Abstract
Background:
CDC recommendation for treatment of uncomplicated gonorrhea (NG) were revised in December 2020 and include ceftriaxone monotherapy when chlamydial infection was excluded. We evaluated the impact of these revised treatment recommendations using data from a network of STD clinics prior to the change in guidelines.
Methods:
We performed a cross-sectional analysis from 8 STD clinics participating in the STD Surveillance Network from Jan 2015-June 2018 assessing gonorrhea/chlamydia (CT) testing episodes, NAAT results, CT only and NG/CT treatment records, and timing of treatment. We describe the frequency of NG and CT treatment practices and what proportion of patients treated would not have had to receive an anti-chlamydial agent.
Results:
Of 190,589 episodes that occurred during the study period, 67,895 (35.6%) episodes were associated with a treatment record consistent with gonorrhea and/or chlamydia (CT only (n=37,530) or NG/CT (n=30,365)), most (~86%) were prescribed on the same-day as initial testing. Of the 67,895 episodes with corresponding treatment record(s), 42.1% were positive for either NG or CT compared to 3.7% were positive for NG or CT for those not associated with treatment records (n=122,694 episodes). Among 30,365 episodes associated with NG/CT treatment records, monotherapy would only have been indicated for 10.1% (3,081/30,365) of the episodes as they were treated on follow-up and were NG positive and CT negative.
Conclusions:
Treatment was prescribed in one third of NG/CT testing episodes, with the majority provided same day. Despite changes in NG treatment guidelines to ceftriaxone monotherapy, majority of patients would continue to receive an anti-chlamydia agent when treated for gonorrhea in these settings.
Keywords: presumptive, STD clinics, chlamydia, gonorrhea, treatment
Summary
Provision of same-day treatment is common in STD clinic patients being treated for gonorrhea and chlamydia, likely resulting in patients continuing to get dual therapy despite recent treatment guideline changes.
Introduction
Effective NG prevention and control strategies hinge on early diagnosis and treatment to reduce both further transmission and potential sequelae from the infection. Nucleic acid amplification tests (NAATs) have improved the diagnosis of sexually transmitted infections (STIs) but they often have a turnaround time of 48-72 hours, which could lead to delays in therapy and further transmission of infection. As FDA-cleared molecular NAAT point-of-care (POC) tests for NG are not yet widely available, patients who are considered symptomatic should be presumptively treated, defined as the initiation of treatment on the same day of testing but before laboratory confirmation.1 Although presumptive treatment can shorten the average duration of infection and help ensure treatment, it may result in over-treatment and exposures to unneeded antibiotics.2,3
In the United States (US), a high number of reported gonorrhea (NG) cases continue to be observed, with 677,769 reported cases in 2020, representing a 45% increase since 2016.4 Untreated NG infections can lead to serious reproductive complications in women, including adverse birth outcomes and potentially increased acquisition of human immunodeficiency virus (HIV) in both men and women.5-7 Given Neisseria gonorrhoeae’s ability to develop antimicrobial resistance 8, treatment recommendations have changed over the past decade.9-12 Prior to December 2020, the recommended treatment for NG was a combination of two antibiotics – ceftriaxone and azithromycin. 11 This was recommended as a strategy to prevent NG from becoming resistant to ceftriaxone, as well as to treat any possible co-infection with CT. However, several factors, including a greater understanding of ceftriaxone’s pharmacokinetics, decreases in NG’s susceptibility to azithromycin, and antimicrobial stewardship, led to the reevaluation of this recommendation.13 To preserve the effectiveness of azithromycin and doxycycline for other infections, updated guidelines (2020) removed anti-CT agents from treatment of NG if the patient is known to be negative for CT. While this strategy assists in extending the clinical life span of antibiotics and address antimicrobial stewardship, it is important to determine how these changes may influence prescribing practices in clinical settings.
In order to evaluate the effect of revised recommendations, we reviewed data collected in select sexually transmitted disease (STD) clinics prior to the change in NG treatment recommendations. We selected clinic visits where patients were tested for both N. gonorrhoeae and C. trachomatis and reviewed associated treatment records that were consistent with recommended NG and/or CT regimens. Our aim was to describe treatment patterns in STD clinics, the frequency of presumptive treatment, and to determine how many patients treated for NG would not have had to receive an anti-CT agent based on the revised NG treatment guidelines.
Material and Methods
Study population and setting
We conducted a retrospective cross-sectional analysis using data collected as part of routine clinical care from participating STD clinics in the STD Surveillance Network (SSuN). SSuN is comprised of ten state, county, and city health departments that conduct facility-based surveillance in publicly funded, urban STD clinics.
Data Collection
Demographic information (age, sex, race/ethnicity), behavioral characteristics (gender of sex partner(s)), clinical history (presence/absence of symptoms, contact to a partner with an STI, HIV status), NG (both NAAT and gram stain) and CT laboratory tests and results, and treatment provided are collected through the routine course of clinical care and transmitted as part of the SSuN project. For each of these visits, we categorized the patient as symptomatic if they reported having any STD-related symptoms (that could include vaginal/penile/anal discharge, dysuria, genital pain, sores/ulcers, rashes, itching, or foul odor, lower abdominal pain). Patients denying the presence of any of the above-mentioned symptoms were categorized as asymptomatic. If the presence or absence of all these symptoms was not known, the patient was categorized as having an unknown symptom status for that visit. Of the ten jurisdictions funded for SSuN, the following eight STD clinics in six jurisdictions had >80% known symptom status (either reported or denied symptoms) and included: Baltimore, Maryland (two clinics), Minneapolis, Minnesota (one clinic), Multnomah County, Oregon (one clinic), Philadelphia, Pennsylvania (two clinics), San Francisco, California (one clinic), and Seattle, Washington (one clinic).
The period of observation was from January 2015 through June 2018. We identified patients who had ≥ 1 visit where they were tested for both NG and CT using a NAAT and defined that visit as the index visit. For purposes of this analysis, the unit of analysis was an NG/CT testing episode, defined as the period between the index visit and any follow up visits that occurred up to 14 days from the index visit. The 14-day time period was used to capture any treatment that likely would be reasonably related to the index visit testing results. Unique patients could be included more than once if they had more than one NG/CT testing episode during the observation period.
Data Analysis
Descriptive statistics were used to describe patient’s demographics and clinical characteristics. For each NG/CT testing episode, we identified associated treatment records and determined if they were treated for CT only or for NG/CT, based on the 2015 CDC STD Treatment Guidelines.8 Treated for “CT only” was defined as any combination of the recommended regimens for the treatment of chlamydial infections7 (azithromycin 1g orally in a single dose, doxycycline 100mg orally 2x for 7 days, erythromycin base 500mg orally 4x for 7 days, erythromycin ethylsuccinate 800mg orally 4x for 7 days, levofloxacin 500mg orally once daily for 7 days, or ofloxacin 300mg orally 2x for 7 days) without a corresponding NG treatment. We defined having been treated for NG/CT as having been prescribed ceftriaxone 250mg, cefixime 400mg, or gentamicin 240mg plus an anti-chlamydial agent. A small number of episodes (<1%) associated with a treatment used for gonorrhea (e.g., ceftriaxone, cefixime, or gentamicin) but without the antichlamydial agent were included in the analysis.
To describe treatment patterns, we calculated the proportion of episodes associated with a CT only or NG/CT treatment record(s). Of these, we determined the proportion of episodes where patients were treated same-day (treated on the initial testing visit), and the proportion treated at follow-up (treated subsequent to the initial testing visit up to 14 days). Since all clinics have the capacity for gram stain testing, episodes where the results of a gram stain were positive (presence of polymorphonuclear leukocytes and gram negative intracellular diplococci) were identified. Of those episodes with documented presumptive treatment, we calculated the proportion of episodes with “over-treatment” (i.e., prescribed antimicrobials at the initial testing visit but NG and CT NAAT results were negative). We also estimated the proportion of episodes with “under-treatment” (i.e., NG and/or CT positive but did not have a NG/CT treatment record at the index visit or during the follow-up period). To investigate the potential impact of the change in NG treatment recommended, we included only the episodes associated with a treatment for NG/CT and stratified by those treated presumptively and those treated on follow-up. We calculated the proportion of episodes treated at follow up that were known to be NG positive and CT negative since this is the group who would have had the greatest impact of the updated treatment recommendations.
Analyses were conducted overall and for women, heterosexual men (only female sex partners) and gay, bisexual, and other men who have sex with men (MSM). Classification of male sexual behavior/orientation was based on the sex partner’s reported or self-identification of sexual orientation as reported by the patient. Sexual orientation and sex of sex partner data were collected for female patients, and the majority identified as heterosexual women and reported only sex with men. However, due to small sample sizes among the female groups who identified as homosexual or bisexual or among those with missing information, females without regard to the sex of their sex partners are reported. All analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, NC, USA). This analysis was determined to be non-research by the Centers for Disease Control and Prevention.
Results
During the 3.5-year observation period, there were 136,397 unique persons who presented for care accounting for 318,557 clinic visits within the eight SSuN STD clinics. Concurrent NG/CT testing was performed in 67.5%, or 214,895 visits. Based on the approach of bundling index and follow-up visits, there were a total of 201,643 NG/CT testing episodes. We excluded 11,054 episodes or 5.5% of the episodes where gender of sex partners was unknown among male patients (female participants were included regardless of availability of data on gender of sex partners). Our analysis included 190,589 NG/CT testing episodes from 106,708 unique patients. Characteristics of these patients are summarized in Table 1. Briefly, the overall median age was 30 years (interquartile range [IQR]: 25–39 years), though the median age of women was 27 years (IQR = 23-35) compared to 32 years for MSM (IQR = 27–43 years) and 31 years for heterosexual men (IQR = 25-40 years). Half of the MSM (50.6%) were non-Hispanic (NH) White, while the majority of heterosexual men (61.2%) and women (56.0%) were NH Black. Women and heterosexual men represented approximately 60% or more of the clinic populations in Minneapolis (62.9%), Philadelphia (86.2%), and Baltimore (92.4%), while MSM represented approximately half or more in Multnomah County (47.6%), San Francisco (48.9%), and Seattle (64.2%) clinics. Of the 190,589 testing episodes, 75,343 (39.5%) were among MSM, 64,815 (34.0%) were among heterosexual men, and 50,431 (26.5%) were among women.
Table 1.
Characteristics of 106,708 unique patients presenting to STD clinics who were tested at least once for both gonorrhea (NG) and chlamydia (CT), overall and by gender and gender of sex partners, STD Surveillance Network, 2015-2018.
| Demographic and clinical characteristics |
Total Unique Patients (n =106,708) |
MSM (n= 32,126) |
Heterosexual men (n= 42,894) |
Women (n= 31,688) |
||||
|---|---|---|---|---|---|---|---|---|
| # | % | # | % | # | % | # | % | |
| Age group (years) | ||||||||
| <=19 | 6,054 | 5.7 | 681 | 2.1 | 2,096 | 4.9 | 3,277 | 10.3 |
| 20-24 | 19,838 | 18.6 | 4,270 | 13.3 | 7,464 | 17.4 | 8,104 | 25.6 |
| 25-34 | 42,917 | 40.2 | 13,455 | 41.9 | 17,256 | 40.2 | 12,206 | 38.5 |
| 35-44 | 19,033 | 17.8 | 6,548 | 20.4 | 8,018 | 18.7 | 4,467 | 14.1 |
| >=45 | 18,866 | 17.7 | 7,172 | 22.3 | 8,060 | 18.8 | 3,634 | 11.5 |
| HIV positive status | 6,179 | 5.8 | 5,432 | 16.9 | 451 | 1.1 | 296 | 0.9 |
| Race/ethnicity | ||||||||
| Hispanic | 10,962 | 10.3 | 5,246 | 16.3 | 3,293 | 7.7 | 2,423 | 7.6 |
| NH-White | 32,152 | 30.1 | 16,268 | 50.6 | 8,958 | 20.9 | 6,926 | 21.9 |
| NH-Black | 49,252 | 46.2 | 5,244 | 16.3 | 26,268 | 61.2 | 17,740 | 56.0 |
| NH-Asian | 5,395 | 5.1 | 2,365 | 7.4 | 1,337 | 3.1 | 1,693 | 5.3 |
| NH Other* | 8,947 | 8.4 | 3,003 | 9.3 | 3,038 | 7.1 | 2,906 | 9.2 |
| SSuN sites | ||||||||
| Baltimore, MD | 20,598 | 19.3 | 1,572 | 4.9 | 11,384 | 26.5 | 7,642 | 24.1 |
| Minneapolis, MN | 16,895 | 15.8 | 6,265 | 19.5 | 5,579 | 13.0 | 5,051 | 15.9 |
| Multnomah County, OR | 8,769 | 8.2 | 4,176 | 13.0 | 2,834 | 6.6 | 1,759 | 5.6 |
| Philadelphia, PA | 31,363 | 29.4 | 4,336 | 13.5 | 15,759 | 36.7 | 11,268 | 35.6 |
| San Francisco, CA | 18,959 | 17.8 | 9,274 | 28.9 | 5,216 | 12.2 | 4,469 | 14.1 |
| Seattle, WA | 10,124 | 9.5 | 6,503 | 20.2 | 2,122 | 4.9 | 1,499 | 4.7 |
Other includes Alaska Native and American Indian, multi-race, other and unknown race
ACRONYMNS: STD=sexually transmitted disease; MSM=gay, bisexual, and other men who have sex with men;
Overall, approximately 20% of the 190,589 testing episodes were either positive for CT, NG or co-infected (Table 2), with MSM having the highest overall positivity compared to heterosexual men and women. There was considerable variation in NG positivity by gender and gender of sex partner, with 11.5% positivity in MSM compared to 6.2% in heterosexual men and 3.2% in women. Conversely, CT positivity was observed to have less variability among the three groups.
Table 2.
Number of and percent of NG/CT testing episodes among STD clinic patients by pathogen, STD Surveillance Network, 2015-2018.
| Total Episodes (n=190,589) |
Episodes among MSM (n=75,343) |
Episodes among Heterosexual men (n=64,815) |
Episodes among Women (n=50,431) |
|
|---|---|---|---|---|
| # (%) Positive | # (%) Positive | # (%) Positive | # (%) Positive | |
| No infection detected | 153,701 (80.6) | 56,999 (75.7) | 52,724 (81.3) | 43,978 (87.2) |
| CT only | 18,235 (9.6) | 7,048 (9.4) | 6,968 (10.8) | 4,219 (8.4) |
|
NG only
|
14,265 (7.5) | 8,638 (11.5) | 4,014 (6.2) | 1,613 (3.2) |
| Co-infection with NG and CT | 4,388 (2.3) | 2,658 (3.5) | 1,109 (1.7) | 621 (1.2) |
Genital indicates urine or urethral specimens in men; urine or cervical/vaginal specimens in women.
ACRONYMNS: STD=sexually transmitted disease; MSM=gay, bisexual, and other men who have sex with men; NG=gonorrhea; CT=chlamydia
Treatment Patterns
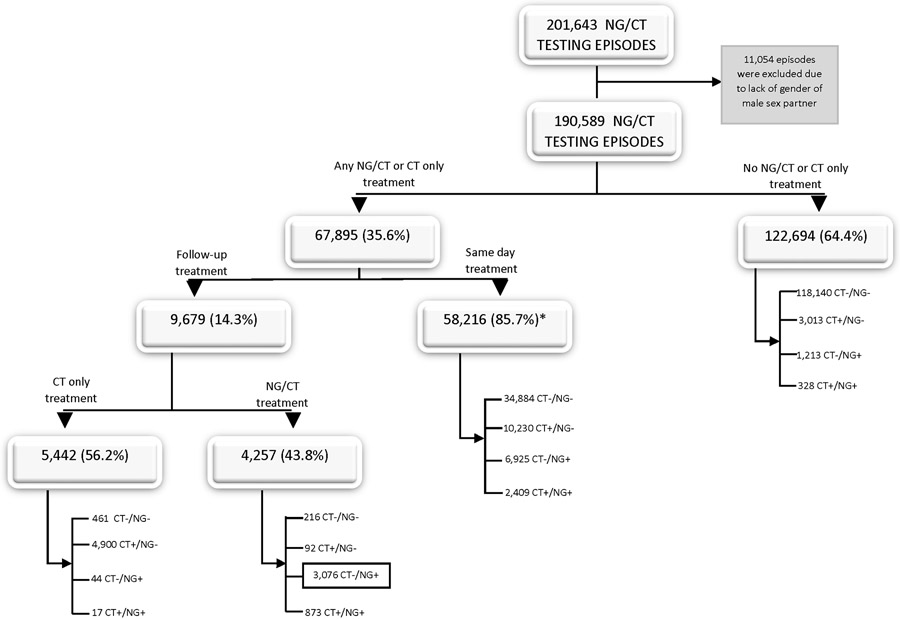
Among all testing episodes, 122,694 (64.4%) were not associated with a NG/CT or CT treatment record within 14 days of being tested. Most of these testing episodes (118,140 or 96.3%) were among patients who did not test positive for either NG and/or CT (Figure 1). However, 3.7% or 4,554 were positive for either or both pathogens.
Figure 1. Results of NG and CT testing and associated treatment among NG and CT testing episodes, STD Surveillance Network, 2015-2018.
*This includes 3,768 testing episodes where a patient had a positive gram stain consistent with a diagnosis of gonorrhea.
ACRONYMNS: NG=gonorrhea; CT=chlamydia
Antimicrobial treatment consistent with treatment of NG/CT or CT only was prescribed in 67,895 or 35.6% of the episodes, of which 58,206 (84.7%) episodes were provided treatment same-day as the index visit and the remaining 9,679 (14.3%) were provided treatment during the follow-up period (Figure 1). Although 58,216 episodes were treated same-day, a small portion 6.5% or 3,768 episodes were among males who had a positive gram stain. These episodes would have technically not been considered presumptively treated as they had laboratory confirmation of infection. The majority (85.9% or 49,992) of the 58,216 episodes either reported symptoms and/or reported being a contact to a partner with an STI. The frequency of presumptive treatment varied between MSM, heterosexual men, and women. Overall, 17.4% (8,798/50,431) of index visits among women, 31.7% (23,876/75,343) among MSM, and 39.4% (25,532/64,815) among heterosexual men included presumptive treatment. When stratified among the episodes where patients reported symptoms and did not report being a contact to STD, presumptive treatment for NG/CT or CT only was still lower among women when compared to her male counterparts (data not shown). However, presumptive treatment for CT only or NG/CT among the episodes where patients reported to be a contact was just as common among women as it was among men (data not shown).
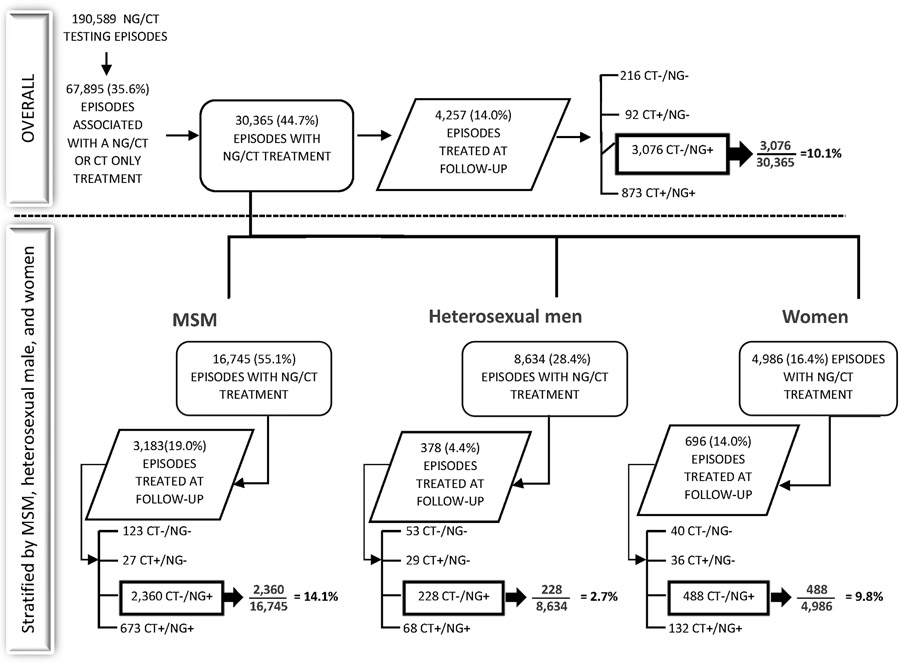
Episodes associated with NG/CT treatment that would have not required an anti-CT agent
Among the 67,895 episodes associated with a treatment record, 44.7% (n= 30,365) were associated with recommended regimens for NG/CT. Over half (55.1%) of these episodes were among MSM, followed by heterosexual men (28.4%) and women (16.4%) (Figure 2). Among these 30,365 episodes, 4,257 (14.0%) were associated with a treatment record during the follow up period. Overall NG/CT test results among the 4,257 episodes as well as stratified by MSM, heterosexual men and women are shown in Figure 2. Under the revised 2020 NG treatment recommendations, 10.1% (3,076/30,365) of the episodes where patients were treated for NG/CT would not have required treatment with an anti-CT agent. When stratified, 14.1% (2,360/16,745) of episodes among MSM would not have required treatment with an anti-CT agent, compared to 9.8% (488/4,986) among women, and only 2.7% (228/8,634) among heterosexual men.
Figure 2. Flowchart of episodes associated with follow up NG/CT treatment by gender and gender of sex partner, STD Surveillance Network, 2015-2018.
ACRONYMNS: NG=gonorrhea; CT=chlamydia
Discussion
Our results demonstrate that when treatment is provided in these clinical settings, it was prescribed more often on the same day of initial NG/CT testing versus after test results were available. Although the overwhelming majority of patients who were treated with an antimicrobial for NG or CT reported having symptoms and/or reported to be a contact to a partner with an STI, men (both heterosexual men and MSM) were presumptively treated more frequently than women. Because presumptive treatment is a frequently preferred paradigm, any changes to treatment practices of uncomplicated NG resulting from the updates to the NG treatment recommendations in late 2020 will likely mean that most SSuN clinic patients treated for NG will still need to be treated with an anti-CT agent, despite the variation observed among MSM, heterosexual men, and women.
Clinicians are often faced with the decision to prescribe treatment ahead of laboratory results. This may be due to the presence of signs and symptoms, risk of STD exposure, or a high index of suspicion for an STI where follow-up is questionable. And while the benefits of this approach can help reduce the burden of disease, as well as continued transmission, it can contribute to potentially unnecessary costs, overtreatment, and adverse personal and social outcomes. 14 In our study we found most of the NG/CT testing episodes associated with presumptive treatment were clinically indicated, yet less than 40% of those showed laboratory evidence of one or both of these infections. This is comparable to other studies, including a study by Rowlinson, et al, who found 55% of individuals were overtreated.2 Another study by Shover found that only 30% of MSM treated presumptively for NG at a sexual health clinic tested positive for NG.15 Despite recommended guidance on when to prescribe presumptive treatment, most recognize the existing challenges in using it to predict STI positivity. These results reinforce the need for more widespread POC assays for NG/CT in STD clinics. In contrast, our study demonstrated a low percentage of undertreatment. It is worth noting that though we showed an undertreatment of >4%, some of those episodes with positive NG and/or CT results could have been treated post 14 days or at an alternative healthcare setting.
In our population of STD clinic patients, we found that women were prescribed presumptive treatment for NG/CT or CT only about half as frequently as their male counterparts. This pattern of males being treated presumptively for NG or CT more often than women has been documented in other studies. In a study conducted by Pugsley, et al found that men were more likely than women to be treated presumptively for NG or CT in both STD and family planning clinics, possibly because of a propensity for infected men to present with symptoms. 3 In another study by Dretler, using data from an academic pediatric emergency department, male patients were more likely to receive empiric treatment and also more likely to have positive test results. 16 One of the reasons cited in published reports may be related to how specific the presence of symptoms are with a suspected infection. 17-19 For example, women reporting non-specific symptoms can be associated with a broader range of differential diagnoses beyond STD concern (e.g., vaginitis, urinary tract infection, pregnancy). Given that our review of treatment was restricted to those that were consistent with treatment for gonorrhea or chlamydia, it is possible that women were treated with other medications during the course of their clinic visit, such as those that may be more warranted in diagnosed conditions such as trichomoniasis, bacterial vaginosis or yeast infections. It is also worth noting that women and men were prescribed presumptive treatment with similar frequencies among episodes where patients reported being a contact to STD only. In addition to symptomology, there are likely many other factors that potentially contribute to the provision of presumptive treatment, including reliability of the performance of the diagnostic assay at the anatomic site tested, local community prevalence, as well as other factors that may influence provider perceptions of risk. These factors may also be contributing factors, but additional studies are needed to better explore this before definitive conclusions can be reached.
Although the updated guidelines recommend use of anti-CT agents only if the patient is known to be negative for CT, given the frequency of presumptive treatment among the SSuN STD clinic population, we have shown in the majority of cases, dual therapy would likely still have been warranted. Currently, there are two FDA-cleared assays for both NG and CT that have been recognized for use at the point of the clinical encounter20, including a recently approved molecular point-of-care (POC) that provide sample to result in 30 minutes.21 Although these tests are authorized for use in multiple healthcare settings, it will likely still take time for more widespread use. Hence, in the short term, many providers will continue to rely on patient report of symptoms and risk exposure, exam findings, and clinical judgement, and as a result, continue to provide dual therapy.
This study has some limitations. First, our study population included STD clinics that primarily capture segments of a population that may be more likely to present with STD-related symptoms when compared to other health care settings. Hence, our results cannot be assumed to apply to the general US population or even to non-STD clinic healthcare setting. Second, data were obtained retrospectively and it is possible the electronic medical record may have missing or inconsistent reporting of clinical variables. Third, we did not look beyond a 14-day window after initial testing, and it is possible that patients could have had a longer lag time to treatment beyond 14 days. Lastly, our calculations may be an underestimate since we did not include those episodes where testing occurred for NG only or for those who were treated but not tested for either pathogen.
This study shows that in a select group of STD clinics, same-day therapy is far more common when compared to treatment following the availability of test results, limiting the impact of revised NG treatment recommendations. Such prescribing practices may limit continued transmission but may come at the expense of overtreatment. Without the on-site capacity to rule-out CT, the majority of patients treated for NG in this setting will likely continue to receive an anti-CT agent. However, the future is promising as technological advances in the area of POC molecular NAAT assays not only have the potential to improve diagnosis and treatment, but provide more timely and targeted prescribing, particularly in the context of these new guidelines.
Table 3.
Gonorrhea (NG)/chlamydia (CT) testing episodes associated with presumptive treatment*, by anatomic site of testing and clinical characteristics, STD Surveillance Network, 2015-2018.
| Anatomic Site of Testing | Clinical Characteristics | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urethral Testing only |
Extragenital Testing only |
Urethral + Extragenital Testing |
Unknown anatomic site |
Symptomatic+ only |
Contact to Partner with STI only |
Symptomatic+ + Contact to Partner with STI |
Not symptomatic+ or Contact to Partner with STI |
|||||||||
| # | % | # | % | # | % | # | % | # | % | # | % | # | % | # | % | |
| MSM (n=21,707) | 2,635 | 12.1 | 1,244 | 5.7 | 17,826 | 82.1 | 2 | 0.01 | 7,631 | 35.2 | 8,277 | 38.1 | 3,557 | 16.4 | 2,242 | 10.3 |
| Heterosexual men (n=23,972) | 12,368 | 51.6 | 159 | 0.7 | 11,437 | 47.7 | 8 | 0.03 | 13,567 | 56.0 | 6,351 | 26.5 | 2,594 | 10.8 | 1,460 | 6.1 |
| Women (n=8,769) | 3,396 | 39.8 | 189 | 2.2 | 5,139 | 60.2 | 45 | 0.5 | 3,041 | 34.7 | 2,893 | 33.0 | 2,081 | 23.7 | 754 | 8.6 |
| Total (54,448) | 18,399 | 34.9 | 1,592 | 2.9 | 34,402 | 65.2 | 55 | 0.1 | 24,239 | 47.0 | 17,521 | 32.2 | 8,232 | 15.1 | 4,456 | 8.2 |
Does not include those episodes among patients who had a positive gram stain.
Symptomatic is defined as STD-related symptoms (including vaginal/penile/anal discharge, dysuria, genital pain, sores/ulcers, rashes, itching, or foul odor, lower abdominal pain).
ACRONYMS: MSM=gay, bisexual, and other men who have sex with men; STI=sexually transmitted infection
ACKNOWLEDGMENTS
The authors wish to acknowledge the contributions of clinic and state and local data managers, epidemiologists, and public health professionals collaborating in SSuN.
Funding
This work was supported by the U.S. Centers for Disease Control and Prevention through cooperative agreement number PS13-1306 (STD Surveillance Network).
Footnotes
Conflicts of Interest
None declared for any authors.
Disclaimer
‘The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.’
REFERENCES
- 1.Barrow RY, Ahmed F, Bolan GA, Workowski KA. Recommendations for Providing Quality Sexually Transmitted Diseases Clinical Services, 2020. MMWR Recomm Rep 2020; 68(5): 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowlinson E, Golden MR, Berzkalns A, et al. Epidemiologic treatment for contacts to Neisseria gonorrhoeae and Chlamydia trachomatis infection in sexually transmitted disease clinic patients in Seattle, WA; 1994 to 2018. Sex Transm Dis. 2020; 47(10): 665–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pusgley RA, Peterman TA. Presumptive and follow-up treatment for gonorrhea and chlamydia among patients attending public health department clinics in Virginia, 2016. Sex Transm Dis. 2019; 46(3): 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2020. Atlanta: U.S. Department of Health and Human Services; 2022. [Google Scholar]
- 5.Pathela P, Braunstein SL, Blank S, Schillinger JA. HIV incidence among men with and without sexually transmitted rectal infections: estimates from matching against an HIV case registry. Clin Infect Dis. 2013; 57(8): 1203–9. [DOI] [PubMed] [Google Scholar]
- 6.Peterman TA, Newman DR, Maddox L, et al. Risk for HIV following a diagnosis of syphilis, gonorrhoea or chlamydia: 328,456 women in Florida, 2000-2011. Int J STD AIDS. 2015; 26(2): 113–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heumann CL, Quilter LA, Eastment MC, et al. Adverse Birth Outcomes and Maternal Neisseria gonorrhoeae Infection: A Population-Based Cohort Study in Washington State. Sex Transm Dis 2017; 44(5): 266–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. Antibiotic resistance threats in the United States, 2019. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. Available from https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf [Google Scholar]
- 9.Workowski KA, Berman S; Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 2010; 59(No. RR-12)1–110. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Update to CDC’s Sexually transmitted diseases treatment guidelines, 2010: oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb Mortal Wkly Rep 2012; 61(31): 590–4. [PubMed] [Google Scholar]
- 11.Workowski KA, Bolan GA; CDC. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015; 64(RR-03): 1–137. [PMC free article] [PubMed] [Google Scholar]
- 12.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021; 70(4): 1–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.St Cyr S, Barbee L, Workowski KA, et al. Update to CDC’s Treatment Guidelines for gonococcal infection, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(50): 1911–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levitt MA, Johnson S, Engelstad L, et al. Clinical management of chlamydia and gonorrhea infection in a county teaching emergency department--concerns in overtreatment, undertreatment, and follow-up treatment success. J Emerg Med. 2003; 25(1): 7–11. [DOI] [PubMed] [Google Scholar]
- 15.Shover CL, Beymer MR, Unger EM, et al. Accuracy of presumptive gonorrhea treatment for gay, bisexual, and other men who have sex with men: results from a large sexual health clinic in Los Angeles, California. LGBT Health. 2018; 5(2): 139–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dretler AW, Trolard A, Bergquist EP, et al. The influence of race and sex on gonorrhea and chlamydia treatment in the emergency department. Am J Emerg Med. 2020; 38(3): 566–70. [DOI] [PubMed] [Google Scholar]
- 17.Wiest Dr, Spear SJ, Bartfield JM. Empiric treatment of gonorrhea and chlamydia in the ED. Am J Emerg Med 2001; 19(4): 274–5. [DOI] [PubMed] [Google Scholar]
- 18.Faricy L, Page T, Ronick M, et al. Patterns of empiric treatment of Chlamydia trachomatis infections in an underserved population. Fam Med. 2012; 44(6): 408–15. [PMC free article] [PubMed] [Google Scholar]
- 19.Anaene M, Soyemi K, Caskey R. Factors associated with the over-treatment and under-treatment of gonorrhea and chlamydia in adolescents presenting to a public hospital emergency department. Int J Infec Dis. 2016; 53: 34–8. [DOI] [PubMed] [Google Scholar]
- 20.Gaydos CA, Melendez JH. Point-by-Point progress: gonorrhea point of care tests. Expert Rev Mol Diagn. 2020; 20(8): 803–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van der Pol B, Tayler SN, Mena L, et al. Evaluation of the performance of a point-of-care test for chlamydia and gonorrhea. JAMA. Netw Open 2020; 3(5): e204819. [DOI] [PMC free article] [PubMed] [Google Scholar]