Fig. 2.
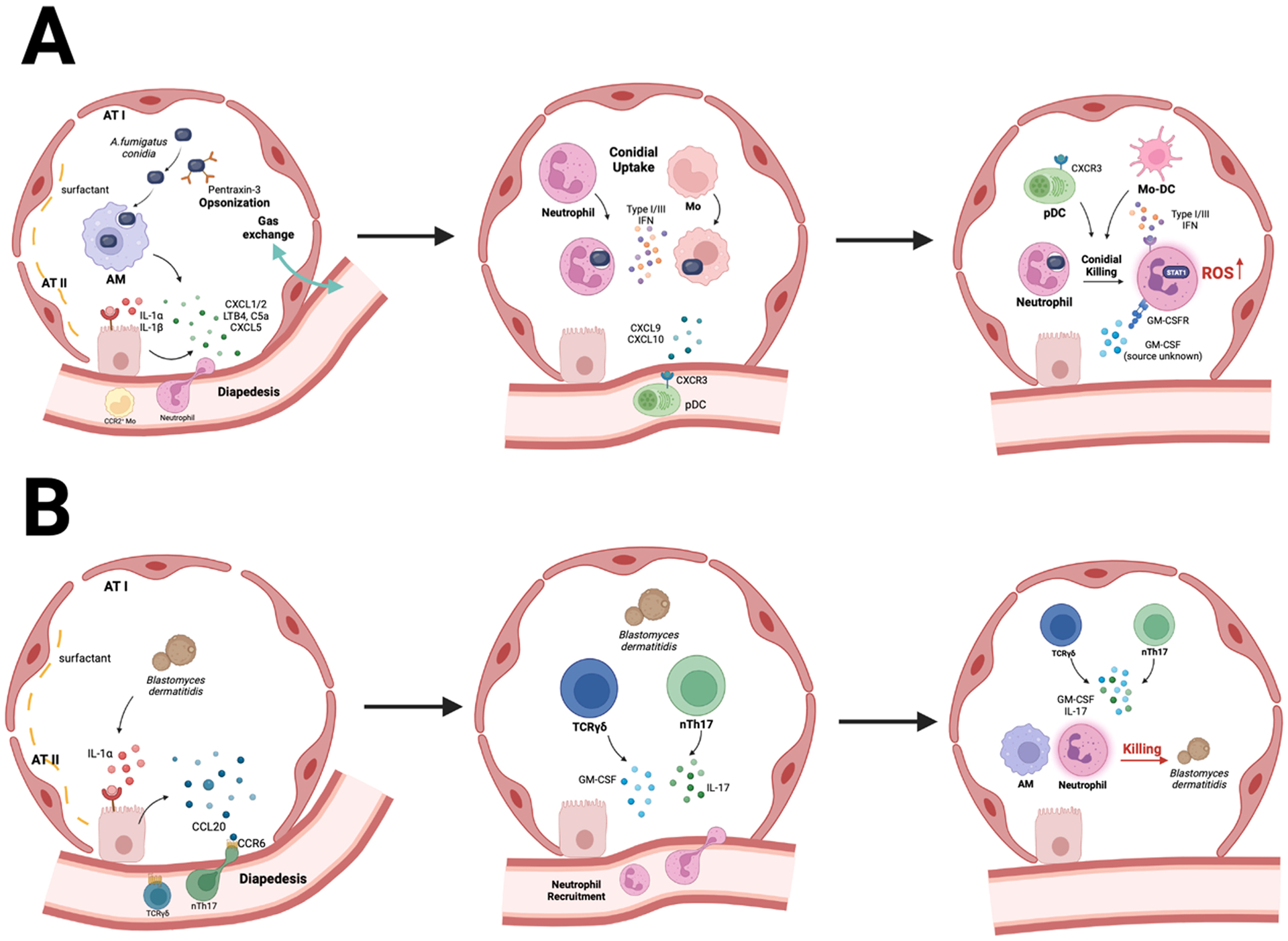
Immune crosstalk is a central feature of pulmonary antifungal immunity. A. Aspergillus conidia induce the rapid release of IL-1 α/β by lung-resident AMs and DCs. This process activates IL-1R/MyD88 signaling in pulmonary epithelial cells which causes the release of neutrophil chemoattractants, primarily CXCL1 and CXCL5. CXC- chemokines collaborate with LTB4, C5a, and galectin-3 to mediate neutrophil influx to infected airways. CCL2, –7, and –12 mediate the ensuing influx of CCR2+ monocytes into the lung parenchyma. Neutrophils, monocytes, and monocyte-derived dendritic cells (Mo-DCs) engulf conidia into phagolysosomes and inactivate fungal cells via products of NADPH oxidase. Monocyte-regulated type I and type III IFNs enhance fungal killing. Fungus-engaged neutrophils and Mo-DCs release CXCL9 and CXCL10 which recruits CXCR3+ plasmacytoid DCs from the circulation into the lung. Plasmacytoid DCs (pDC) do not bind conidia but enhance the oxidative burst to boost conidial killing in neutrophils. GM-CSF enhances this process as well. B. During Blastomyces infection, early IL-1α/β release triggers epithelial CCL20 production which acts on CCR6+ ILCs and mediates their trafficking to the infected lung. ILCs and natural T helper 17 cells produce IL-17 and GM-CSF which potentiate yeast cell killing by neutrophils and Mo-DCs.
