FIGURE 1.
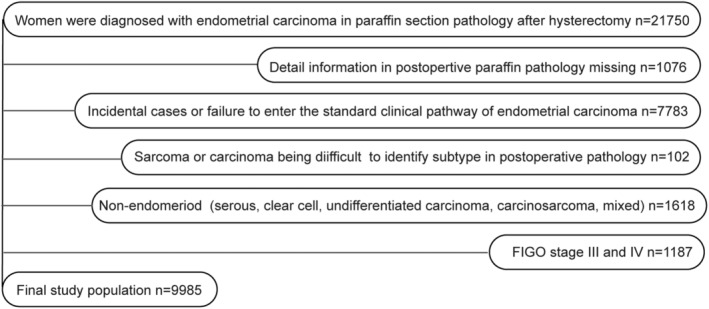
Flowchart showing the inclusion and exclusion of study participants. The endometrial carcinoma database had 21,750 cases accurately diagnosed in postoperative pathology; 1,076 cases without postoperative pathology details were excluded, including localized endometrial carcinoma lesions only confined to the endometrium layer. Lesions were removed during preoperative biopsies, and no cancer lesions were found in postoperative paraffin pathological sections. We excluded 7,783 incidental cases or cases out of the standard clinical pathway of endometrial carcinoma. Some cases were accidentally found with endometrial carcinoma during uterus intraoperative gross evaluation (IGE), IFS, or postoperative pathology, which did not undergo the standardized clinical pathway of endometrial carcinoma and standardized pre/intraoperatively high‐risk factors assessments. Included patients were preoperatively diagnosed based on a previous biopsy or were observed with definite intrauterine occupations in preoperative imaging or ultrasound. Admission diagnoses comprised endometrial carcinoma, occupation disease in the uterine cavity or atypical hyperplasia (possible endometrial carcinoma). We excluded 102 sarcomas or cases difficult to diagnose. In the remaining 12,789 participants, we excluded 1,618 patients with non‐endometrioid endometrial carcinoma (serous, clear cell, undifferentiated, mixed carcinoma, and carcinosarcoma). After excluding 1,187 cases in clinical‐stage III/IV, 9,985 EA women who underwent pre/intraoperatively high‐risk factors assessment were retrieved for subsequent analysis.
