term kidney function for the entire TAVI package, including pre-procedural diagnostics and the procedure itself. Herein, was hypothesized that better perfusion after TAVI could improve the renal function and compensate for negative effects such as contrast agent application, rapid pacing or intraoperative hypotension during TAVI. Indeed, there was an improvement in short-term renal function of 13.9%, while observing an impaired renal function in only 9% of all patients. Also, relevant impairment of renal function (2.1%, including patients with RRT) or necessity of RRT (0.8%) were very low. Interestingly, the presence or absence of higher stages of CKD were no predictors of impaired renal function, which did not worsen more often in patients with higher CKD stages. On the contrary, a negative correlation of short-term impairment of kidney function and baseline-creatinine was noted. This is concordant with a recent publication reporting improved renal function 1 year after TAVI for patients with moderate-to-severe CKD [20]. Others have found similar results, with 1 recent study showing in a logistic regression analysis that lower baseline renal function was predictive for improved renal function after TAVI [7]. Although the study included more than 1,500 patients, the definition of improved renal function used, defined as a positive change 48 hours after TAVI, was very short-termed. Nevertheless, ratios of improved short-term kidney function in the CKD group were similar to the present ones. Consequently, the findings herein, support the findings of these publications.
Interestingly, higher CRP-levels were also associated with impaired kidney function at discharge. It was assumed that this was related to an increased rate of kidney failure in the context of potential infections or also possibly to the use of nephrotoxic antibiotics. Consequently, an appropriate effort should be made to avoid postinterventional infections.
Referring to the higher ratios of impaired kidney function at follow up, a correlation to TAVI is not assumed, since the impairing effect of TAVI (i.e., complications) should naturally occur before discharge. We rather propose the natural impairment of kidney function in our aged patient cohort.
Due to the small number of patients with renal replacement therapy after TAVI (0.8%), the impact of CKD could not be analyzed. Data in the United Kingdom TAVI Registry showed that the risk of new dialysis requirement after TAVI was independently associated with lower baseline kidney function [21]. Nevertheless the present study shows that concerns of impairing kidney function in CKD patients after TAVI should not be grounds for refusal of TAVI.
Limitations of the study
When discussing the results presented in the present analysis, some limitations have to be considered. This is single-center retrospective data and results have to be considered hypothesis-generating, and should be confirmed in larger multi-center trials.
In clinical routine, commonly there is a great diversity in the diagnostic sequence. Sometimes a patient undergoes CT, coronary angiography and PCI before TAVI in the same stay, whereas in the case of staged procedures, there could be no exposition with contrast agent prior to TAVI. The distribution of these patients could have impacted the homogeneity of the study population. Due to the study setting, measurement of creatinine levels was at the discretion of the treating physician and not performed daily. Consequently, an underreported incidence or an underestimated stage of AKI cannot be excluded. Since the last measured creatinine was analyzed before discharge, the rate of impaired kidney function may be overestimated, since creatinine after AKI could further decrease. We can rule out an underestimation, since patients with increasing creatinine are not discharged in our hospital. Additionally, the cohort of patients was reduced at follow up, complicating interpretation of the follow up analysis.
Clinical data was based on medical reports. Since structured clinical interviews were not used, some variables are likely to be underreported.
Conclusions
The present study suggests that relevant impairment of renal function after TAVI is rare, and occurs independently of reduced renal function. Additionally, the data suggests that TAVI can improve renal function in patients with CKD. This is clinically important, since it could help facilitate decision-making for the TAVI intervention, and improve the risk assessment in these patients. Furthermore, it was demonstrated that CT in pre-procedural diagnostics does not impair renal function.
Supplementary Information
Footnotes
Funding
The article processing charge was funded by the Baden-Württemberg Ministry of Science, Research and Art and the University of Freiburg via the Open Access Publishing funding program.
Conflict of interest: None declared
References
- 1.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Samad Z, Sivak JA, Phelan M, et al. Prevalence and outcomes of left-sided valvular heart disease associated with chronic kidney disease. J Am Heart Assoc. 2017;6(10) doi: 10.1161/JAHA.117.006044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leon M, Smith C, Mack M, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2016;374(17):1609–1620. doi: 10.1056/nejmoa1514616.. [DOI] [PubMed] [Google Scholar]
- 4.Makki N, Lilly SM. Advanced chronic kidney disease: Relationship to outcomes post-TAVR, a meta-analysis. Clin Cardiol. 2018;41(8):1091–1096. doi: 10.1002/clc.22993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Attard S, Buttigieg J, Galea S, et al. The incidence, predictors, and prognosis of acute kidney injury after transcatheter aortic valve implantation. Clin Nephrol. 2018;90(6):373–379. doi: 10.5414/CN109544. [DOI] [PubMed] [Google Scholar]
- 6.Langfritz M, Shahin M, Nietlispach F, et al. Baseline Predictors of Renal Failure in Transcatheter Aortic Valve Implantation. J Invasive Cardiol. 2019;31(10):E289–E297. [PubMed] [Google Scholar]
- 7.Azarbal A, Malenka DJ, Huang YL, et al. Recovery of Kidney Dysfunction After Transcatheter Aortic Valve Implantation (from the Northern New England Cardiovascular Disease Study Group) Am J Cardiol. 2019;123(3):426–433. doi: 10.1016/j.amjcard.2018.10.042. [DOI] [PubMed] [Google Scholar]
- 8.Wessely M, Rau S, Lange P, et al. Chronic kidney disease is not associated with a higher risk for mortality or acute kidney injury in transcatheter aortic valve implantation. Nephrol Dial Transplant. 2012;27(9):3502–3508. doi: 10.1093/ndt/gfs102.. [DOI] [PubMed] [Google Scholar]
- 9.Alassar A, Roy D, Abdulkareem N, et al. Acute kidney injury after transcatheter aortic valve implantation: incidence, risk factors, and prognostic effects. Innovations (Phila) 2012;7(6):389–393. doi: 10.1097/IMI.0b013e3182814e43. [DOI] [PubMed] [Google Scholar]
- 10.Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739–91. doi: 10.1093/eurheartj/ehx391. [DOI] [PubMed] [Google Scholar]
- 11.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2014;35(37):2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 12.Jochheim D, Schneider VS, Schwarz F, et al. Contrast-induced acute kidney injury after computed tomography prior to transcatheter aortic valve implantation. Clin Radiol. 2014;69(10):1034–1038. doi: 10.1016/j.crad.2014.05.106. [DOI] [PubMed] [Google Scholar]
- 13.Section 2: AKI Definition. Kidney Int Suppl 2011. 2012;2(1):19–36. doi: 10.1038/kisup.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonald JS, McDonald RJ, Comin J, et al. Frequency of acute kidney injury following intravenous contrast medium administration: a systematic review and meta-analysis. Radiology. 2013;267(1):119–128. doi: 10.1148/radiol.12121460. [DOI] [PubMed] [Google Scholar]
- 15.McDonald JS, McDonald RJ, Lieske JC, et al. Risk of Acute Kidney Injury, Dialysis, and Mortality in Patients With Chronic Kidney Disease After Intravenous Contrast Material Exposure. Mayo Clin Proc. 2015;90(8):1046–1053. doi: 10.1016/j.may-ocp.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scherner M, Wahlers T. Acute kidney injury after transcatheter aortic valve implantation. J Thorac Dis. 2015;7(9):1527–1535. doi: 10.3978/j.issn.2072-1439.2015.06.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nuis RJ, Rodés-Cabau J, Sinning JM, et al. Blood transfusion and the risk of acute kidney injury after transcatheter aortic valve implantation. Circ Cardiovasc Interv. 2012;5(5):680–688. doi: 10.1161/CIRCINTERVENTIONS.112.971291. [DOI] [PubMed] [Google Scholar]
- 18.Kappetein A, Head S, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document†. Eur Heart J. 2012;33(19):2403–2418. doi: 10.1093/eurheartj/ehs255.. [DOI] [PubMed] [Google Scholar]
- 19.Seiffert M, Schnabel R, Conradi L, et al. Predictors and outcomes after transcatheter aortic valve implantation using different approaches according to the valve academic research consortium definitions. Catheter Cardiovasc Interv. 2013;82(4):640–652. doi: 10.1002/ccd.24751. [DOI] [PubMed] [Google Scholar]
- 20.Calça R, Teles RC, Branco P, et al. Impact of transcatheter aortic valve implantation on kidney function. Arq Bras Cardiol. 2019;113(6):1104–1111. doi: 10.36660/abc.20180356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferro CJ, Law JP, Doshi SN, et al. Dialysis following transcatheter aortic valve replacement: risk factors and outcomes: an analysis from the UK TAVI (Transcatheter Aortic Valve Implantation) Registry. JACC Cardiovasc Interv. 2017;10(20):2040–2047. doi: 10.1016/j.jcin.2017.05.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.