Abstract
Introduction
Traumatic brain injury (TBI) is a leading cause of death and morbidity worldwide. Evidence-based guidelines for managing severe TBI have been available for over 25 years. However, adherence to guidelines remains variable despite evidence highlighting improvement in outcomes with individual recommendations. There is limited evidence to support a superior outcome with compliance to whole sets of recommendations. The aim of this review was to determine whether adherence to TBI guidelines as a package improves outcomes in adults and paediatric patients with severe TBI.
Methods
A structured literature search was conducted using the MEDLINE®, Embase™, PubMed and CINAHL® (Cumulative Index to Nursing and Allied Health Literature) databases. Studies were considered eligible for inclusion in this review if they were quantitative studies investigating the use of TBI guidelines in relation to one or more of the following outcomes: mortality, functional outcome and length of hospital stay.
Results
Nine cohort studies were identified that fulfilled the inclusion criteria and answered the clinical question. A review of these papers was conducted.
Conclusions
Mortality after severe TBI improves with increasing adherence to evidence-based guidelines in both adults and children. The evidence also suggests that compliance with guideline recommendations results in improved functional outcomes and reduced length of hospital stay.
Keywords: Traumatic brain injury, Guidelines, Adherence, Outcome
Introduction
The Brain Trauma Foundation (BTF) first published its evidence-based guideline for severe traumatic brain injury (TBI) in 1996.1 These guidelines have evolved over the last 25 years; they were first updated in 2000, then in 2007 and 2016. The aim of these guidelines is to provide healthcare staff with a comprehensive set of recommendations to support best practice for patients following severe TBI. They have helped reduce variability in TBI care around the world and have become a global standard.2 Guidelines have also been published by other authors3,4 but the BTF guideline is the most widely used.5 A paediatric version was introduced in 20036 and last revised in 2019.7
The current version of the BTF severe TBI guideline includes 28 recommendations, each of which is based on varying levels of evidence.8 Recommendations based on low-quality evidence have been discarded over time. High-quality evidence has increased, although class 1 evidence remains scarce.9 The 2016 guideline contains 18 topics.8 This compares with ten topics in 1996.1 In more recent editions of the guideline, topics such as deep vein thrombosis prophylaxis, brain oxygen monitoring and treatment, infection prophylaxis, cerebrospinal fluid drainage and decompressive craniectomy have been included.
Of the 28 recommendations in the 2016 guideline, there are eight recommendations based on level 1 and level 2a evidence.8 These include three positive treatment recommendations: providing adequate nutrition to reduce mortality, performing early tracheostomy to reduce mechanical ventilation days and performing a larger rather than smaller decompressive craniectomy to improve outcomes. The guideline recommends against the use of steroids, which is the only level 1 recommendation. The other high-quality recommendations advise against the use of seizure prophylaxis for prevention of late post-traumatic seizures and against the prophylactic use of a bifrontal craniectomy in diffuse head injury.8,9 The topics covered in the BTF paediatric guidelines7 are similar to those in the adult guidelines.
There is considerable variability in TBI guideline adherence and implementation among neurotrauma centres in Europe.5 Individual elements of the guidelines have been shown to improve patient outcomes but there remains a lack of evidence to support a superior outcome when adhering to the full package. Two previously published systematic reviews report on guideline adherence but focus on individual recommendations without linking adherence to outcomes.10,11 The authors found adherence was greater for recommendations that were based on high levels of evidence. However, only three recommendations in the current BTF guidelines are based on high-level evidence (levels 1 and 2a).8 Neither review examined guideline adherence in paediatric patients. Evidence of the impact of a combined set of recommendations may improve their implementation, potentially affecting patient outcomes.
The aim of this review was to determine whether adherence to TBI guidelines as a package improves outcomes in adult and paediatric patients with severe TBI. The primary objective was to assess impact on mortality, functional neurological outcome and length of hospital stay. The secondary objective was to assess whether the degree of improvement in outcomes is related to the degree of guideline adherence.
Methods
This review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines.12 An electronic literature search was performed using the MEDLINE®, Embase™, PubMed and CINAHL® (Cumulative Index to Nursing and Allied Health Literature) databases. A combination of free text words and medical subject headings was used. The search terms included (traumatic brain injury OR head injury OR TBI OR brain trauma OR head trauma OR cerebral trauma) AND (guideline OR protocol OR guidance OR recommendation) AND (adher* OR compliance).
The titles and abstracts of these papers were independently screened for relevance by two authors (SD and KMR), and discrepancies were resolved by discussion. Papers published in English were considered and the reference lists of all relevant papers were searched for secondary references. The search was current as of 23 May 2020.
The inclusion and exclusion criteria for studies were:
• Population: Adult and paediatric patients with blunt or penetrating severe TBI, which was defined as those with prolonged unconsciousness following head injury or a Glasgow coma scale score of ≤8.1 Studies that included predominantly military-related TBI were excluded as they are unlikely to reflect the pattern of severe TBI experienced in the civilian population.13
• Intervention: Use of in-hospital TBI guidelines; studies that had, within their design, datasets relating to adherence to guidelines.
• Outcomes of interest: Mortality, functional outcome, length of hospital stay.
• Study design: Quantitative studies published since the first evidence-based guideline for TBI was produced in 1996.1 There were no randomised controlled trials. Cohort studies (both prospective and retrospective) and case-controlled series were considered. Small case series (sample size <30) and case reports were excluded.
Results
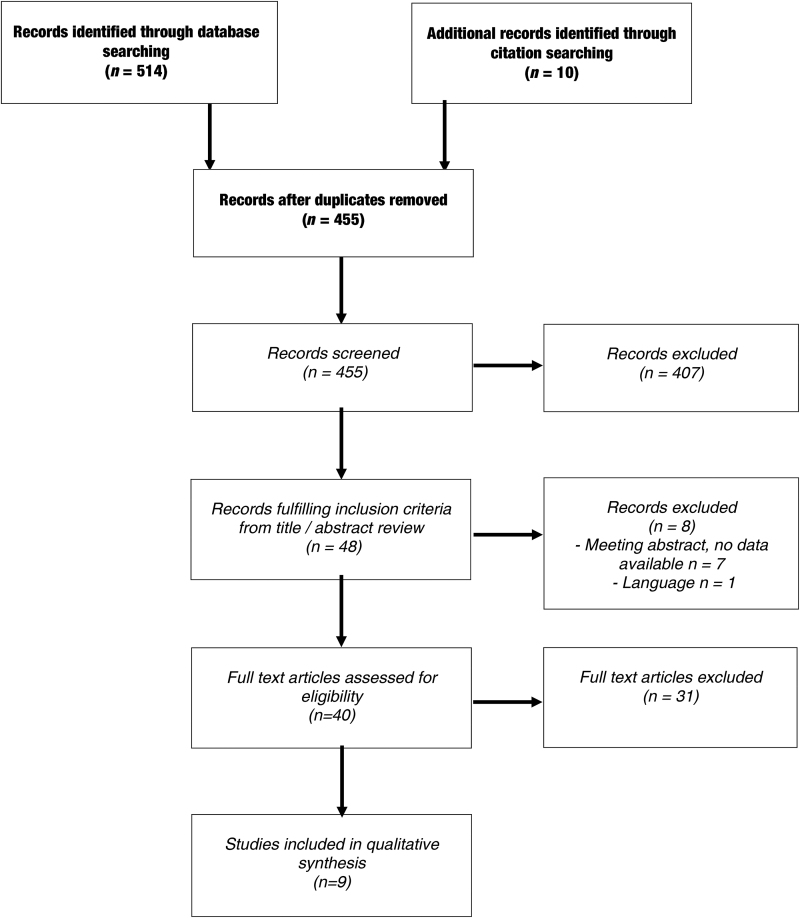
The database search identified 514 articles, and an additional 10 articles were identified from forwards and backwards citation searching of all relevant papers (Figure 1). After excluding duplicates, titles and abstracts were screened, and 40 publications were reviewed in full. Of these, nine papers fulfilled the inclusion criteria, all of which reported prospective or retrospective observational studies. A review of these selected papers was conducted and the results are summarised in Table 1. Each study was assigned a level of evidence based on its quality according to the Oxford Centre of Evidence-Based Medicine.14
Figure 1 .
Flowchart of studies included in review
Table 1 .
Summary of studies reviewed
| Study | Patient group and guideline used | Study type and level of evidence | Outcomes | Key results |
|---|---|---|---|---|
| Fakhry, 2004,15 US | 831 TBI patients aged >14 years, with GCS ≤8 and who lived >48h were compared as 3 groups: • Before protocol (n=219) • Low (50%) protocol compliance (n=188) • High (88%) protocol compliance (n=423) Guideline: Protocol based on BTF guidelines (1996 version) |
Retrospective cohort, single centre Evidence level 3 |
Mortality | Significant reduction in mortality in the high compliance group compared with other groups (p=0.047). |
| Functional outcomes • GOS and RLAS measured at hospital discharge |
Significant improvement in functional outcomes. Increase in proportion of patients with GOS 4–5 in the high compliance group (61.5% high compliance vs 50.3% low compliance vs 43.3% before protocol; p<0.001). RLAS also showed similar trend (p=0.004). | |||
| ICU/hospital LOS | ICU LOS (p=0.021) and total hospital LOS (p=0.005) were reduced in the high compliance group compared with before the protocol was implemented. | |||
| Rusnak, 2007,16 Austria | 405 severe TBI patients were included. Compliance with TBI guidelines was evaluated using a complex scoring system based on the level of evidence for each recommendation. Guideline: BTF guidelines (1996 version) |
Prospective cohort, multicentre Evidence level 4 |
Mortality • ICU survival |
Overall guideline compliance did not affect ICU survival (OR: 1.01). Resuscitation of BP and oxygenation, and maintaining CPP >70mmHg were the only recommendations found to significantly improve ICU survival. |
| Functional outcomes • Favourable (GOS 4–5) vs unfavourable (GOS 1–3) |
Overall guideline compliance did not increase probability of favourable outcome (OR: 1.02). Resuscitation of BP and oxygenation was the only recommendation to significantly improve functional outcome. |
|||
| ICU/hospital LOS | Following all recommendations resulted in an increase in ICU stay and a reduction in total hospital LOS. | |||
| Gerber, 2013,17 US | 2,320 TBI patients who presented within 24h of injury and had GCS ≤8 were included. Patients were grouped by time period: 2001–2003, 2004–2006, 2007–2009. Guideline: BTF guidelines (2000 and 2007 versions) |
Prospective cohort, multicentre Evidence level 2 |
Guideline adherence | General trend of increasing guideline adherence over time. ICP monitoring increased from 55.6% (2001–2003) to 75.2% (2007–2009) (p<0.0001). ICP compliance significantly reduced mortality (p=0.0002). ICP elevations of >25mmHg on days 1 or 2 dropped (p=0.0001). Adherence to CPP treatment thresholds increased over the decade (p<0.0001). |
| Mortality • Case fatality rate at 2 weeks |
Case fatality rate decreased from 22% to 13% over the decade (OR: 0.53, p<0.0001). | |||
| Shafi, 2014,18 US | 2,056 TBI patients with admission GCS ≤8 were included. Guideline: 6 ‘processes of care’ developed based on BTF guidelines (2007 version) |
Retrospective cohort, multicentre Evidence level 4 |
Mortality | Increased compliance with 6 processes of care was associated with a reduced mortality rate (OR: 0.88). Every 10% increase in compliance was associated with a 12% reduction in risk of death. |
| Guideline adherence | Overall mean compliance in the entire study population was 73%. | |||
| Vavilala, 2014,19 US | 236 patients aged <18 years with TBI (GCS ≤8) who were intubated for at least 48h were included. The impact of adherence to guidelines in the first 72h of hospital admission was assessed. Guideline: Paediatric severe TBI guidelines (2003 version) |
Retrospective cohort, multicentre Evidence level 4 |
Mortality | Increasing guideline adherence was associated with better survival (adjusted HR: 0.94). Every 1% increase in adherence resulted in a 6% lower hazard of death. Significant association with increasing compliance up to 60–80%. |
| Functional outcomes • GOS at discharge: favourable (GOS 4–5) vs unfavourable (GOS 2–3) |
Increasing guideline adherence was associated with favourable GOS (adjusted HR: 0.99). Adherence of 40–60% or above was significantly associated with lower rates of unfavourable GOS compared with <20% compliance. | |||
| Lee, 2015,20 US | 185 TBI patients with GCS ≤8 were compared as 3 groups: • Low compliance (<55%) • Moderate compliance (55–75%) • High compliance (>75%) Guideline: BTF guidelines (2007 version) |
Retrospective cohort, single centre Evidence level 3 |
Mortality | Low guideline compliance was a significant predictor of mortality. Reduced odds of mortality were seen in patients with moderate compliance (OR: 0.20) and high compliance (OR: 0.27) compared with low compliance. No significant difference in mortality between the high and moderate compliance groups. |
| Gupta, 2016a,21 India | 200 severe TBI patients aged ≥18 years and alive with tracheal intubation for >48h were compared as 3 groups: • Low compliance (<65%) • Moderate compliance (65–75%) • High compliance (>75%) Guideline: BTF guidelines (2007 version) |
Prospective cohort, single centre Evidence level 3 |
Mortality • Inpatient mortality |
3% reduction in mortality for every 1% increase in guideline adherence (adjusted RR: 0.97, 95% CI: 0.95–0.99). Adherence of <65% was associated with twofold higher inpatient mortality. |
| Gupta, 2016b,21 US | 200 severe TBI patients aged ≥18 years and alive with tracheal intubation for >48h were compared as 3 groups: • Low compliance (<65%) • Moderate compliance (65–75%) • High compliance (>75%) Guideline: BTF guidelines (2007 version) |
Retrospective cohort, single centre Evidence level 3 |
Mortality • Inpatient mortality |
No relationship between guideline adherence rate and inpatient mortality. |
| Reisner, 2018,22 US | 192 TBI patients aged <18 years with GCS ≤8 and who had undergone placement of an ICP monitor were compared as 2 groups: • Pre-guideline (n=71) • Post-guideline (n=121) Guideline: Developed an evidence-based paediatric TBI guideline |
Retrospective cohort, multicentre Evidence level 3 |
Mortality | Mortality rate was significantly lower following implementation of TBI guideline (32% pre-guideline vs 19% post-guideline, p=0.04). |
| Functional outcomes • WeeFIM® score on rehabilitation admission and discharge |
No difference in functional outcome score. | |||
| ICU/hospital LOS | Mean hospital LOS and number of days on a ventilator was similar between groups. | |||
| Vavilala, 2019,23 US | 199 TBI patients aged <18 years, of which 193 (97%) had severe TBI (GCS ≤8). Assessed adherence in the first 72h after diagnosis of severe TBI to three key performance indicators: early initiation of nutrition, avoidance of unwanted hypocarbia and maintenance of CPP (>40mmHg) Guideline: Clinical care pathway based on BTF guidelines for severe paediatric TBI (2012 version) |
Prospective cohort, single centre Evidence level 3 |
Mortality | Adherence to CPP and nutrition targets was significantly associated with higher discharge survival. |
| Functional outcomes • Favourable (discharge home or to a rehabilitation service) vs unfavourable (in-hospital death, or discharge to a nursing or long-term facility) |
Adherence to CPP and nutrition targets was significantly associated with favourable discharge disposition. |
BP = blood pressure; BTF = Brain Trauma Foundation; CI = confidence interval; CPP = cerebral perfusion pressure; GCS = Glasgow coma scale; GOS = Glasgow outcome scale; HR = hazard ratio; ICP = intracranial pressure; ICU = intensive care unit; LOS = length of stay; OR = odds ratio; RLAS = Rancho Los Amigos scale; RR = relative risk; TBI = traumatic brain injury
The included studies were published between 2004 and 2018, and included 6,824 TBI patients.15–23 Seven studies were from the US, and the remaining two were from Austria and India. Five studies were purely retrospective observational studies15,18–20,22 but four collected data prospectively.16,17,21,23 One study had two distinct cohorts: one cohort with prospectively collected data from India and the other with retrospectively collected data from the US.21 These cohorts were treated as two separate groups when analysing the data. Most studies were multicentre (n=6) and all included patients with extracranial trauma.
Adherence and mortality
Eight studies showed that adherence to evidence-based guideline recommendations was associated with a significant reduction in mortality in severe TBI patients.15,17–23 Gerber et al reported a statistically significant reduction in case fatality rate in their prospective observational multicentre study involving 2,347 patients.17 They demonstrated an increasing trend of guideline adherence between 2001 and 2009, and over this time period their case fatality rate reduced from 22.4% to 13.3% (p=0.0001). In a retrospective single-centre study of 831 patients by Fakhry et al, the group that demonstrated 88% compliance with the TBI protocol had a significant reduction in mortality compared with both the low (50%) compliance group and the patient cohort treated before the protocol was implemented (p=0.047).15 Similarly, in a retrospective multicentre study of paediatric patients by Reisner et al, guideline implementation led to a significant mortality reduction (32% pre-guideline vs 19% post-guideline; p=0.04).22
There is also evidence that the degree of guideline adherence correlates with a reduction in mortality. In a retrospective multicentre study involving 2,056 patients, Shafi et al found that for every 10% improvement in guideline compliance, there was a 12% reduction in risk of death.18 Gupta et al reported a 3% reduction in risk of death for every 1% increase in adherence.21 They also found that guideline adherence of <65% was associated with a nearly twofold higher inpatient mortality. Similarly, Lee et al reported that compliance of <55% was a significant predictor of mortality in their retrospective single-centre study.20 In a retrospective multicentre study of paediatric TBI patients, Vavilala et al found mortality rates continued to improve with increasing adherence up to 60–80% compliance, beyond which there was no further improvement.19
Adherence and functional outcome
The relationship between functional outcome and guideline adherence was reported in five studies.15,16,19,22,23 Fakhry et al found a significant improvement in functional outcomes at hospital discharge with increased protocol compliance.15 There were a higher proportion of patients with a Glasgow outcome scale (GOS) score of 4 or 5 in the high-compliance group (61.5% high compliance vs 50.3% low compliance vs 43.3% in cohort before protocol; p<0.001).
Vavilala et al demonstrated a clear association with increased adherence and favourable functional outcomes (GOS 4–5) at hospital discharge.19 They found that compliance with over 40–60% of the guideline was associated with a significantly lower rate of unfavourable outcomes (GOS 2–3) compared with less than 20% guideline compliance.
Another study of paediatric patients by Vavilala et al noted that adherence to a severe TBI clinical care pathway (in particular maintaining cerebral perfusion pressure [CPP] and early initiation of nutrition) was associated with favourable functional outcomes at discharge from hospital.23 The other two studies did not find an association between guideline adherence and functional outcome.16,22
Adherence and intensive care/hospital stay
Three studies investigated the association between length of stay (LOS) and levels of adherence.15,16,22 Fakhry et al found that high guideline compliance resulted in a reduction in mean intensive care unit LOS by 1.9 days (p=0.021) and mean total hospital stay by 5.4 days (p=0.005) compared with before the protocol was implemented.15 However, there was no difference between low and high adherence rates, suggesting a weak association. A prospective multicentre study by Rusnak et al reported a mixed picture.16 They noted that complying with all the guideline recommendations resulted in an increase in intensive care unit LOS but a reduction in total hospital LOS. Reisner et al found that implementation of guidelines for severe TBI did not affect hospital LOS or number of days patients were on a ventilator.22
Specific recommendations
Individual recommendations that had the most significant impact on survival were maintaining blood pressure and oxygentation,16,19 intracranial pressure (ICP) monitoring,17,20,22 maintaining CPP16,17,23 and early nutrition.17,19,23 Recommendations linked to improved functional outcome were maintaining blood pressure and oxygenation,16 and maintaining CPP.19,23
Discussion
This aim of this review was to determine whether adherence to TBI guidelines improves outcome in severe TBI patients. The evidence reviewed clearly demonstrates that compliance with TBI guidelines is associated with a significant reduction in mortality in adult and paediatric patients with severe TBI.15,17–23 Furthermore, increasing guideline adherence correlates with a reduction in mortality. Five studies assessed the influence of guidance adherence on functional outcomes, with three finding a significant improvement in functional outcomes with guideline adherence and two showing no association.15,16,19,22,23 Two large cohort studies found a benefit with guideline adherence and total hospital LOS.15,16
Results from this review suggest that some specific recommendations may have greater weight than others. Maintaining blood pressure and oxygenation, ICP monitoring, maintaining CPP and early nutrition were most frequently associated with improved outcomes. The level of evidence associated with these recommendations is graded as level 2a (nutrition), level 2b (ICP monitoring, CPP monitoring) and level 3 (maintaining blood pressure).8 There does not appear to be a direct link between the quality of evidence supporting a recommendation and its impact on outcomes. Further research to strengthen the evidence base underpinning specific recommendations may be beneficial as increasing adherence has been reported with better levels of evidence.11
This review demonstrates that using multiple recommendations from a guideline can have a combined effect. What is not so clear is whether focusing on a more limited number of recommendations may bring about a similar or greater effect. The current literature does not fully clarify which recommendations when grouped together improve outcomes. Addressing this may lead to the development of more focused guidelines and therefore the potential for easier implementation.24,25
Our findings reinforce some of the themes that have developed in healthcare over the last two to three decades in relation to evidence-based medicine and guideline implementation. Clinical guidelines reduce variation in practice and increase the use of evidence-based interventions.26 Although guidelines may be developed through a consensus approach with a combination of research evidence, clinical experience and economic pragmatism,27 some (such as the BTF guidelines)8 are based primarily on evidence with clear indications of the level of evidence supporting their recommendations.
There are some limitations to this review. All the included studies were prospective or retrospective observational studies. These types of studies are particularly susceptible to bias and confounding; consequently, the results need to be treated with caution.
In the included studies, there was no consistency in the duration of guideline implementation. Two studies looked at the impact of guideline adherence for the first 72 hours19,21 while Gerber et al looked at 10 days of intensive care unit data.17 It remains unclear whether early use alone is beneficial or whether guidelines should be implemented throughout the hospital stay. In standard practice, clinical judgement is used to determine the duration of guideline adherence. Further evidence is needed to inform this debate.
Similarly, in the reviewed studies, no differentiation was made between patients with extracranial trauma and those with isolated TBI. Although outcomes from isolated TBI are widely recognised to be better,28 there is a dearth of knowledge on whether guideline implementation has a similar impact on both of these groups.
Further variation across the studies was noted in how guidelines were introduced, from simple introduction and education19,20 to developing an integrated pathway of care triggered by the diagnosis of severe TBI.15,18,22,23 In some cases, a whole network of hospitals was involved in the implementation of severe TBI guidelines, working in collaboration with the BTF itself, hospital administration teams and clinicians.17 This approach mirrors suggestions that many levels of healthcare need to be involved in implementation to improve engagement and use of guidelines.25,29
Guidelines are likely to have the greatest impact if all appropriate patients are treated using their recommendations.30 Some authors attempted to overcome this by engineering the guidelines into an approach where they were more likely to be used. Reisner et al did this by developing a patient care protocol and using a computerised patient management system.22 Shafi et al developed six ‘processes of care’ that incorporated guidelines into patient treatment, resulting in significantly improved compliance.18 Fakhry et al recommended repeated education and assessment.15 Gerber et al described an integrated programme of implementation involving all levels of healthcare and the guideline developers with regular meetings to assess progress while also linking increased funding to increased adherence.17
We identified several areas of consideration for future research. Few studies have sought to analyse the combination of pre and in-hospital guideline-directed care. Early intervention and arrival in a more stable condition may allow further improvements in hospital care and outcome. The difference in outcomes between isolated severe TBI and severe TBI associated with extracranial trauma is also an area for further research, highlighted by this review. Furthermore, having more knowledge of which recommendations have the greatest influence on outcome and which combinations work to produce cumulative benefits may allow the development of more abbreviated guidelines that are easier to implement.
Conclusions
This review suggests that mortality after severe TBI improves with increasing adherence to evidence-based guidelines in both adults and children. The evidence also suggests compliance with guideline recommendations improves functional outcomes and reduces hospital LOS. There is considerable variability in reported TBI guideline use among neurotrauma centres in Europe.5 Further research to strengthen the evidence base for TBI guidelines and addressing implementation barriers can potentially improve outcomes in patients with severe TBI.
References
- 1.Bullock R, Chesnut RM, Clifton G, et al. Guidelines for the management of severe head injury. Eur J Emerg Med 1996; 3: 109–127. [DOI] [PubMed] [Google Scholar]
- 2.Hirschi R, Rommel C, Letsinger J, et al. Brain Trauma Foundation guideline compliance: results of a multidisciplinary, international survey. World Neurosurg 2018; 116: e399–e405. [DOI] [PubMed] [Google Scholar]
- 3.Joseph B, Friese RS, Sadoun M, et al. The BIG (brain injury guidelines) project: defining the management of traumatic brain injury by acute care surgeons. J Trauma Acute Care Surg 2014; 76: 965–969. [DOI] [PubMed] [Google Scholar]
- 4.Undén J, Ingebrigtsen T, Romner B. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: an evidence and consensus-based update. BMC Med 2013; 11: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volovici V, Ercole A, Citerio G, et al. Variation in guideline implementation and adherence regarding severe traumatic brain injury treatment: a CENTER-TBI survey study in Europe. World Neurosurg 2019; 125: e515–520. [DOI] [PubMed] [Google Scholar]
- 6.Carney NA, Chesnut R, Kochanek PM. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med 2003; 4(Suppl 3): S1. [DOI] [PubMed] [Google Scholar]
- 7.Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the Brain Trauma Foundation guidelines, executive summary. Pediatr Crit Care Med 2019; 20: 280–289. [DOI] [PubMed] [Google Scholar]
- 8.Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 2017; 80: 6–15. [DOI] [PubMed] [Google Scholar]
- 9.Volovici V, Steyerberg EW, Cnossen MC, et al. Evolution of evidence and guideline recommendations for the medical management of severe traumatic brain injury. J Neurotrauma 2019; 36: 3183–3189. [DOI] [PubMed] [Google Scholar]
- 10.Cnossen MC, Scholten AC, Lingsma HF, et al. Adherence to guidelines in adult patients with traumatic brain injury: a living systematic review. J Neurotrauma 2021; 38: 1072–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khormi YH, Gosadi I, Campbell S, et al. Adherence to Brain Trauma Foundation guidelines for management of traumatic brain injury patients and Its effect on outcomes: systematic review. J Neurotrauma 2018; 35: 1407–1418. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed]
- 13.Chapman JC, Diaz-Arrastia R. Military traumatic brain injury: a review. Alzheimers Dement 2014; 10: S97–S104. [DOI] [PubMed] [Google Scholar]
- 14.Centre for Evidence-Based Medicine. OCEBM levels of evidence. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ (cited April 2023). [Google Scholar]
- 15.Fakhry SM, Trask AL, Waller MA, et al. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma 2004; 56: 492–499. [DOI] [PubMed] [Google Scholar]
- 16.Rusnak M, Janciak I, Majdan M, et al. Severe traumatic brain injury in Austria VI: effects of guideline-based management. Wien Klin Wochenschr 2007; 119: 64–71. [DOI] [PubMed] [Google Scholar]
- 17.Gerber LM, Chiu YL, Carney N, et al. Marked reduction in mortality in patients with severe traumatic brain injury. J Neurosurg 2013; 119: 1583–1590. [DOI] [PubMed] [Google Scholar]
- 18.Shafi S, Barnes SA, Millar D, et al. Suboptimal compliance with evidence-based guidelines in patients with traumatic brain injuries. J Neurosurg 2014; 120: 773–777. [DOI] [PubMed] [Google Scholar]
- 19.Vavilala MS, Kernic MA, Wang J, et al. Acute care clinical indicators associated with discharge outcomes in children with severe traumatic brain injury. Crit Care Med 2014; 42: 2258–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JC, Rittenhouse K, Bupp K, et al. An analysis of Brain Trauma Foundation traumatic brain injury guideline compliance and patient outcome. Injury 2015; 46: 854–858. [DOI] [PubMed] [Google Scholar]
- 21.Gupta D, Sharma D, Kannan N, et al. Guideline adherence and outcomes in severe adult traumatic brain injury for the CHIRAG (Collaborative Head Injury and Guidelines) study. World Neurosurg 2016; 89: 169–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reisner A, Chern JJ, Walson K, et al. Introduction of severe traumatic brain injury care protocol is associated with reduction in mortality for pediatric patients: a case study of Children's Healthcare of Atlanta's neurotrauma program. J Neurosurg Pediatr 2018; 22: 165–172. [DOI] [PubMed] [Google Scholar]
- 23.Vavilala MS, King MA, Yang JT, et al. The Pediatric Guideline Adherence and Outcomes (PEGASUS) programme in severe traumatic brain injury: a single-centre hybrid implementation and effectiveness study. Lancet Child Adolesc Health 2019; 3: 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003; 362: 1225–1230. [DOI] [PubMed] [Google Scholar]
- 25.Runnacles J, Roueché A, Lachman P. The right care, every time: improving adherence to evidence-based guidelines. Arch Dis Child Educ Pract Ed 2018; 103: 27–33. [DOI] [PubMed] [Google Scholar]
- 26.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 1993; 342: 1317–1322. [DOI] [PubMed] [Google Scholar]
- 27.Thomas L. Clinical practice guidelines. Evid Based Nurs 1999; 2: 38–39. [Google Scholar]
- 28.Perel P, Arango M, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 2008; 336: 425–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Francke AL, Smit MC, de Veer AJ, Mistiaen Pet al. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 2008; 8: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003; 348: 2635–2645. [DOI] [PubMed] [Google Scholar]