Abstract
Medical student interest and pursuit of a career in pathology have been steadily declining since 2015. We conducted three separate surveys of medical students to better understand these trends. In our first survey, we focused on assessing U.S. allopathic medical students understanding and perceptions of pathology. We later surveyed U.S. osteopathic medical students as a companion to the allopathic medical student survey, in which many similarities were discovered with some key differences. In our final survey, we specifically looked at curriculum differences between the U.S. allopathic medical schools that graduate the most students who enter pathology training programs (Group 1) versus those schools that graduate the fewest future pathologists (Group 2) to determine if the curriculum had an impact on medical student matriculation into pathology. Together, through these surveys, we were able to identify several remarkable recurring trends, presenting areas of targetable action. Here, we summarize themes from the three studies as well as a review of pertinent literature to offer best practices for exposing and engaging medical students to pathology and possibly recruiting students to consider pathology as a career.
Keywords: Career, Education, Experiential learning, Medical student, Pathology, Specialty choice
Introduction
Every medical student learns about pathology during pre-clinical training as the basis of disease. Through lectures and small group-based learning (i.e. problem-based/case-based learning), students have variable experiences in laboratory medicine.1 In clinical clerkships, every medical student experiences the importance of laboratory testing for patient care. However, many medical students are unaware of the duties of pathologists in their clinical practice. Recent studies highlight the opportunity of exposing medical students to pathology as a clinical practice.2, 3, 4, 5, 6, 7, 8 Exposing medical students to pathology during clinical clerkships years may offer an opportunity to recruit students to pathology, and at the very least will show every medical student the importance of pathology and laboratory medicine in patient care. Many specialties have advocated for medical school exit competencies, fundamental skills, and knowledge that all doctors should have command of to provide quality patient care. The Canadian Association of Pathologists has recommended exit competencies for pathology and laboratory medicine, which could be used to promote exposure to pathology throughout the medical school curriculum.3
Understanding of pathology as a clinical practice
Arguably, the greatest challenge to medical student engagement in pathology is a lack of understanding of the day-to-day responsibilities of a pathologist. Only 70% of allopathic respondents and 57% of osteopathic respondents agreed or strongly agreed they understand pathology job-related responsibilities, leaving 30–40% of medical students without a clear understanding of what a pathologist actually does. Furthermore, only 30% of osteopathic medical students felt they had sufficient exposure to pathology to consider it as a specialty compared to 60% of allopathic students. This lack of exposure to pathology is a trend seen in other countries as well.2, 3, 4, 5, 6, 7, 8 In a survey of medical students at a private institution in Pakistan, 27.8% of students reported a lack of sufficient exposure to pathology in order to consider it as a career.2 This lack of visibility tends not only to decrease medical student recruitment into pathology but also leaves medical students ill-prepared to properly utilize pathology services in patient care. Interestingly, while osteopathic students report having less exposure to pathology, data show that there is an upward trend in osteopathic students applying to pathology.9 Possible contributing factors to this may have to do with the growth of osteopathic schools as well as the context of experience osteopathic students have compared to allopathic students.9 While osteopathic students report less microscope use and less autopsy exposure, this may inadvertently leave them more open to considering pathology as a specialty as they are not influenced by negative ideas in pathology (i.e., we only do autopsy or do not talk to people”). In addition, osteopathic students rank lifestyle expectations higher than allopathic students, which may also be a contributing factor to this trend.9
Pathology in the preclinical years
Current allopathic and osteopathic medical school curricula feature pathology exposure predominantly in the classroom setting during the preclinical years. However, our data suggest that the preclinical curriculum alone is not the driving force for the decline in medical student interest in pathology. Pathology education in the preclinical years is often part of an integrated curriculum with only 3% of the schools surveyed in the curriculum study reporting a free-standing pathology course.10 This number will likely continue to decline as many medical schools are undergoing curriculum changes, in favor of an integrated system. Preclinical pathology education predominantly occurs through lecture format in lieu of hands-on experiences. However, even pathology educational lectures are becoming less visible as more medical students look to sources outside of their institutional lectures to supplement their education.11 Of note, participation in a separate histology or pathology course was not statistically significantly different between allopathic or osteopathic students among those who considered pathology versus those who did not, and there was no difference between allopathic and osteopathic students overall.9,10 In addition, there was no statistically significant difference between preclinical curriculum between Group 1 and Group 2 pathologist-producing schools.12
Pathology in the clinical years
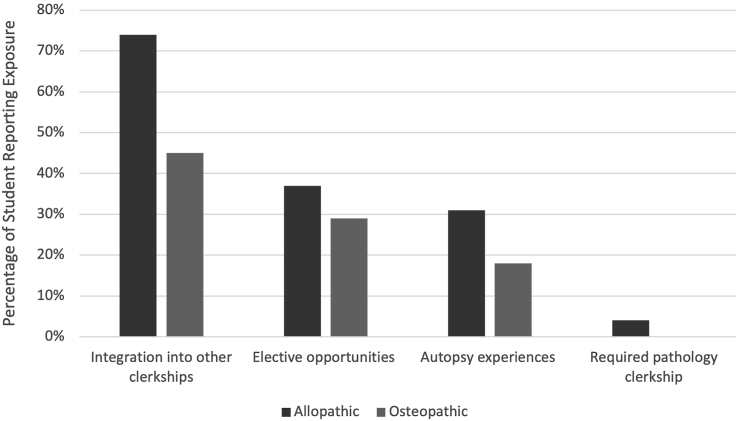
Exposure to pathology in the clinical years of undergraduate medical training is significantly limited and is quite variable. While most allopathic and osteopathic students report having some exposure to pathology during this time, 14% of allopathic students and 34% of osteopathic students reported no exposure to pathology in the clinical years at all.9,10,12 The clinical years, particularly the third year, are a significant milestone in undergraduate medical education as it traditionally marks the beginning of core clinical rotations. Over half of allopathic and osteopathic medical students reported deciding on their medical specialty during their 3rd year of medical school.9,10 Current trends in pathology exposure in the clinical years include integration during other rotations (74% allopathic students and 45% osteopathic students), elective opportunity (37%, 29%), autopsy experience (31%, 18%), and required pathology rotation (4%, 0%)(Fig. 1).9 Of note, allopathic students were statistically more frequently exposed to pathology in another rotation or observed an autopsy, as compared to osteopathic students.9 As medical students are immersed in core clinical specialties, they are also learning how pathology data are being used to manage patients. Not surprisingly both allopathic and osteopathic medical students endorse that clinical rotations are an important factor in determining specialty choice (90% vs 85%, respectively). Interestingly, a study of medical students in Saudi Arabia found that there was a decrease in pathology interest as students entered into the clinical years.7 It is unclear if this is due to a lack of exposure to pathology in the clinical years or some other factors.
Fig. 1.
Exposure to pathology in the clinical curriculum. The figure illustrates the differences in the top clinical experiences of allopathic and osteopathic medical students in pathology. Allopathic students overall report more exposure to pathology in the clinical years than osteopathic students.
Integrating pathology into clinical curriculum
The idea of a dedicated pathology rotation for all medical students, including rotations through various sections of the anatomic and clinical pathology service, while highly appealing, is realistically not feasible for most medical schools. Only 4% of allopathic (and no osteopathic) students reported participating in a required rotation, and only two medical schools (7%) reported a required pathology curriculum in the 3rd year of medical school.12 Integration of pathology into clinical rotations is much more common (33% of schools surveyed and 47% Group 1 vs 20% Group 2).12 Pathology was most commonly integrated into general surgery (n = 3) and obstetrics and gynecology (n = 3), but also neurology (n = 2), internal medicine (n = 1), and family medicine (n = 1).12 Such experiences ranged from 2 h to 2 weeks in pathology and included activities, such as rotating through the laboratory during internal medicine rotation, attending brain cutting during neurology rotations, and attending frozen sections or sign-out during surgery and obstetrics and gynecology rotations (see Table 1 for additional descriptions of the experiences).12 While these experiences predominantly focused on anatomic pathology, opportunities for similar experiences could also be created in clinical pathology specialties, including spending time in the microbiology laboratory during internal medicine, working up transfusions reactions to include rotating through the blood bank during surgery, internal medicine, or an emergency medicine rotation. The University of Michigan Medical School integrated one week of pathology in the surgery rotation, which included anatomic pathology experiences (autopsy, sign-out, and grossing), along with experiences in different clinical pathology rotations (chemistry and blood banking). In their survey, 79% of the 263 students who had the experience rated it positively.5
Table 1.
Integration of pathology into the clinical curriculum.
| Experience | Number of programs | Rotation (s) | Duration | Description of experience |
|---|---|---|---|---|
| Tumor board | 3 | Surgery, OB/GYN (2) | 1 h | Attend tumor board |
| Case-based discussion | 2 | Internal medicine, Not specified |
3 days, half-day | Laboratory medicine workshop case-based discussion of laboratory test ordering, how often, and how to interpret. Case-based discussion – 1 afternoon a week |
| Frozen sections and specimen grossing | 3 | Surgery, not specified | Not specified | Observe the frozen section process, observe specimen grossing and tissue processing |
| Sign-out | 4 | Surgery, internal medicine, Ob/GYN (2) | Half-day, 1 day | Sit in on surgical pathology, hematopathology, or gynecologic pathology sign-out |
| Brain cutting | 2 | Neurology | Once per week, half-day | Attend brain cutting |
| Follow specimen | 1 | Not specified | Not specified | Follow specimen to laboratory as part of clinical team |
| Rotation through clinical Laboratory | 1 | Internal medicine | 3 days total | Rotation through four laboratory sections (hematopathology, microbiology, coagulation, and chemistry) to understand test turnaround time |
| Not specified | 1 | Family medicine | 2 h | Experience not specified |
| Not specified | 1 | Multiple | Not specified | Embedded into every clinical clerkship |
Elective experiences in pathology
Approximately one-third of allopathic (37%) and osteopathic (29%) medical students have elective opportunities in pathology. Students who participated in elective opportunities or research opportunities in pathology were more likely to consider pathology as a career as compared to students who did not consider pathology.12 This trend has also been found in other countries.6 The level of participation in elective experiences appears to have some impact on students’ decisions to go into pathology, with active participation offering a more meaningful experience.1 Most Group 1 allopathic medical schools reporting having an elective in which the medical student had a role most similar to a resident, attended tumor boards, and participated in sign-out (33–53% [Group 1] vs 7–28% [Group 2]). In comparison, Group 2 schools reported having more of a shadowing experience (13% [Group 1] vs 29% [Group 2]).12 A different survey of medical students found that those students who had enrolled in a pathology elective were more likely to express an interest in pathology than those who had not (44% versus 24%, respectively).7
Other opportunities for exposure to pathology
Post-sophomore fellowship: Post-sophomore fellowship (PSF) opportunities are another option for giving medical students exposure to pathology responsibilities. Sixty-seven percent (67%) of Group 1 schools offer some form of extended pathology experience compared to 27% of Group 2.12 Fifteen percent of pathology residency programs report a PSF affiliated with their medical school.13 Many of these opportunities have been in existence for more than 10 years, with four programs adding the opportunity in the last five years.13 University of Iowa's PSF, started in 1995, has graduated 126 fellows of which 43% went into pathology, suggesting the significant impact PSF could have on medical student experience in pathology.14 Similar findings have also been seen in other PSF programs, including the University of Vermont, another long-standing PSF program.15 Previously, part of the appeal of such programs from a student fellow perspective might have been that the PSF year could count toward one year of ACGME-accredited pathology training, which is no longer the case.13
Other opportunities to expose students to pathology outside of the scheduled curriculum include summer fellowships between the 1st and 2nd years of medical school, summer research, extended research experiences, or another one-year fellowship/observership experience.12 UC Davis’ summer research program geared toward undergraduate medical students seeks to expose them to pathology and laboratory medicine and 55% of the students who completed the program considered a career in pathology.16 Medical student engagement in experiences such as these may be helpful with recruitment and better understanding of pathology.
Mentorship: Although attracting medical students to pathology is imperative, pathologists also need to be available to mentor them. While most medical schools have some pathology mentors, the degree of involvement varies between Group 1 and Group 2 pathologist-producing programs. More Group 1 schools had mentors who provided information regarding careers and mentors who participated in academic advising. Access to an engaged mentor is important as 50% of students surveyed in both Group 1 and Group 2 pathologist-producing schools listed this as a major way in which medical schools help students with choosing a specialty.12 Signing up to be a mentor and engaging in both pathology-related (i.e. College of American Pathologist Pathologist Pipeline Champion Program) and even non-pathology-related activities helps build those relationships, which may lead to better recruitment efforts. Only 11% of osteopathic students and 33% of allopathic students agreed or strongly agreed that pathologists actively recruited them.12
Interest groups: Participation in pathology student interest groups (PathSIG) by organizing laboratory tours, holding microscopic slide sessions, simulating tumor board sessions, or frozen sections are supplementary activities to engage, show interest, and mentor students. While there were no statistically significant differences found when comparing PathSIGs in both Group 1 and Group 2 schools, all Group 1 schools reported having a PathSIG compared to 73% of Group 2 schools.12 Of note, a significant portion of medical students were unaware whether their school had a PathIG, so in addition to participating in these activities, better advertisement of events and more active recruitment is also important.
Addressing attitudes/negative perceptions of pathology and pathologists and the role of social media
Attitudes and social media: In a recent survey of medical students, factors that they identified that influenced their choice of specialty included job opportunities (95%), self-interest (95%), income (90.2%), working hours (87%), level of stress (79.9%), and patient–doctor interaction (76.9%). When asked about the specialty of pathology, these same students said that pathologists do not interact with patients (72.2%), which would have been viewed as a negative aspect of the specialty. Some of these students (48.8%) said that pathology is too complex; only 28.1% said that pathologists are highly paid and 16.3% said that pathology does not allow for part-time work.6 Another survey of medical students found that factors contributing to their lack of interest in pathology as a specialty choice included lack of general interest (37.4%), lack of exposure (27.8%), and lack of patient interaction (14.6%).6 In both of these surveys, the expressed lack of ”self-interest" or ”general interest” in pathology was not further described, but might partly be explained by a lack of understanding of the various potential roles of pathologists.
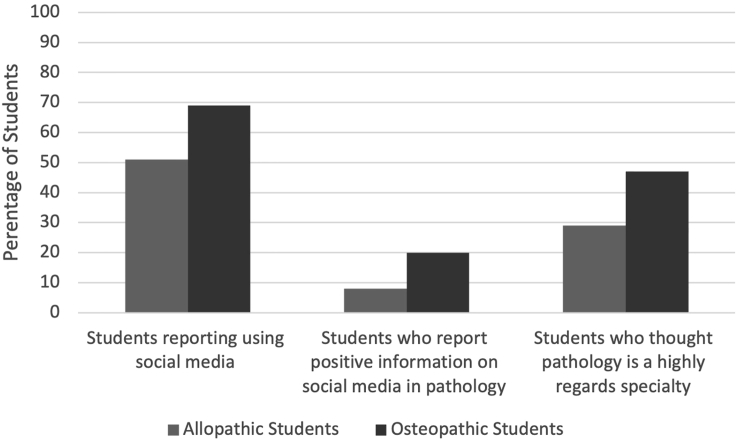
Findings from our previous study examining the factors that influence US allopathic medical students to pursue a pathology career found that pathology is not a respected specialty. Only 29% of allopathic respondents thought pathology was a highly regarded specialty compared to 47% of osteopathic students.9,10 Furthermore, in our current curriculum, students from both Group 1 and Group 2 pathology-producing schools reported that pathology is “out of sight, out of mind.” With this, comes many negative perceptions about the specialty, including a saturated job market and that pathologists are introverted, socially awkward individuals. Social media often perpetuates these ideas. A significant proportion of medical students use these platforms to learn about different specialties. Fifty-one percent (51%) of allopathic respondents in our survey admitted to using Internet/social media to research pathology, and only 8% of respondents who did not go into pathology agreed or strongly agreed that information on social media regarding pathology is encouraging.10 These findings were even more pronounced in the osteopathic student survey, in which 69% of respondents reported using social media to learn about pathology and less than 20% reported finding the data to be encouraging (Fig. 2).9 Considering 51.8% of medical students from another survey indicated that ”prestige” was a factor influencing their choice of specialty and 95% of those students also listed job opportunities as an important factor, it is not surprising that these negative perceptions would impact the number of students who might choose pathology as a career.6
Fig. 2.
Medical students’ attitudes toward pathology. The figure illustrates both allopathic and osteopathic students' attitudes/social media perceptions to pathology as a specialty.
Negative impressions on social media whether true or false can influence medical student decision-making. However, having more pathologists at all levels (resident, fellow, and attending) active on social media could help to dispel some of these negative impressions. Pathology Twitter (”#pathtwitter”) and sites like PathElective.com are growing in popularity.17,18 Attendings, residents, and medical students alike engage with each other as well as with other specialties by posting interesting cases, conferences, and even sharing job opportunities. The College of American Pathologists Virtual Lecture Series is a great example of how social media can influence the pathology narrative. The lecture series, associated with the “#CAPVirtualPath” Twitter phrase, at one point had 73 million impressions.17 While social media is not the only way to have an influence on medical students, advocating for the specialty to change perceptions of pathology through its use is key to reaching this younger generation.
Patient interaction or lack thereof: A significant challenge to garnering medical school recruitment into pathology is the lack of patient interaction. The nature of the specialty limits patient contact and while some have chosen pathology for this very reason, many medical students decide against pathology because of a desire for more patient contact. In our survey, 68% of allopathic respondents and 91% of osteopathic respondents who decided against pathology did so because of a preference for more patient contact.9,10 A recent survey of medical students found that 72.2% of them thought that pathologists do not interact with patients, which is significant since the ‘patient–doctor interaction’ was reported by 76.9% of the students as a factor that influenced their choice of specialty.6
This aspect of pathology cannot be changed; most pathologists do not regularly directly interact with patients, but there are options in pathology for medical students who prefer to not give up all patient contact. These opportunities are particularly available in transfusion medicine (e.g. apheresis procedures and massive transfusion protocols) as well as in cytology with the performance of fine needle aspirations. In addition, there is a growing trend of “pathology explanation/care clinics”, in which patients are able to sit with a pathologist and go over their slides and results.19 One such program, which is offered by the College of American Pathologists, is the See, Test, Treat program, an annual women's health cancer screening and health education event in which women receive physical examinations, including pelvic exams with Pap smear and mammograms and are able to sit with pathologists the very same day to look at their slides.20
Pathologists are an integral part of the team (system-based practice)
Importantly, while most pathologists may not directly interact with patients, medical students must be reminded that pathology diagnoses directly affect patient care. Pathologists are directly apart of the medical team. Pathologists render diagnoses that inform treatment plans, perform frozen sections that may alter surgical approach, participate in tumor boards where interdisciplinary discussion guides patient care, manage transfusion medicine services providing direct patient care, and run laboratories. Pathologists often take part in radiologic-pathologic correlation conferences and mortality and morbidity conferences. Regardless of specialty choice, medical students must have a basic understanding of the role of the pathologists as pathologists are an integral part of the clinical team.
Conclusion
Much of the decline of U.S. medical students matching into pathology can be attributed to voids in exposure and understanding rather than aversion to the field. Our profession has an opportunity to fill these voids through the incorporation of pathology into core clinical clerkships, development of PFSs, mentorship, and using social medial as a tool to engage students and refute negative perceptions. Experiential exposure to pathology is imperative in medical education as pathology is crucial to providing comprehensive patient care. The CAP has used the data and ideas generated from the work of the CAP GMEC to inform the efforts of the CAP Pathologist Pipeline Ad Hoc Committee (PPAHC). Key initiatives of the PPAHC have included significant outreach through marketing on social media, encouraging involvement in CAP activities, such as the CAP Medical Student Forum, CAP Residents Forum, and CAP Annual Meeting, and developing the CAP Distinguished Medical Student Award, all in efforts to bring the practice of pathology to the attention of medical students and non-pathologist clinical colleagues. Additionally, the PPAHC developed a nationwide group of Pathologist Pipeline Champions whose goal is to raise awareness of the importance of pathology and laboratory medicine within health care. Pipeline Champions serve as role models within their institutions and advocate for pathology by providing opportunities to engage students in pathology through interest groups, mentoring, and clinical experience. Suggested activities circulated to the Pipeline Champions for student engagement are included in Supplemental Material S1. Regardless of which medical specialty is ultimately chosen, students must have a clear understanding of the role of the pathologist and pathology in patient care, as pathology is an integral part of the system of patient care. These recommendations require commitment and dedication from pathologists and pathology professional organizations. If successful, this will lead not only to a rise in matriculation of medical students into the field but also to a better understanding of pathology for all medical students and ultimately better care for patients.
There are limitations to the three surveys that we conducted, including that this is self-reported data. Also, medical school education continues to evolve with many schools having undergone or are currently undergoing major curriculum changes. Pathology experiences in the new curriculum may be different for students going forward than what we have collected at the time of our surveys. However, our research demonstrates that exposure is the key to medical student matriculation into pathology.
Author's notes
John Childs: the views and opinions expressed in this manuscript are those of the author and do not reflect the official policy or position of the Department of Army/Navy/Air Force, Department of Defense, or the United States Government. Barbara Knollmann-Ritschel: the opinions expressed herein are those of the authors and are not necessarily representative of the official policy of the Uniformed Services University of the Health Sciences (USUHS), the Department of Defense (DOD), the United States Army/Navy/Air Force, or the U.S. Government.
Funding
The College of American Pathologists Graduate Medical Education Committee (CAP GMEC) is provided by the College of American Pathologists in the form of educational staff support (authors KJ and AL), travel reimbursement for committee members (authors CBM, MB, JMC, MRG, AMH, BB, MPB, LRD, JKK, BECKR, VGP, CFT, and RDH), and funding for publication.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.acpath.2023.100074.
Appendix A. Supplementary data
The following is the supplementary data to this article.
References
- 1.Smith B.R., Kamoun M., Hickner J. Laboratory medicine education at U.S. Medical schools: a 2014 status report. Acad Med. 2016;91(1):107–112. doi: 10.1097/ACM.0000000000000817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghanchi N.K., Nizamuddin R.N., Qasim A., et al. Perception of pathology as a future career choice among medical Students from Karachi, Pakistan: experience from a private medical school. J Pak Med Assoc. Apr 2017;67(4):627–629. [PubMed] [Google Scholar]
- 3.Ford J., Pambrun C. Exit competencies in pathology and laboratory medicine for graduating medical students: the Canadian approach. Hum Pathol. May 2015;46(5):637–642. doi: 10.1016/j.humpath.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Humphreys H., Stevens N., Leddin D., et al. Pathology in Irish medical education. J Clin Pathol. Jan 2020;73(1):47–50. doi: 10.1136/jclinpath-2019-206033. [DOI] [PubMed] [Google Scholar]
- 5.Lew M. Increasing medical student exposure to pathology by creating an integrated rotation during surgery clerkship. Acad Pathol. 2021;8 doi: 10.1177/23742895211015344. 23742895211015344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magid M.S., Cambor C.L. The integration of pathology into the clinical years of undergraduate medical education: a survey and review of the literature. Hum Pathol. Apr 2012;43(4):567–576. doi: 10.1016/j.humpath.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Masuadi E.M., Mohamud M.S., Alhassan A.M., et al. Factors and determinants of choosing pathology as a future career: results from a multi-institution study. Cureus. Jun 2021;13(6) doi: 10.7759/cureus.15790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fielder T., Watts F., Howden C., Gupta R., McKenzie C. Why choose a pathology career? Arch Pathol Lab Med. Jul 01 2022;146(7):903–910. doi: 10.5858/arpa.2021-0118-OA. [DOI] [PubMed] [Google Scholar]
- 9.George M.R., Johnson K.A., Berg M.P., et al. Factors influencing US osteopathic medical students to choose pathology as a specialty. Acad Pathol. 2022;9(1):100034. doi: 10.1016/j.acpath.2022.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCloskey C.B., Johnson K., Brissette M., et al. Factors influencing US allopathic medical students to choose pathology as a specialty. Acad Pathol. 2020;7 doi: 10.1177/237428952095192. 2374289520951924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu J.H., Gruppuso P.A., Adashi E.Y. The self-directed medical student curriculum. JAMA. Nov 23 2021;326(20):2005–2006. doi: 10.1001/jama.2021.16312. [DOI] [PubMed] [Google Scholar]
- 12.McCloskey CB, Brissette M, Childs JM, et al. How influential are medical school curriculum and other medical school characteristics in students' selecting pathology as a specialty? Acad Pathol. (In press). [DOI] [PMC free article] [PubMed]
- 13.Naritoku W.Y., Timmons C.F. The pathologist pipeline: implications of changes for programs and post-sophomore fellowships-program directors' section perspective. Acad Pathol. 2016;3 doi: 10.1177/2374289516646117. 2374289516646117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Isaacson A.L., Robinson R.A., Samuelson M.I. Creating pathologists from a post-sophomore pathology fellowship: 21 Years and 126 fellows at an academic pathology department. Acad Pathol. 2019;6 doi: 10.1177/2374289519851203. 2374289519851203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacPherson B.R. The pathology student fellowship program at the University of Vermont: 1956-2005. Hum Pathol. Nov 2005;36(11):1168–1171. doi: 10.1016/j.humpath.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Howell L.P., Wahl S., Ryan J., Gandour-Edwards R., Green R. Educational and career development outcomes among undergraduate summer research interns: a pipeline for pathology, laboratory medicine, and biomedical science. Acad Pathol. 2019;6 doi: 10.1177/2374289519893105. 2374289519893105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold C., Booth A., Holloman A., Mirza K., Arnold M., Burgin Teresa B. Long distance learning with a heart. Pathologist. 2021;(73):42–47. [Google Scholar]
- 18.Lilley C.M., Arnold C.A., Arnold M., et al. The implementation and effectiveness of PathElective.com. Acad Pathol. 2021;8 doi: 10.1177/23742895211006829. 23742895211006829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibson B., Bracamonte E., Krupinski E.A., et al. A "pathology explanation clinic (PEC)" for patient-centered laboratory medicine test results. Acad Pathol. 2018;5 doi: 10.1177/2374289518756306. 2374289518756306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magnani B., Harubin B., Katz J.F., Zuckerman A.L., Strohsnitter W.C. See, test & Treat: a 5-year experience of pathologists driving cervical and breast cancer screening to underserved and underinsured populations. Arch Pathol Lab Med. Dec 2016;140(12):1411–1422. doi: 10.5858/arpa.2016-0094-SA. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.