Abstract
The e-cigarette (EC) epidemic began in the United States (US) in 2007; since 2014 EC is the most commonly used form of tobacco. However, the mental health implications of vaping are grossly unknown. The aim of this umbrella review is to provide astate-of-the-art summary of existing research concerning vaping and mental health conditions in children. Following the PRISMA Statement 2020 guidelines, a systematic search was conducted across PubMed, Cochrane Library, and Google Scholar up to April 15th, 2022 to locate relevant studies. The Joana Briggs Institute (JBI) methodology for umbrella reviews and quality appraisal tool was utilized. Six studies, pooling a total of 846,510 adolescents aged 21 years or below, were included by collating 85 primary clinical studies. Of these, 58.8% of the primary clinical studies originated in the US, with 4.7% from Canada, South Korea, and the United Kingdom each; 3.5% each from England and Taiwan; 2.4% each from Australia, France, Hawaii, Mexico, and Russia; and 1.2% each from Denmark, Greece, Hong Kong, Iceland, New Zealand, Poland, and Switzerland. Overall, significant associations were found between mental health outcomes, including depression and suicidality, among current EC users and those who had ever used EC. Compared to adolescents who had never used EC, both depression and anxiety were reportedly higher among EC users. Impulsive behaviors, reported as impulsivity, were also found to be correlated with the adoption of EC use. However, there is a lack of evidence regarding the impact of EC use on mental health outcomes in children. This umbrella review highlights the urgent need to further explore the effects of current EC use from a psychiatric and public health perspective.
Keywords: Vaping, e-cigarette, mental health, children, adolescents, depression, suicidality, anxiety, impulsivity
Introduction
The E-cigarette (EC) epidemic among youth began with the distribution of ECs in the United States in 2007. Since 2014, these products have become the most commonly used tobacco form. 1 While a shift from a combustible cigarette (CC) use to EC use has been an area of key progress, the tobacco sphere continues to penetrate society. EC is designed to deliver flavors, nicotine, and other chemicals delivered via inhaled aerosol. 1 Products range from e-cigarettes, vaping pens, tank systems, e-hookahs, and electronic nicotine delivery systems (ENDS); they may appear as regular cigarettes, pipes or cigars, USBs, and pens. 2 Most of the EC in use have a heating system, batteries, and a liquid-holding tank. 2 The use of EC is referred to as vaping and these systems can be utilized to deliver marijuana, other drugs. 2 “Puff Bar (26.1%), Vuse (10.8%), SMOK (9.6%), JUUL (5.7%), and Suorin (2.3%)” were the most commonly used EC brands among current high school students, as reported by the CDC and FDA. 3 The nation’s youth e-cigarette epidemic is largely attributed to flavored tobacco products including menthol and other flavors. In the US, 27.5% of high school students use EC 4 ; the 3 largest market users originate from the US, the United Kingdom, and Japan. The global EC market was valued at $20.4 billion, in 2021—this is expected to grow to $30 billion by 2027. 5 Alarmingly, EC use among the youth rose by 1800% between the years 2011 and 2019. 4 Three in 4 users aged between 15 and 21 years are unaware that EC contains nicotine. 4
The mental health implications of vaping in children are largely unknown, although data may associate the changes with those seen with tobacco cigarettes. Mental health concerns among children related to vaping, other than addiction have been largely neglected. 6 While smoking CC has been an established risk factor for adverse mental health, the reasons for the underemphasis of EC as a potential determinant of mental health are unknown. 7 Smokers may also view EC products as a modality to improve dysphoric symptoms, without recognizing that smoking cessation may lead to the improvement of said symptoms. 6 The aim of this umbrella review is to provide an updated summary of the existing research syntheses related to vaping and mental health conditions in children, focusing on the mental health consequences of vaping in this group.
Methods
Search strategy
This umbrella review was conducted adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines and the Joana Briggs Institute (JBI) methodology for umbrella reviews.8,9 We searched PubMed, Cochrane library, and Google Scholar to locate the studies. The search terms are enlisted in Supplemental Materials. All databases and additional sources were searched from inception until April 15, 2022. All citations were stored in EndNote X9 (Clarivate Analytics).
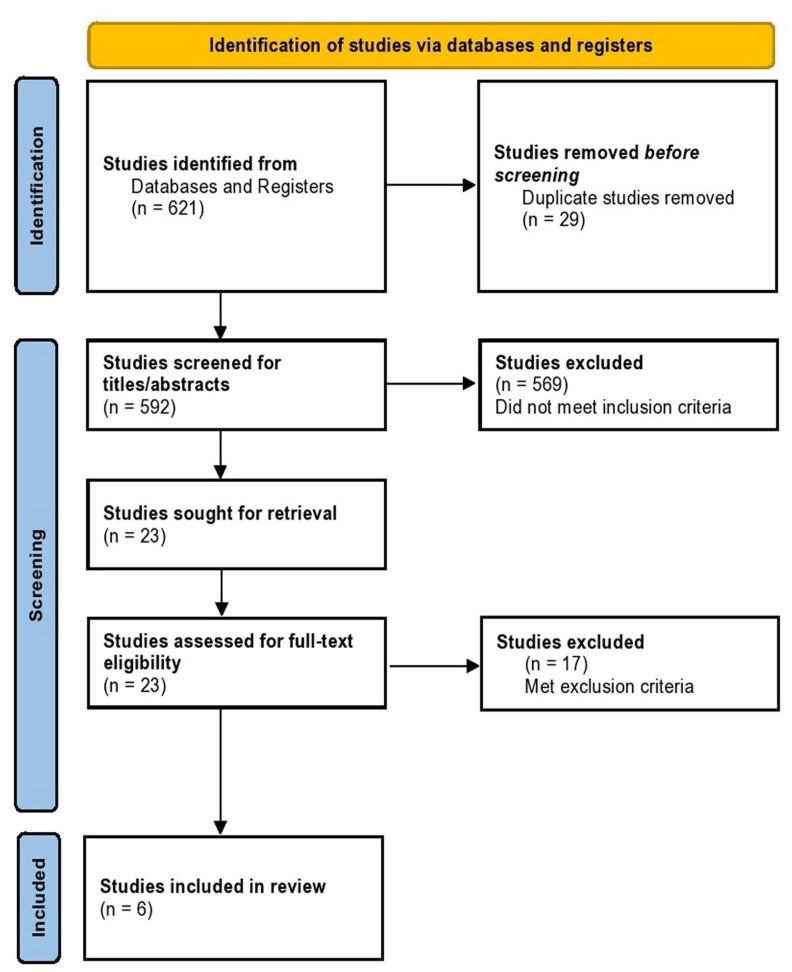
The PRISMA flowchart is depicted in Figure 1. A total of 621 studies were identified through the databases and other sources searching. Twenty-nine duplicates were removed before screening; 592 studies were screened for titles/abstracts. Of these, 23 were assessed for full-text screening. Post-full-text screening, 6 reviews were included in this umbrella review. The excluded studies (n = 17) are enlisted in Table 1 with reasons.
Figure 1.
PRISMA flowchart depicting the study selection process.
Table 1.
Full-text studies excluded in this umbrella review.
| Authors | Studies/reports included | Screening result | Reason for exclusion | DOI |
|---|---|---|---|---|
| Lim (2022) 10 | 17 | Excluded | Reports of epidemiological studies that share the global prevalence of cannabis vaping, not related to mental health outcomes | https://doi.org/10.1001/jamapediatrics.2021.4102 |
| Notley (2021) 11 | 60 | Excluded | Focused on interest and enjoyment in flavors, with no mental health indicators/sequelae | https://doi.org/10.1111/add.15723 |
| Bozier (2020) 12 | 225 | Excluded | Focus on cardiopulmonary, general health, and oral manifestations | https://doi.org/10.1016/j.chest.2019.12.042 |
| Selph (2020) 13 | 30 | Excluded | Focus on quitting interventions | https://doi.org/10.1001/jama.2020.3332 |
| Gonsalves (2020) 14 | 23 | Excluded | Focus on pulmonary outcomes only | https://doi.org/10.1016/j.jpeds.2020.09.040 |
| Pericot-Valverde (2018) 15 | 66 | Excluded | No demaracation of adult populations and pediatric populations aged 18-21 years | https://doi.org/10.1016%2Fj.addbeh.2018.04.024 |
| Glasser (2017) 16 | 686 | Excluded | Focus on ENDS and general outcomes | https://doi.org/10.1016%2Fj.amepre.2016.10.036 |
| Garcia (2020) 17 | 19 | Excluded | Focus on autonomic cardiovascular effects | https://doi.org/10.1007%2Fs10286-020-00683-4 |
| O’Brien (2021) 18 | 21 | Excluded | Focus on causal and temporal relationships between e-cigarette and tobacco use | https://doi.org/10.1186/s12889-021-10935-1 |
| Gentry (2019) 19 | 9 | Excluded | Focus on the adult population | https://doi.org/10.1093%2Fntr%2Fnty054 |
| Lee (2020) 20 | 35 | Excluded | Focus on marketing, product and design | https://doi.org/10.1001%2Fjamapediatrics.2020.0259 |
| Smith (2021) 21 | 15 | Excluded | Focus on social aspects and norms | https://doi.org/10.1016/j.drugpo.2021.103227 |
| Kinouani (2019) 22 | 6 | Excluded | Focus on motivations | https://doi.org/10.1080/08897077.2019.1671937 |
| Tzortzi (2020) 23 | 133 | Excluded | Reports of suicidal ideation in adults >21 years | https://doi.org/10.3390/ijerph17072248 |
| Fluharty (2017) 24 | 148 | Excluded | Lack of <21 years findings | https://doi.org/10.1093/ntr/ntw140 |
| Gogliettino (2016) 25 | 5 | Excluded | Lack of focus on mental health outcomes, but addresses white matter development that is linked to symptoms of depression. Age group until 28 years. | https://doi.org/10.1016%2Fj.drugalcdep.2016.02.015 |
| Underner (2021) 26 | NA | Excluded | Non-English language text | https://doi.org/10.1016/j.encep.2020.11.008 |
Inclusion and exclusion criteria
This umbrella review included a systematic review and meta-analytical studies. These studies included national sample studies, cohorts, case series, and case reports as well. Children/adolescents aged 21 years or less that were exposed to electronic cigarettes/vaping were included. Mental health consequences were enlisted wherever available. No date restrictions were applied; however, non-English articles were excluded. In addition, studies that did not analyze the <21 years age group were excluded even if they reported on EC and mental health outcomes. A manual search of the bibliography of all screened studies was conducted.
Data extraction and synthesis
Two reviewers (AMK and ZS) identified the articles for inclusion by screening titles and abstracts, followed by a full-text review. Any discrepancies were resolved by active discussion between the 2 reviewers or with a third person (SA) to reach a consensus. The data extraction tool was adapted from the JBI data extraction tool used for research syntheses. The 2 authors extracted data into the following domains: the PICO framework, year of publication, type of review, number of primary clinical studies included, sample size, locations, and key findings of EC and mental health outcomes. The findings based on the included reviews were further segregated (study-level) by providing a synthesis of the primary clinical studies among included reviews. The findings were reported on prevalence rates (proportion, percentage, OR/aOR, or other measures), and in most cases, 95% confidence intervals (CI) were reported.
Methodological quality
The JBI critical appraisal tool was used to assess the quality of included reviews. The JBI critical appraisal checklist for systematic reviews and research synthesis checklist was used. Two reviewers (AMK and ZS) evaluated all 6 of the included reviews. A consensus was reached for the final quality ratings. The articles were grouped under the following: low (0-4), medium (5-7), and high-quality (8-10) studies.
Additionally, studies that were eligible for inclusion underwent quality appraisal using the AMSTAR-2 checklist. While there are many variants to appraise systematic reviews/meta-analyses, the AMSTAR-2 checklist is the most commonly used one to assess the methodological quality of systematic reviews, with and without a meta-analysis of randomized and non-randomized studies. 27 This checklist comprises 16 questions and consists of 7 domains that can determine the validity of included reviews and conclusions. The critical domains include the presence of an a-priori review protocol, adequate literature search, and exclusion criteria justification of individual studies. assessment of the risk of bias, the appropriateness of statistical methods, sources of publication bias if a meta-analysis is conducted and considerations of potential biases during result interpretation.
This umbrella review was registered with PROSPERO: CRD42022312130. No funding was obtained for this study.
Results
Characteristics of the included reviews
Summary findings of included reviews are enlisted in Table 2. The study populations had diverse characteristics. The sample size of the included studies was 846 510. While studies also focused on young adults, we only included data from adolescents aged 21 years and below. Racial and ethnic minorities were represented across the studies. The participants were recruited from many resources including national sample data, in-schools, and longitudinal and cross-sectional surveys. The included reviews (n = 6) originated from both high-income and low and middle-income countries.28-33 The number of primary studies in the included reviews under the umbrella framework was 85. The primary studies across all reviews originated from the US (n = 50, 58.8%), Canada/South Korea/UK each (n = 4, 4.7%), England/Taiwan each (n = 3, 3.5%), Australia/France/Hawaii/Mexico/Russia each (n = 2, 2.4%), Denmark/Greece/Hong Kong/Iceland/New Zealand/Poland/Switzerland each (n = 1, 1.2%). All 6 reviews were published between 2016 and 2021. Two of the 6 studies were scored as high-quality reviews. Whereas, the other 4 reviews were classified as medium-quality reviews (Table 2).
Table 2.
Characteristics and key findings of included systematic reviews and meta-analyses.
| No | Authors | Country of the study population | Number of primary studies included; type of review | Included sample characteristics | Participants | Exposure(s) | Comparator(s)/control(s) | Outcome(s) | Prevalence rates of vaping and mental health findings | JBI appraisal score |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Becker et al 28 | Seventeen studies were from the US, 4 from South Korea, 2 from England, and 1 was from Taiwan | 24; Systematic Review | Adolescents aged 12-18 years | (i) Adolescents and young adults in the 12-26 age group; (ii) Mental health assessed by transdiagnostic concepts linked with adolescent psychopathology (ie, reward responsiveness, executive function, and impulsivity), psychometric assessments of mental health conditions (ie, depression, anxiety, and ADHD)/mental illness diagnosis as reported by the self; (iii) Assessed for EC use | EC use (ie, e-cigarette, vape pod, vaping pod, JUUL, and ENDS) with any liquid (ie, cannabis, nicotine, or flavoring). | No history of EC use | Psychiatric comorbidities (ie, depression, anxiety, ADHD, PTSD, bipolar disorder, schizophrenia, oppositional defiant disorder, and conduct disorder) or transdiagnostic constructs (ie, working memory, executive function, impulsivity, and attachment) assessed by (i) reported diagnosis, (ii) psychometric scales, and (iii) individuals recruited from mental health treatment programs | Internalizing symptoms (composite) were associated with EC use among adolescents in the PATH study and among at-risk US high school students. Depression was associated with EC use in 4 national cohorts (Korea, United States, and Taiwan) and in a California based study, with positive associations and 1 cohort showing bidirectional relationship. Anxiety was reported in 1 cross-sectional study as measured with scales for several anxiety subtypes, finding EC-only use less strongly related to anxiety as compared to CC-only use; lifetime EC-only users had higher levels of panic disorders as compared to those that abstained from nicotine, but had lower levels of GAD, social phobia, panic, anxiety sensitivity, and OCD than only CC users. Suicidality was weakly linked to EC use with 4 national cross-sectional studies in the US and Korea; current EC use was linked to suicidal plans, ideation, and attempts. Eating disorders and link to EC use was significant in 1 South Korean study, with current EC and female lifetime users presenting with higher rates of unhealthy weight control behaviors. CC users had similar associations. Externalizing disorders (composite) were significant in the PATH study associated with lifetime EC user. ADHD symptoms, as reported in 2 studies, could be predicted by subsequent EC use but not CC use. Conduct disorder and delinquency was reported in 3 articles and was related to subsequent EC use; baseline rule-breaking tendency independently predicted EC use. Perceived stress was reported in a longitudinal cohort employing teenagers and was associated with past-month and lifetime EC use. |
9 |
| 2. | Chan et al 29 | Five from the US, 3 from the UK, 1 each from Canada, Mexico and Taiwan | 11; systematic review and meta-analysis | Non-smokers aged <18 years at baseline | General adolescent population (aged 18 years and below), who have never smoked at baseline | Vaping or EC use, with no history of cigarette use (history or co-user cigarette use at baseline was excluded) | No EC use at baseline | Smoking initiation at subsequent follow-up (those that tried but did not become an “ever smoker” were excluded) | Significant longitudinal associations between vaping and smoking were found (OR = 2.93, 95% CI = 3.63-12.31). Confounder analysis determined that family and peer influence were key determinants of smoking. The social developmental model and social ecological models were applied yielding an E-value of 2.9 for adolescent vaping impact on smoking initiation. |
7 |
| 3. | Rothrock et al 30 | Fourteen studies were from the US, 2 from South Korea and 1 each from Australia, Canada, England, France, Hawaii, Hong Kong, Iceland, Mexico, Poland, Russia, Switzerland, and Taiwan | 28; systematic review and meta-analysis | Adolescents aged 10-19 years | Adolescents as defined by World Health Organization (10-19 years) or high school age or younger) who used EC and who did not smoke EC | Vaping/alcohol use | EC users vs. non-EC users | Rates of alcohol use and binge drinking/drunkenness | EC users had a higher risk for any alcohol use compared to non-EC users (OR = 6.62, 95% CI = 5.67-7.72). EC users also had a higher risk for binge drinking/drunkenness compared to non-EC users (OR = 6.73, 95% CI = 4.5-10.07). |
8 |
| 4. | Soneji et al 32 | Three studies were from the US and 1 was from Hawaii | 4; Systematic review and meta-analysis | Adolescents aged 14-20 years | Adolescents | Adolescents who were never cigarette smokers at baseline or were EC users | EC users vs. non-EC users | Among never cigarette smokers at baseline, cigarette smoking initiation at follow-up; in baseline none-past 30-day cigarette smokers who were 30-day EC users, past 30-day cigarette smoking at follow-up was determine | Cigarette smoking initiation among never cigarette smokers and ever EC users at baseline compared to never EC users at baseline revealed the following mean values: (aOR = 3.89, 95% CI = 2.91-4.88). Psychosocial symptoms (depression, impulsivity; and rebelliousness), Behavioral symptoms (substance use, delinquent behavior) and other symptoms (cigarette use at home, peer smoking; binge drinking, marijuana use) were reported as covariates. |
6 |
| 5. | Chadi et al 31 | Seven were from the UK, 2 from Canada, and 1 each from Russia, New Zealand, Greece, France, and Australia | 14; systematic review and meta-analysis | Individuals aged <21 years | Children and adolescents between 10 and 21 years | ENDS use | Without ENDS use | EC use associated to marijuana use | Adolescents and young children showed stronger associations between EC use and marijuana use (aOR = 4.29, 95% CI = 3.14-5.87) as compared to the adult population (aOR = 2.3, 95% CI = 1.4-3.69) | 6 |
| 6. | Hua and Talbot 33 | Four were from the US, 1 each from the UK and Denmark | 6; systematic review of case reports | Children aged <21 years | Neonatal and pediatric individuals reporting symptoms of EC side effects and diagnosed by HCPs | EC use or exposure | None | Associatte EC use to health outcomes and related sub-categories | Suicide attempt was reported in one 13-year-old male who ingested 3 mL of EC refill liquid; ease of availability and less dose for toxicity were causes for nicotine poisoning in the case. Mechanical injuries in an 18-year-old male with ADHD occurred due to spontaneous explosion of EC battery. General findings due to EC use pertained to patients with opioid addiction, those abusing other drugs. |
5 |
Umbrella review findings
Becker et al 28 included 221 691 adolescents aged 12 to 18. Of those, 28 239 (12.7%) used EC. Among the sample that used EC, 16 333 (57.8%) were lifetime and ever EC users. A 1522 (5.4%) were current users (used in the previous month to the previous year). On noting EC and CC (lifetime) use, 6170 (21.8%) adolescents were documented, whereas 1236 (4.4%) used EC and CC in the previous month to the previous year. Finally, EC and cannabis/marijuana/other illicit drugs were abused by 2978 (10.5%) adolescents.
Chan et al 29 included 11 primary clinical studies of non-smokers aged <18 years at baseline. Meta-analytical findings suggested that longitudinal associations between initiating vaping and smoking were found (OR = 2.93, 95% CI = 3.63-12.31). Of the 11 studies that Chan et al pooled, 7 of them (N = 24 971) examined associations between lifetime vaping at enrollment and smoking initiation during the follow-up period. Key findings comprised of the following. Chan et al reported that EC use led to 6 times higher odds of commencing CC use as compared to never EC users. Further, low-age (12-15 years) youths had higher risks of CC initiation and use. Young never smokers (11- to 18-year-olds) were more likely to try CC if they tried EC in the past. Chen and colleagues also found a prospective association between every use of EC and smoking initiation among Asian populations. Ever-use of EC was robustly associated with CC initiation but with a modest increase in CC use. The review also ascertained that the youth population (aged 11-18 years) in Great Britain had the association of ever-EC use to CC initiation. Adolescents who use EC are more likely to begin smoking cigarettes. Chen’s examination of past-month smoking and vaping initiation pooled in 17 564 children. 29 On this front, regional sample findings determined EC use associations with CC smoking behaviors, including both initiation and follow-up. US statewide sample estimates determined that EC use was ascertained as an independent risk factor for future smoking among non-smokers/past smokers’ youth. Lifetime vaping was also associated with past 6-month vaping and smoking initiation. Whereas ever EC users at baseline were more likely to initiate combustible tobacco use in the next year.
Rothrock et al 30 included a total of 28 primary clinical studies with 458 357 adolescents aged 10 to 19 years. of these participants, 146 059 were binge drinkers and 373 150 individuals had drunkenness. 30 In their analysis, Rothrock et al 30 pooled 373 150 adolescents. They determined that EC users had higher risks for any alcohol use as compared to non-EC users (OR = 6.62, 95% CI = 5.67-7.72). Furthermore, EC users had higher risks for drunkenness/binge drinking as compared to non-EC users (OR = 6.73, 95% CI = 4.5-10.07). 30
In their review, Soneji et al 32 included 4 primary clinical studies with adolescents aged 14-20 years pooling in 10 705 adolescents. Based on findings from prospective longitudinal panel data in a national sample study, Soneji found that the youth recent vapers and non-CC smokers had nearly 5 times the risk of reporting cigarette smoking at follow-up (RR = 4.78); recent vapers were twice likely to report smoking (RR = 2.15); vaping did not predict smoking cessation. 34 The authors also reported that the adjusted prevalence of current EC or CC use in 2014 was 13.7%, which is higher than the 9% prevalence determined in 2004 before EC was introduced. Never smokers and those who used EC were more likely to smoke CC (OR = 2.87, 95% CI = 2.03-4.05); moreover, the uptake of CC among EC never and recent EC users was predicted by rebelliousness and perception of EC being healthier alternatives. Past-6-month use of any combustible tobacco was more frequent in baseline EC users (30.7%) as compared to never users (8.1%); on adjusting for interpersonal and environmental risk factors for smoking, the likelihood of CC use was computed (OR = 2.73, 95% CI = 2-3.73). Overall, Soneji and colleagues found that EC ever users as compared to non-users were more likely to initiate CC users over the next year.
Hua and Talbot 33 reported a total of 6 cases of children with vaping-related effects. Among these cases, there are many causes of vaping-related effects including suicide attempts, and mechanical injuries related to ADHD. 33 General EC findings were related to opioid addiction and the abuse of other drugs that led to suicide attempts and poisonings caused by intentional abuse/misuse of EC. 33
Chadi et al 31 reported a total of 14 primary studies assessing the associations between marijuana and ENDS use in 130 780 children with a median/mean age of fewer than 18 years. In summary, the authors assessed marijuana use among those aged 18 or below, which was higher (aOR = 4.29, 95% CI = 3.14-5.87) as compared to those older than age 18 (aOR = 2.3, 95% CI = 1.4-3.79. EC users were more likely to be older, Caucasian, male, and with poorer academic scores as compared to non-EC users. Generally, EC users were also more likely to report smoking CC, drinking, seeking sensation, and abusing drugs. Moreover, Increased EC use was linked to higher odds of current marijuana use (aOR = 1.7, 95% CI = 1.3-2) and heavy marijuana use (aOR = 1.6, 95% CI = 1.2-2.2). the authors also found that user groups including EC and alcohol/other drug use had similar behavioral health behaviors and physical health. Of note, EC-only users had lesser mental health symptoms and less alcohol/other drug use as compared to CC-only and EC/CC users. Dual (CC and EC) users were more likely to use cannabis as compared to EC-only users with increased frequency of use (1-2 times a week: aOR = 2.04, 95% CI = 1.26-3.31; 3-6 times a week: aOR = 4.8, 95% CI = 2.72-8.46, daily: aOR = 10.67, 95% CI = 5.56-20.49. EC users were more likely than CC users to report blunt (aOR = 1.81, 95% CI = 1.21-2.71) and hookah use (aOR = 3.12, 95% CI = 1.9-5.13), however, no differences were reported in smokeless tobacco, cigar, or marijuana use. EC experimentation was higher among those who smoked 10 or more CC (OR = 5.67, 95% CI = 3.11-10.34) and among ever-CC users (OR = 4.46, 95% CI = 2.81-7.09). With increased student age, the likelihood to consume EC reduced, whereas students with more spending money were more likely to use EC. The most frequent reasons for trying EC a curiosity (64.5%) and being recommended to try (24.2%); current CC smokers tried EC to quit CC smoking (16.6%), whereas other users tried EC for harm reduction (27.8%). 31
Mental Health Findings
Depression
Based on our umbrella synthesis, 2 of the 6 studies reported depression findings associated with vaping. Beckeret al 28 and Chadi et al 31 included a total of 10 primary studies in their review. Becker et al’s key findings were overall significant with depressive symptoms, with similar reporting seen by Chadi et al. 31
Becker et al found that EC-only uses compared to no use were associated with depressive symptoms (aOR = 1.37, 95% CI = 1.19-1.57. However, there were also findings of no significance for medium/high depressive symptoms in children who exclusively used EC use. When correlating baseline depressive symptoms with odds of commencing EC use, there was an associative link reported (aOR = 1.015, 95% CI = 1.003-1.023); moreover, sustained EC use compared to no use led to increases in depressive symptoms over time (b = 1.272); sustained EC users also had a significant association between past 30-day EC use and depressive symptoms (b = 1.611). Chadi et al 31 found that never vs. ever-tobacco users “Center for Epidemiologic Studies Depression Scale (CES-D)” values were 13.31 (10.99) versus 16.88 (12.45) in mean (SD) respectively; this means that ever-tobacco users had higher levels of depression as measured (P < .001). CES-D values were lower in EC users as compared to CC users though; EC = 2.85 (1.4) and CC-only = 3.19 (1.54). Among EC users, Chadi et al found inconclusive findings for outcomes of stress-coping including decision-making coping (OR = 0.99, 95% CI = 0.9-1.09), anger coping (OR = 0.96, 95% CI = 0.9-1.03), and social-support coping (OR = 0.94, 95% CI = 0.9-0.99); the multivariate model examined associations between these variables and lifetime EC use among schoolers, which did not have any relevant shifts.
On the whole, Becker et al reported largely significant findings of EC users with higher measures of depression, sadness, and hopelessness compared to non-users, however, the levels were lower than CC/dual users. Additionally, depressive symptoms (aOR= 1.21) were associated with the past 30-day use of vaporized cannabis. When comparing both reviews reporting depressive findings, there was only one case where no significant links were found between EC use and medium/high depression. Whereas, all other counts were suggestive of a cause-and-effect, and correlative shift in mental health outcomes.
Suicidality
Suicidality was reported in 2 of the 6 included reviews by Becker et al and Hua. In total, the 2 reviews pooled 4 primary studies and 1 case report. While Becker et al reported an associative relationship between suicidality with EC use, Hua and Talbot 33 reported a case of accidental ingestion of EC refill liquid by a 13-year-old male, unrelated to psychiatric overlays.
Becker et al’s review, pooled in 105 815 adolescents, where past-12-month EC-only use was associated with suicidal ideation (aOR = 1.23), cumulative higher rates of suicidal planning (χ2 = 17, P < .001), and suicide attempts (χ2 = 9.64, P = .002). However, Becker et al also reviewed studies where suicidal ideation had insignificant links with EC use in the past 12 months. On logistic regression analysis, suicidal ideation (aOR = 1.58, 95% CI = 1.31-1.89), suicidal plans (aOR = 2.44, 95% CI = 1.94-3.08), suicide attempts (aOR=2.44, 95% CI=1.85-2.44), and serious suicide attempts (aOR = 3.09, 95% CI = 1.51-6.32) were observed at higher likelihoods compared to non-EC users, which is a key finding. EC past-30-day use was, however, associated with suicide ideation (aOR = 2.49, 95% CI = 1.82-3.42), suicide planning (aOR = 4.63, 95% CI=3.22-6.67), and suicide attempts (aOR = 6.17, 95% CI = 6.17, 95% CI = 4.13-9.24). Odds ratios for suicide plans were higher in females, which is a singular finding reported by Becker et al The suicide attempt reported by Hua and Talbot 33 by a 13-year-old male was unlinked with the psychiatric manifestation of EC use. However, the ease of availability and the low dose required for toxicity was the key cause of nicotine poisoning in the child.
Impulsivity
Impulsivity was reported by Becker et al, Chadi et al, and Hua et al; 3 of the 6 reviews addressed the manifestation of vaping use. Becker et al 28 reviewed outcomes of 10 697 adolescents where behavioral impulsivity was associated with earlier age of EC onset, which also predicted frequency of EC use (B = -0.25, P = .02); EC-only (OR = 1.26, 95% CI = 1.18-1.35) users and EC/CC (OR range = 1.45-1.77) users had higher levels of impulsivity as compared to never users. In simpler terms, impulsivity was increased in EC users compared to never users. Another key finding reported by Becker was that impulsivity was associated with past-30-day vaporized cannabis use (aOR=1.37). In the review by Hua and Talbot, 33 there was no psychiatric linkage to impulsivity; 1 case of mechanical injuries in an 18-year-old male with ADHD was reported; the injury occurred due to a spontaneous explosion of an EC battery. Now, Chadi et al 31 included 2668 participants in their review; based on the TCI impulsivity scale, never versus ever tobacco users reported as mean (SD) were 2.34 (1.49) and 2.8 (1.37) (P = .004) respectively. Our key learnings from both Becker and Chadi’s reviews are that TCI and regression findings suggest that impulsivity is higher for EC-only and EC/CC users as compared to never users.
Anxiety disorder
Anxiety disorder was only reported in 2 of the 6 reviews included in this umbrella review. Becker et al and Chadi et al 31 pooled a total of 3 primary clinical studies. Anxiety was a common denominator among both reviews.
For instance, Becker et al analyzed 4075 participants. They found that 19.9% of adolescents using nicotine EC had anxiety and were doing illicit substance vaping (aOR = 1.96, 95% CI = 1.18-3.14). Contrary to popular belief, Becker et al additionally found that CC users compared to EC users had lower levels of anxiety sensitivity. Chadi et al 31 synthesized 2488 participants where anxiety symptoms were reported in non-users (2.83 (1.47)), EC-only users (2.74 (1.38)), and CC-only users (3.16 (1.69)); the highest ratio was present in CC-only users, followed by non-users, and thereby EC-users. To sum up, Chadi et al reported higher anxiety symptoms in CC users compared to EC users, and data was uncertain on non-users compared to EC users’ anxiety symptoms.
Critical appraisal includes studies
In accordance with the AMSTAR-2 Checklist findings, we assessed findings across 16 domains (Table 3). When assessing if the included reviews included PICO in the research question, 3 reviews [Becker et al 28 , Rothrock et al, 30 and Chadi et al 31 ] included them, whereas Chan et al 29 and Soneji et al 32 partially did; Hua and Talbot 33 did not include a PICO framework with the research question. On assessing whether methods were established prior to conducting the reviews, Becker et al, 28 Chan et al, 29 and Rothrock et al 30 fully established them, Chadi et al 31 and Soneji et al 32 established them partially and Hua and Talbot 33 not at all. The study design selection and literature search strategy were fully established and reported in all reviews excluding Hua’s and Talbot 33 where it was partially stated.
Table 3.
Quality appraisal of the included reviews using the AMSTAR-2 tool.
| Authors | Research question included PICO | Review methods established prior to review | Explanation of study design selection | Comprehensive literature search strategy | Study selection performed in duplicate | Data extraction performed in duplicate | List of excluded studies with justification | Describe studies in adequate detail | Satisfactory technique for assessing RoB | Report sources of funding |
|---|---|---|---|---|---|---|---|---|---|---|
| Beckeret al 11 | ||||||||||
| Chan et al 12 | ||||||||||
| Rothrock et al 13 | ||||||||||
| Chadi et al 14 | ||||||||||
| Soneji et al 15 | ||||||||||
| Hua and Talbot 16 |
Abbreviation: PICO, population or participants, and conditions of interest; Interventions or exposures; Comparisons or control groups; Outcomes of interest.
Green = yes; red = no; and orange = partial yes.
Table 3.
Quality appraisal of the included reviews using the AMSTAR-2 tool (continued).
| Authors | Use appropriate methods for statistical combination of results (for meta-analysis) | Assess potential impact of RoB in individual studies on the results (for meta-analysis) | Account for RoB in individual studies when interpreting results | Explanation for and discussion of heterogeneity in results | Investigate publication bias and discuss impact (for quantitative synthesis) | Reported conflict of interest |
|---|---|---|---|---|---|---|
| Becker et al 11 | ||||||
| Chan et al 12 | ||||||
| Rothrock et al 13 | ||||||
| Chadi et al 14 | ||||||
| Soneji et al 15 | ||||||
| Hua and Talbot 16 |
Abbreviation: RoB, risk of bias.
Green = yes; red = no; and orange = partial yes.
The study selection and data extraction were performed in duplicates in all reviews fully excluding Chan’s et al 29 and Hua’s and Talbot 33 reviews where no pairing was established. Only Becker et al 28 and Rothrock et al 30 partially justified the list of studies they excluded whereas all other reviews did not justify exclusion. All reviews included in this umbrella review describe the primary studies they included in adequate detail. On assessing whether a satisfactory technique was applied to assess for risk of bias, all reviews fully satisfied the criteria excluding Soneji et al 32 and Hua and Talbot 33 who did not assess for biases. All included reviews reported sources of funding and conflicts of interest (Table 3).
On assessing whether the included reviews used appropriate statistical combinations for the meta-analysis, Becker et al 28 and Hua and Talbot 33 did not, while Chan et al 29 , Rothrock et al, 30 Chadi et al, 31 and Soneji et al 32 used appropriate methods for statistical testing. Considering the potential impact of risk of bias in individual studies and accounting for bias when interpreting results, Chan et al, 29 Rothrock et al, 30 , and Chadi et al 31 fully accounted for them, whereas Becker et al, 28 Soneji et al, 32 and Hua and Talbot 33 did not at all. When we appraised the reviews for explanation and discussion of the heterogeneity of results, only Chadi et al 31 fully accounted for them, whereas Becker et al, 28 Chan et al, 29 and Rothrock et al 30 partially did so, and Soneji et al 32 and Hua and Talbot 33 did not at all. Finally, on appraising if the sources of publication bias and discussions of impact were made, only Chan et al 29 and Rothrock et al 30 fully accounted for them, whereas Becker et al, 28 Chadi et al, 31 and Hua and Talbot 33 did not account for publication bias; Soneji et al 32 reported and discussed biases partially (Table 3).
Discussion
In this umbrella review, the primary studies originated largely from the US (58.8%), followed by Canada, South Korea, and the United Kingdom (4.7% each).28–33 The 6 reviews were published between 2016 and 2021. The key mental health findings of our umbrella review included (i) depression, (ii) suicidality, (iii) impulsivity, and (iv) anxiety disorder. A cross-sectional analysis of a representative sample in the US found that former and current electronic cigarette (EC) users were more likely to have a history of depression compared to non-users. The study also found that sustained EC use and frequency of use were associated with an increase in depression symptoms over a 12-month period. 35 Similarly, in our umbrella review, depression outcomes were associated with mental health outcomes including depression by Becker et al 28 and Chadi et al 31 where outcomes of 119 747 children were pooled in. Our study found that depressive symptoms on a whole had higher associations with EC-only, EC/CC use as compared to no use; these trends were noticed with lifetime EC-only use and with the past 30 days of use. Our findings are also supported by current literature where links are proposed between mental health and nicotine—which is known to increase depressive feelings. Cullen et al reported study findings of nearly 30 000 EC users, frequent vaping leads to an estimated 2.4 higher likelihood of being diagnosed with depression. 36
A review of 7 studies assessed the impact of vaping and electronic cigarette (EC) use on mental health. 37 The review found that suicide attempts were significantly more common among EC users compared to non-users. 37 Data from a survey of Korean middle and high school students also found that students who had used ECs in the past 30 days had higher rates of suicidal ideation, suicide planning, and attempts compared to non-EC users. 38 Previous studies have linked nicotine addiction from combustible cigarettes with an increased risk of suicidality.39,40 Our review found that suicidality was more common in electronic cigarette (EC) users, with higher rates of suicidal ideation, suicide plans, and suicide attempts observed in individuals with past-12-month EC use (Becker et al 28 ). In 1 case, suicide planning was found to be higher among females, however, the findings were not conclusive and further research is needed to fully understand the relationship between EC use and suicidality in female. Electronic cigarette (EC) use has been linked to a range of mental health issues in adolescents, including impulsivity, anxiety, and suicidality. A cross-sectional survey of 927 EC users found that impaired self-regulation and behavioral impulsivity predicted trying ECs at a younger age, and that early-age consumption was associated with a higher risk of frequent EC use. 41 This review also found that earlier age of EC onset and ever-use of combustible cigarettes was associated with high impulsivity. A review of 13 366 participants found that earlier age of EC onset and ever-use of combustible cigarettes was associated with high impulsivity as measured by the Temperament and Character Inventory (TCI) impulsivity scale and analytical models (odds ratios >1). It is important to further study the longitudinal relationship between EC use and impulsivity in order to fully understand the impact of EC use on impulsivity in adolescents.
Data from a national survey of children and youth aged 3 to 17 years in the US found that 7.1% of EC users were diagnosed with anxiety. EC use has also been found to be more common among individuals with substance use disorders and psychiatric disorders.42,43 In our review, anxiety disorder was reported by Becker et al and Chadi et al, 31 pooling in 6563 participants. Anxiety was associated with illicit substance vaping (OR = 1.96) and lowered anxiety sensitivity among CC compared to EC users.
The authors of the study by Bhave and Chadi 44 discuss the risks of electronic cigarettes (EC) and vaping use among youth globally, with a focus on the situation in India. They mention that even though vaping is banned in India, it still poses a significant threat to youth in the country. Due to the increasing usage of EC, healthcare workers are often times required to treat vaping-associated lung injuries. EC and vaping use among youth is a significant public health concern, and it is important for countries like India to consolidate public health measures to prevent mental and physical damage incurred by vaping.
Duan et al 45 examined the relationship between electronic cigarette (EC) use and cannabis use over a 4-year period and assessed for any mental health impacts of EC use. The authors found that at baseline, both cannabis and EC use were significantly associated with each other. When considering the initiation of cannabis use over the course of the study, they found that individuals with internalizing mental health problems (OR = 2.51) were more likely to initiate cannabis use. This study is particularly important because both cannabis use and EC use have been linked to severe internalizing mental health problems. The authors of this study recommend that efforts should be made to curb the use of electronic cigarettes (ECs) due to the longitudinal association between EC use and cannabis initiation. To address this issue, specific interventions should be implemented nationally to target youth who have been exposed to ECs. 45
E-cigarette vaping-associated lung injury (EVALI) is a serious concern among young adolescents in the US, with cases approaching epidemic levels. The use of nicotine and tetrahydrocannabinol in e-cigarettes has been linked to long-term health implications, including mental health problems, morbidity, and even mortality. Reddy et al 46 studied e-cigarette vaping-associated lung injury (EVALI) in pediatric intensive care units. Among young adolescents, EVALI has been largely reported in the US, nearing epidemic levels. 46 In their retrospective case series, the authors reported nicotine EC and tetrahydrocannabinol use among 6 patients aged 17 years. 46 While none of the pediatric patients died, there were many concerns raised for the long-term implications e-cigarettes have on the young; including but not limited to mental health well-being, morbidity—specifically lung health, and mortality. 46
A study by Jacobs et al 47 examined the motivations behind vaping and its impact on behavior by examining the sensitivities of the behavioral activation system (BAS) and behavioral inhibition system (BIS) in relation to cannabis and vaping. The study found that among 2467 students in the 11th grade in California, those who used nicotine were more likely to have fun-seeking scores (P < .05) and lower BIS scores compared to non-users (P < .05). On the other hand, those with higher BIS scores were less likely to consume cannabis (OR = 0.91). 47 While the authors specifically targeted outcomes of behaviors, we believe that different forms of motivation must be studied. 47 These will help in designing public programs that can target different adolescent groups to reduce trends of cannabis and nicotine vaping. 47
Rahmandar et al 48 write that over 1.7 million high school students use EC, but they find that a large proportion of them include Caucasians who self-identify as transgender and gay, lesbian, and youth with disabilities. While the authors’ focus is on the racial and ethnic targets, we find that key regulations and recommendations targeted at the pre-specified groups may help in curbing the EC epidemic and improve community-level mental health outcomes. 48
Our umbrella review has certain limitations. First, we included only those studies that self-identified as systematic/meta-analysis studies in the title, abstract, keyword, or methods. Nonetheless, we carried out a thorough search of the reference lists of included studies to ensure that no omissions were made. Second, the effect sizes across the included reviews were insufficient in quantitative terms, where included reviews only included case presentations. Third, while the 6 reviews included in this umbrella review were published after 2016, the primary clinical studies were dating back to the earlier-usage of EC. Finally, it is important to consider that the primary original studies included in this umbrella review may have overlapped, therefore overrepresenting the findings of given studies.
Conclusion
This umbrella review included data from 846,510 children aged 21 years or younger, representing a diverse range of ethnicities and geographical backgrounds. So far, there has been no umbrella review addressing the relationship between vaping and mental health outcomes in children. To date, there has been no umbrella review addressing the mental health outcomes of children who use electronic cigarettes (ECs). While mounting evidence links EC use to mental health outcomes, it is crucial to address these potential consequences in children. Future reviews should examine the duration of EC exposure and evaluate the impacts on depression, suicidality, anxiety, and impulsivity to establish concrete associations. This, in turn, will enable more effective mental health and policy-based interventions to be designed to safeguard public health.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_11782218231167322 for Vaping and Mental Health Conditions in Children: An Umbrella Review by Ali Mahmood Khan, Saeed Ahmed, Zouina Sarfraz and Pantea Farahmand in Substance Abuse: Research and Treatment
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contribution: The authors confirm contribution to the paper as follows: study conception and design: AMK and ZS; data collection: ZS; analysis and interpretation of results: AMK, SA and ZS. draft manuscript preparation: AMK, SA, ZS and PF. All authors reviewed the results and approved the final version of the manuscript.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.CDC. Surgeon General’s Advisory on E-cigarette Use Among Youth. 2018. Accessed August 5, 2022. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/surgeon-general-advisory/index.html
- 2.CDC. About Electronic Cigarettes (E-Cigarettes). 2022. Accessed August 5, 2022. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/about-e-cigarettes.html
- 3.Fox M. More than 2 million US teens use e-cigarettes, a quarter of them daily, CDC and FDA find. 2021. Accessed August 5, 2022. https://edition.cnn.com/2021/09/30/health/youth-tobacco-survey-vaping/index.html
- 4.E-cigarettes: Facts, stats and regulations. 2021. Accessed August 5, 2022. https://truthinitiative.org/research-resources/emerging-tobacco-products/e-cigarettes-facts-stats-and-regulations
- 5.Global E-Cigarette Market (2022 to 2027) - Industry Trends, Share, Size, Growth, Opportunity and Forecasts - ResearchAndMarkets.com | Business Wire. 2022. Accessed August 5, 2022https://www.businesswire.com/news/home/20220401005272/en/Global-E-Cigarette-Market-2022-to-2027—Industry-Trends-Share-Size-Growth-Opportunity-and-Forecasts—ResearchAndMarkets.com [Google Scholar]
- 6.Williams JM, Ziedonis D. Addressing tobacco among individuals with a mental illness or an addiction. Addict Behav. 2004;29:1067-1083. [DOI] [PubMed] [Google Scholar]
- 7.Patten SB. Vaping and mental health. J Can Acad Child Adolesc Psychiatry. 2021; 30:3. [PMC free article] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021;372. [DOI] [PubMed] [Google Scholar]
- 9.Methodology for JBI Umbrella Reviews. 2014.Accessed May 5, 2022. www.joannabriggs.org
- 10.Lim CCW, Sun T, Leung J, et al. Prevalence of adolescent cannabis vaping: A systematic review and meta-analysis of US and Canadian studies. JAMA Pediatr. 2022;176:42-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Notley C, Gentry S, Cox S, et al. Youth use of e-liquid flavours-a systematic review exploring patterns of use of e-liquid flavours and associations with continued vaping, tobacco smoking uptake or cessation. Addiction. 2022;117:1258-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bozier J, Chivers EK, Chapman DG, et al. The evolving landscape of e-cigarettes: a systematic review of recent evidence. Chest. 2020;157:1362-1390. [DOI] [PubMed] [Google Scholar]
- 13.Selph S, Patnode C, Bailey SR, Pappas M, Stoner R, Chou R.Primary care-relevant interventions for tobacco and nicotine use prevention and cessation in children and adolescents: updated evidence report and systematic review for the US preventive services task force. JAMA. 2020;323:1599-1608. [DOI] [PubMed] [Google Scholar]
- 14.Gonsalves CL, Zhu JW, Kam AJ.Diagnosis and acute management of e-cigarette or vaping product use-associated lung injury in the pediatric population: a systematic review. J Pediatr. 2021;228:260-270. [DOI] [PubMed] [Google Scholar]
- 15.Pericot-Valverde I, Elliott RJ, Miller ME, Tidey JW, Gaalema DE.Posttraumatic stress disorder and tobacco use: a systematic review and meta-analysis. Addict Behav. 2018;84:238-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glasser AM, Collins L, Pearson JL, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med. 2017;52:e33-e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia PD, Gornbein JA, Middlekauff HR.Cardiovascular autonomic effects of electronic cigarette use: a systematic review. Clin Auton Res. 2020;30: 507-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Brien D, Long J, Quigley J, Lee C, McCarthy A, Kavanagh P. Association between electronic cigarette use and tobacco cigarette smoking initiation in adolescents: a systematic review and meta-analysis. BMC Public Health. 2021; 21:954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gentry S, Forouhi NG, Notley C.Are electronic cigarettes an effective aid to smoking cessation or reduction among vulnerable groups? A systematic review of quantitative and qualitative evidence. Nicotine Tob Res. 2019;21:602-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee SJ, Rees VW, Yossefy N, Emmons KM, Tan ASL.Youth and young adult use of pod-based electronic cigarettes from 2015 to 2019: a systematic review. JAMA Pediatr. 2020;174:714-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith H, Lucherini M, Amos A, Hill S. The emerging norms of e-cigarette use among adolescents: a meta-ethnography of qualitative evidence. Int J Drug Policy. 2021;94:103227. [DOI] [PubMed] [Google Scholar]
- 22.Kinouani S, Leflot C, Vanderkam P, Auriacombe M, Langlois E, Tzourio C. Motivations for using electronic cigarettes in young adults: a systematic review. Subst Abus. 2020;4:315-322. [DOI] [PubMed] [Google Scholar]
- 23.Tzortzi A, Kapetanstrataki M, Evangelopoulou V, Beghrakis P. A Systematic literature review of e-cigarette-related illness and injury: not just for the respirologist. Int J Environ Res Public Health. 2020;17:2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fluharty M, Taylor AE, Grabski M, Munafò MR.The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19:3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gogliettino AR, Potenza MN, Yip SW.White matter development and tobacco smoking in young adults: A systematic review with recommendations for future research. Drug Alcohol Depend. 2016;162:26-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Underner M, Perriot J, Brousse G, et al. Cigarette électronique chez les patients fumeurs présentant une pathologie psychotique. Revue de la littérature [Contribution of electronic cigarettes in smoking patients with psychotic disorders. A literature review]. Encephale. 2021;47:452-460. [DOI] [PubMed] [Google Scholar]
- 27.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becker TD, Arnold MK, Ro V, Martin L, Rice TR. Systematic review of electronic cigarette use (vaping) and mental health comorbidity among adolescents and young adults. Nicotine Tob Res. 2021;23:415-425. [DOI] [PubMed] [Google Scholar]
- 29.Chan GCK, D Stjepanović, Lim C, et al. Gateway or common liability? A systematic review and meta-analysis of studies of adolescent e-cigarette use and future smoking initiation. Addiction. 2021;116:743-756. [DOI] [PubMed] [Google Scholar]
- 30.Rothrock AN, Andris H, Swetland SB, et al. Association of E-cigarettes with adolescent alcohol use and binge drinking-drunkenness: asystematic review and meta-analysis. Am J Drug Alcohol Abuse. 2020;46:684-698. [DOI] [PubMed] [Google Scholar]
- 31.Chadi N, Schroeder R, Jensen JW, Levy S. Association between electronic cigarette use and marijuana use among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2019;173:e192574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017; 171:788-797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hua M, Talbot P. Potential health effects of electronic cigarettes: a systematic review of case reports. Prev Med Rep. 2016;4:169-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miech R, Patrick ME, O’Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017;26:e106-e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Obisesan OH, Mirbolouk M, Osei AD, et al. Association between e-cigarette use and depression in the behavioral risk factor surveillance system, 2016–2017. JAMA Netw Open. 2019;2:e1916800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cullen KA, Gentzke AS, Sawdey MD, et al. E-cigarette use among youth in the United States, 2019. JAMA. 2019;322:2095-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Javed S, Usmani S, Sarfraz Z, et al. A scoping review of vaping, E-cigarettes and mental health impact: depression and suicidality. J Community Hosp Intern Med Perspect. 2022;12:33-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim JS, Kim K. Electronic cigarette use and suicidal behaviors among adolescents. J Public Health. 2021;43:274-280. [DOI] [PubMed] [Google Scholar]
- 39.Bohnert KM, Ilgen MA, McCarthy JF, Ignacio RV, Blow FC, Katz IR. Tobacco use disorder and the risk of suicide mortality. Addiction. 2014;109: 155-162. [DOI] [PubMed] [Google Scholar]
- 40.Clarke DE, Eaton WW, Petronis KR, Ko JY, Chatterjee A, Anthony JC. increased risk of suicidal ideation in smokers and former smokers compared to never smokers: evidence from the baltimore ECA follow-up study. Suicide Life Threat Behav. 2010;40:307-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bold KW, Morean ME, Kong G, et al. Early age of e-cigarette use onset mediates the association between impulsivity and e-cigarette use frequency in youth. Drug Alcohol Depend. 2017;181:146-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206: 256-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Masaki K, Taketa RM, Nakama MK, Kawamoto CT, Pokhrel P. relationships between depressive symptoms, anxiety, impulsivity and cigarette and E-cigarette use among young adults. Hawai’i J Heal Soc Welf. 2022;81:51. [PMC free article] [PubMed] [Google Scholar]
- 44.Bhave SY, Chadi N. E-cigarettes and vaping: a global risk for adolescents. Indian Pediatr. 2021;58:315-319. [PubMed] [Google Scholar]
- 45.Duan Z, Wang Y, Spears CA, et al. Role of mental health in the association between E-Cigarettes and cannabis use. Am J Prev Med. 2022;62:307-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reddy A, Jenssen BP, Chidambaram A, Yehya N, Lindell RB. Characterizing E-cigarette vaping-associated lung injury in the pediatric intensive care unit. Pediatr Pulmonol. 2021;56:162-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jacobs W, Merianos AL, Mahabee-Gittens EM, Leventhal A. Vaping motivations: association of behavioral inhibition and behavioral activation systems with nicotine and cannabis vaping among adolescents. Addict Behav. 2022;135: 107436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rahmandar MH, Gribben V. E-cigarette disparities: who are the targets? Curr Probl Pediatr Adolesc Health Care. 2022;52:101201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_11782218231167322 for Vaping and Mental Health Conditions in Children: An Umbrella Review by Ali Mahmood Khan, Saeed Ahmed, Zouina Sarfraz and Pantea Farahmand in Substance Abuse: Research and Treatment