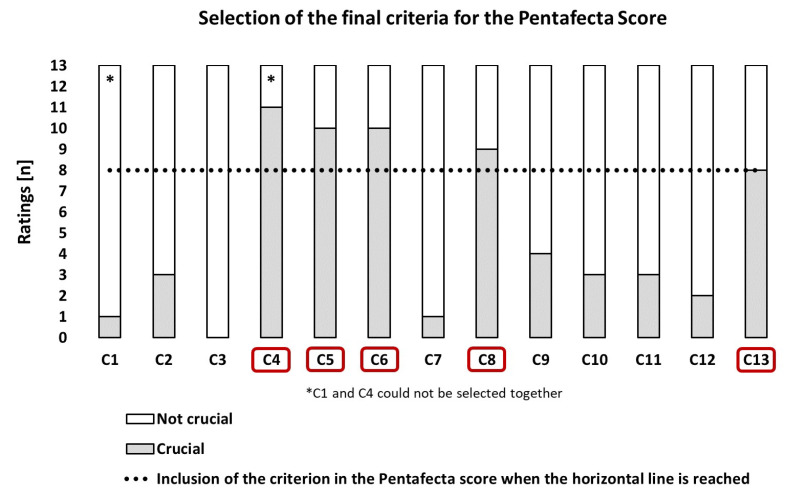
Figure 1.
Formation of the final Pentafecta score based on the ratings of 13 experts on 13 predefined criteria (C1–C13). Legend: C1: There are no specifications for surgical primary therapy—achieving a negative surgical margin is the sole treatment goal. C2: There should be no postsurgical complications of severity grade 3+ (according to Clavien–Dindo) occurring within a time interval of 3 months after surgical therapy of the primary tumor and after nodal lymph node staging. C3: If indicated, the bilateral inguinal lymph node dissection should always include a minimum number of 14 removed lymph nodes. C4: Organ-preserving surgery of the primary tumor is performed if the tumor stage allows (< pT3), although always with the aim of achieving a negative surgical margin. C5: Starting at the tumor stage pT1G2N0, a bilateral inguinal lymph node staging should be performed in all patients, using modified inguinal lymph node dissection (ILND) or dynamic sentinel node biopsy for N0, and radical ILND for N1–2. C6: There should be access to an interdisciplinary tumor board for expert advice and discussion on perioperative chemotherapy (neoadjuvant/adjuvant) for patients with fixed inguinal lymph node metastases (cN3) and patients with pN2–3 after surgical lymph node dissection. C7: The treating hospital should have the interdisciplinary option for radiotherapy (EBRT/Brachytherapy) and should also present this treatment option to their patients in clinical tumor stage T1–2 with a tumor size < 4 cm. C8: If indicated, the inguinal lymph node dissection should be performed within a time window of 3 months for the surgical therapy of the primary tumor. C9: Every patient undergoing surgical primary therapy for penile cancer should receive a 5-year comprehensive individual oncological follow-up (aftercare) plan and be offered the possibility of psychological counseling or treatment, regardless of the extent of the procedure. C10: Surgery for the primary tumor should always be performed with frozen section analysis of the margins. C11: Refer the patient to a specialist lymphoedema therapist (physiotherapist) following ILND surgery. C12: Both surgical interventions on the primary tumor and potential ILND should be performed in accordance with current guideline recommendations for antibiotic prophylaxis. C13: The surgical primary therapy (primary tumor and, if necessary, lymph nodes) should always be carried out at a center with a minimum case volume of n = 15 primary treated cases of penile cancer per year.