Abstract
Concomitant medial meniscus posterior horn root tears and lateral meniscus posterior horn root tears are rare in occurrence. There is limited literature on the simultaneous repair of medial and lateral meniscus root tears, with ACL reconstruction. We discuss management of concomitant medial meniscus posterior horn root tear (MMPHRT), lateral meniscus posterior horn root tear (LMPHRT), and anterior cruciate ligament (ACL) tear. We highlight the surgical technique in which we perform a repair of both medial and lateral meniscus posterior horn root repairs with ACL reconstruction. We explain the sequence of such a repair to avoid tunnel coalescence.
Technique Video
The patient is in the supine position with the knee in near extension with valgus stress applied. Pie crusting of the medial collateral ligament is performed to improve the visualization of the medial meniscus posterior horn root (MMPHR) tear. FiberTape (Arthrex, Naples, FL) and FiberWire 2-0 (Arthrex) are passed through the remnant of the medial meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew, London UK). The tape and sutures are passed with an antegrade suture passer, working from the anteromedial portal and visualizing from the anterolateral portal. The footprint for the MMPHR is prepared, and a guide wire is passed using a low-profile jig set at 50°. The MMPHR tunnel is reamed with a 4.5-mm reamer. The suture and tape passed through the MMPHR are shuttled out and pulled out through the tibia tunnel. With the MMPHR reduced, three all-inside devices; Fastfix 360 (Smith & Nephew) are used to repair the complex horizontal meniscus tear and the posteromedial junction radial tear. These stitches—two to the posterior capsule and the third to the posteromedial capsule—helps to reinforce the medial meniscus to the posterior capsule. We then proceed to do the LMPHRT repair. In a figure-of-four positions, lateral meniscus posterior root tear is visualized. The footprint of the lateral meniscus root is prepared. FiberTape (Arthrex) and FibreWire 2-0 (Arthrex) are passed through the remnant of the lateral meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew). The FiberTape is introduced through the anteromedial portal and the FiberWire is also introduced through the anteromedial portal (Fig 3C). This is to obtain the best trajectory to pass the suture through good meniscus tissue. A guide wire is inserted at the footprint of the LMPHR using a low-profile jig set at 50°. The LMPHR tunnel is reamed using a 4.5-mm reamer. The FiberTape and the FiberWire pulled out through the LMPHR tunnel. This is followed by ACL reconstruction and passage of ACL graft. The orientation of the tunnel in the proximal tibia from medial to lateral are the MMPHR tunnel, LMPHR tunnel, and ACL tunnel. The medial and lateral meniscus roots are tensioned individually and tied over the cortical button, following which, the ACL graft is fixed with a tibial interference screw.
Introduction
Lateral meniscus posterior horn root tears (LMPHRT) are often traumatic and associated with 7-12% of the patients with ACL tears.1 Medial meniscus posterior horn root tears (MMPHRT) are mainly from chronic degeneration in middle-aged individuals and accounts for 10-28% of medial meniscus tears. Traumatic medial meniscus root tears are uncommon and seen usually with multiligament injuries.2
Meniscus root tears are defined as injuries of the meniscal attachments occurring within 1 cm from their bony insertion to the tibial plateau. The loss of meniscus hoop stresses leads to progressive meniscus extrusion with decreased tibiofemoral contact area and increased contact pressure of the hyaline cartilage in the knee compartment.
It has also been shown that meniscus root tears are associated with high-grade knee laxity and can potentially affect the outcomes of ACL reconstructions. Therefore, when performing an ACL reconstruction, it is important to repair the root tears as well, as this will help protect the ACL graft.
The root of the meniscus can be repaired by various techniques. In the transtibial tunnel pull-out technique, sutures are passed through the remnant root and then pulled out through the tibial tunnels and tied over a button or bony bridge on the tibia.3 Other techniques described involve the use of suture anchors. This requires additional portals for suture anchor placement in the tibial footprint of the meniscus roots and the sutures being passed and tied into the meniscus tissue.4
The purpose of this Technical Note with video is to describe our technique of concomitant repair of medial and lateral meniscus posterior horn root with ACL reconstruction using transtibial tunnel technique (Video 1).
Patient Evaluation, Imaging, and Indication
The history of knee buckling during an injury with an immediate onset of knee swelling suggests an anterior cruciate ligament tear. The emphasis with physical examination is to diagnose patients with high-grade knee laxity. A positive anterior drawer test, Lachman test, and pivot shift test; of grade 2 or more suggests the presence of significant meniscus injury, such as meniscus root tear in addition to ACL injury. This increased suspicion will require surgeons to study the MRIs carefully to exclude a possible meniscus root tear.
Magnetic resonance imaging aids in the preoperative diagnosis of concomitant root tears. It is important to carefully look for features of meniscus root avulsion, where the meniscus root is avulsed from its tibial insertion. This is best seen on the coronal section of MRI. Meniscus extrusion on the coronal MRI, as well as the “ghost sign” on sagittal MRI suggests the possibility of meniscus root tear. All meniscus root tears, which occurs with ACL injury, should be repaired, as the meniscus provides secondary stability to the knee.
Surgical Technique
Positioning
The patient is positioned supine with the operative leg hanging and the other leg in a stirrup leg holder. Using standard anteromedial and anterolateral portals, the surgeon performs a diagnostic arthroscopy. Access to the medial compartment of the knee is improved with a limited medial release using the medial collateral ligament pie-crusting technique.5 The knee is placed in nearly full extension, with a valgus force being applied to obtain maximum visibility and access for the MMPHRT (Fig 1A). For improved visualization and access to the lateral compartment of the knee, the operated limb is placed in the figure-of-4 position, with downward force applied at the level of the knee to open the lateral compartment (Fig 1B). A diagnostic arthroscopy is done to confirm the presence of complex MMPHRT (Fig 2, A and B) and LMPHRT (Fig 3A). Video 1 shows the surgical procedure.
Fig 1.
(A) The position of the left knee (outside picture) for opening the medial compartment while doing the repair of MMPHRT. The knee is in near extension with a valgus force applied to open the medial compartment. MMPHRT, medial meniscus posterior horn root tear. (B) The figure-of-four position of the left knee (outside picture) for opening the lateral compartment for lateral meniscus repair with the foot resting on a side table and pressure being applied over the medial aspect of the left knee to open up the lateral compartment of the knee.
Fig 2.
Medial meniscus posterior horn root (MMPHR) repair of the left knee visualising from the anterolateral portal and working from anteromedial portal with knee in near extension with valgus stress. (A) MMPHRT seen during diagnostic arthroscopy. (B) Complex MMPH tear seen with a radial tear in midbody (C) Preparation of the footprint of medial meniscus posterior root with microcurette. (D) FiberTape being passed through the MMPHR with antegrade suture passer. (E) Tunnel being prepared at MMPHR footprint with a 4.5-mm reamer. (F) Retrieval of monofilament suture to shuttle the meniscus sutures into the tibial tunnel. (G) Reduced MMPHR. (H) Use of an all-inside devices to repair posterior junction radial tear and posterior horn horizontal tear, as well as reinforce the MMPHRT to limit medial extrusion. (I) Reduced MMPHR with sutured post horn of medial meniscus. MFC, medial femoral condyle; MMPH, medial meniscus posterior horn; MMPHR, medial meniscus posterior horn root; MMPHRT, medial meniscus posterior horn root tear.  ; curette,
; curette,  ; Antegrade Suture passer,
; Antegrade Suture passer,  ; Reamer,
; Reamer,  ; Suture retriever,
; Suture retriever,  ; All inside device.
; All inside device.
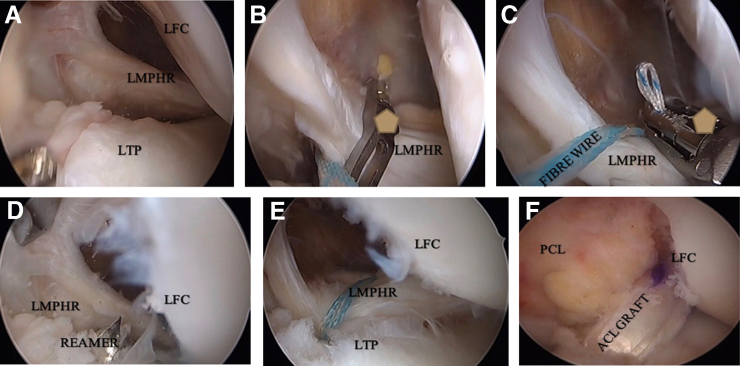
Fig 3.
Lateral meniscus posterior horn root (LMPHR) repair of left knee done in figure-of-four position visualizing from the anterolateral portal and working from the anteromedial portal. (A) LMPHR tear seen during diagnostic arthroscopy visualizing from the anterolateral portal. (B) FiberTape being passed with antegrade suture passer from the anteromedial portal. (C) FiberWire passed through the LMPHR from the anterolateral portal. (D) Tibial tunnel drilled at the footprint of the LMPHR with 4.5-mm reamer. (E) Suture through the LMPHR being pulled out through the tibial tunnel using shuttle suture. (F) Post-ACL reconstruction with the graft in position. LFC, lateral femoral condyle; LTP, lateral tibial plateau; LMPHR, lateral meniscus posterior horn root. Pentagon symbol indicating antegrade suture passing device.
Medial Meniscus Posterior Horn Root Repair
While visualizing from the anteromedial portal and working from the anterolateral portal, the surgeon prepares the medial meniscus posterior root tibial footprint with a microcurette (Fig 2C). High-strength tape, FiberTape (Arthrex, Naples, FL), and high-strength 2-0 suture, Fiberwire (Arthrex) are passed through the remnant of the medial meniscus root using antegrade suture passing device; Firstpass Mini (Smith & Nephew, London UK) (Fig 2D) using a simple suture technique.
The tibial guide wire is inserted using the dedicated low-profile meniscus root repair jig, set at an angle of 50°. This is followed by reaming with a 4.5-mm Endobutton reamer with the wire protected from migration using a microcurette (Fig 2E). The MMPHR tunnel is placed most medially on the anteromedial surface of the tibia, to allow sufficient space for the subsequent LMPHR tunnel, as well as for the ACL tibial tunnel.
The surgeon uses a shuttle relay suture (Fig 2F) to shuttle the sutures in the medial meniscus root through the transtibial tunnel (Fig 2G). All-inside devices, Fastfix 360 (Smith & Nephew, London UK), is used to repair the radial body tear and the posterior horn horizontal tear (Fig 2, H and I). First stitch is to the posterior capsule, and the second is to the posteromedial capsule, to help supplement the transtibial repair.
Lateral Meniscus Posterior Horn Root Repair
In a figure-of-four position with the foot being placed on the side table, a downward force is applied to the knee to open up the lateral compartment(Fig 1B). The lateral meniscus posterior root tear is visualized from the anterolateral portal (Fig 3A) with instruments being passed from the anteromedial portal.
FiberTape (Arthrex) and Fiberwire 2-0 (Arthrex) are passed through the remnant of the lateral meniscus root using an antegrade suture-passing device; First pass Mini (Smith & Nephew) through the anteromedial portal (Fig 3, B and C). This is to obtain the best trajectory for passage of the suture through the good meniscus tissue.
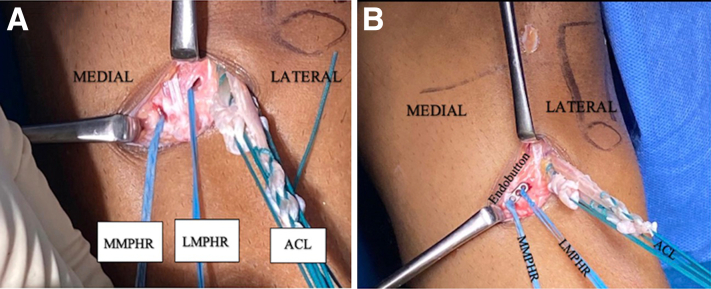
The sutures are then parked in the anteromedial portal. A guidewire is inserted using the dedicated low-profile meniscus root repair jig, setting it at an angle of 50° for the lateral meniscus root tunnel. The LMPHR tunnel is placed lateral to the MMPHR tunnel (Fig 4, A and B). There should be sufficient bone bridge maintained between the medial and lateral meniscus root tunnels (Fig 4B). This is followed by reaming with a 4.5-mm cannulated reamer (Fig 3D), with the wires protected from migration. The sutures from the lateral meniscus root are shuttled into the reamed tunnel (Fig 3E).
Fig 4.
Left knee outside picture showing arrangement of the root repair tunnels and ACL tibial tunnel. (A) Arrangement of the tunnels from medial to lateral of MMPHR, LMPHR, and ACL. Note adequate bony bridge between the tunnels. (B) Sutures from the MMPHR and LMPHR fixed with cortical Endobutton and ACL fixed with aperture fixation with the interference screw. ACL, anterior cruciate ligament; LMPHR, lateral meniscus posterior horn root; MMPHR, medial meniscus posterior horn root.
ACL Tibial Tunnel Preparation
The semitendinosus and gracilis are harvested and quadrupled to obtain an 8.5-mm diameter graft. The ACL tibial tunnel guide wire is passed using an ACL tip aimer guide set at an angle of 55° with the external starting point lateral to both the medial and lateral meniscus root tunnels (Figs 4A and 5). At this point, great care needs to be taken while positioning the tibia tunnel to ensure sufficient bone bridge between the 3 tunnels on the anteromedial surface of the tibia. The ACL tunnel is sited most centrally of the three tunnels, as seen in Fig 5.
Fig 5.
Diagrammatic representation showing arrangement of the tunnels on the tibial side of left knee. From the medial to the lateral side are the MMPHR, LMPHR, and ACL tunnels, respectively. ACL, anterior cruciate ligament; LMPHR, lateral meniscus posterior horn root; MMPHR, medial meniscus posterior horn root.
Fixation of Root Repair and ACL Graft
The sutures from the medial meniscus root, as well as lateral meniscus root, are passed through a cortical button; Endobutton (Smith & Nephew) (Fig 4B), and they are tensioned individually and tied. The medial and lateral meniscus roots are tensioned at 30° of knee flexion with the knee in neutral rotation.6 This is followed by fixation of ACL on the tibial side in 10° of flexion in neutral rotation with an interference screw. The pearls and pitfalls as well as the advantages and disadvantages are mentioned in Table 1 and Table 2 respectively.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Improve access to medial compartment with medial release | Failure to get the suture through good meniscus tissue may result in cut through of the suture through the tissue |
| Use of sutures in simple configuration for meniscus root repair | Malposition of any one of the three tunnels may pose a challenge in drilling the remaining tunnels |
| Use of medial and lateral portal to pass the meniscus sutures for the best trajectory | In osteoporotic bones, high chances of breakage of the bony bridge between the tunnels |
| Choose single tunnel transtibial root repair technique and use small-tunnel diameter | |
| Maintain adequate bony bridge between the tunnels | |
| Change in drilling angle of ACL tunnel compared to meniscus root transtibial tunnels | |
| Use all-inside device to repair to the posterior capsule and offload the root repair site |
ACL, anterior cruciate ligament.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Use of simple sutures reduces the chance of strangulation of the meniscus tissue. | Use of all-inside meniscus repair device to supplement the root repair adds to the cost. |
| With our arrangement of tibial tunnels, it is easier to negotiate the tibial spine. | Use of 3 transtibial tunnels have increased chances of tunnel collision compared to use of suture anchor repair of the meniscus root. |
For initial rehabilitation, the patient needs to be kept on toe touch weight bearing for 6 weeks and followed by full weight bearing after 6 weeks. The knee range of movement is restricted to 90° for the initial 6 weeks, followed by a full range of motion after 6 weeks.
Discussion
Shybut et al. demonstrated that the mean anterior tibial translation of the lateral tibial condyle increased drastically on pivot-shift loading when the lateral meniscus posterior root was avulsed, as compared with an isolated ACL-deficient knee.7 This emphasizes the importance of lateral meniscus root repairs in patients with ACL tears. The presence of high-grade laxity should suggest the presence of significant meniscus injury, and this should caution the surgeon to prepare for meniscus root repair during ACL surgery.
There is a concern of tunnel collision in the tibia when performing an ACL reconstruction and lateral meniscus root repair. Forkel and Petersen suggested excluding the possibility of tunnel collision, the LMPHR sutures were pulled out through the tibial tunnel for the ACL.8 However, this can lead to a nonanatomical repair of the LMPHRT.
Tapasvi et al. recommended drilling independent tunnels for the LMPHR and the ACL graft, with the emphasis on keeping an adequate bony bridge between the two tunnels.9
Feuchet et al. presented a case with concomitant medial and lateral meniscus root injuries along with an ACL tear.10 The medial and lateral meniscus roots were repaired by transtibial pull-out sutures, but the ACL was not reconstructed. They recommended maintaining a bony bridge of 5 mm between the tunnels, as done in our technique.
Bancha et al. have presented a case of simultaneous medial and lateral meniscus root repair with ACL reconstruction.11 To avoid tunnel collision, the medial and lateral meniscus root tunnels were drilled from the anterolateral side of the tibial. Their layout of the tunnels from medial to lateral were the ACL tibial tunnel, the MMPHR tunnel, and the LMPHR tunnel.
In our technique, the arrangement of tunnels from medial to lateral are MMPHR tunnel, LMPHR tunnel, and ACL tibia tunnel (Fig 5). Preparing the tunnels on the anterolateral side, as suggested by Bancha et al., presents a different technical challenge: having to place the tibia guide while avoiding the tibial spines, as well as working under the musculature on the anterolateral tibia. We have shown in our case that the tunnels can be prepared from the anteromedial side of the tibia for such a simultaneous repair.
The emphasis of our technique is the maintenance of an adequate bony bridge between the tunnels and the drilling at different angles to avoid collision of the tunnels. We have positioned the tunnels in the configuration as shown in Fig 5, as it had the least chance for tunnel collision. We use small 4.5-mm tunnels to limit the size of the tunnel, to prevent a collision. Another tip that can be incorporated, which we did not use though, was to use retrograde reamers to ream a socket instead of a full tunnel.12
The use of suture anchors in the repair can also be considered. This is potentially useful, as it obviates the need for full tunnels and the fear of tunnel collision. But it requires additional posterior portals and is technically more demanding.
The suture configuration in root repair can be a simple suture or cinch type. The cinch-type suture has a superior pullout strength compared to a simple configuration. However, cinch sutures can potentially strangulate tissue and affect healing. When placed in good meniscus tissue, a simple suture functions well to bring the meniscus tissue into the tunnel created and is technically less demanding. The clinical outcomes of meniscus root repairs are not influenced by the suture configuration used to repair the root.13 Transtibial pull-out repairs of LMPHRT with concomitant ACL reconstruction have been found to restore translational stability at 2-year follow-up and also reduced meniscus extrusion, which is a risk factor for accelerated knee osteoarthritis.14,15
We often supplement transtibial repair with all-inside repairs to the posterior capsule, as we have done on the medial meniscus. These repairs to the capsule help reinforce the MMPHR repair and offload the transtibial root repair site.16 We feel that this helps reduce retears at the root junction and improves outcomes.
Conclusion
Combined medial and lateral meniscus posterior horn root tear, along with ACL tear, is rare. The simultaneous repair can be achieved with all three tunnels drilled from the anteromedial tibia with a bony bridge of at least 5 mm between the tunnels.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is in the supine position with the knee in near extension with valgus stress applied. Pie crusting of the medial collateral ligament is performed to improve the visualization of the medial meniscus posterior horn root (MMPHR) tear. FiberTape (Arthrex, Naples, FL) and FiberWire 2-0 (Arthrex) are passed through the remnant of the medial meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew, London UK). The tape and sutures are passed with an antegrade suture passer, working from the anteromedial portal and visualizing from the anterolateral portal. The footprint for the MMPHR is prepared, and a guide wire is passed using a low-profile jig set at 50°. The MMPHR tunnel is reamed with a 4.5-mm reamer. The suture and tape passed through the MMPHR are shuttled out and pulled out through the tibia tunnel. With the MMPHR reduced, three all-inside devices; Fastfix 360 (Smith & Nephew) are used to repair the complex horizontal meniscus tear and the posteromedial junction radial tear. These stitches—two to the posterior capsule and the third to the posteromedial capsule—helps to reinforce the medial meniscus to the posterior capsule. We then proceed to do the LMPHRT repair. In a figure-of-four positions, lateral meniscus posterior root tear is visualized. The footprint of the lateral meniscus root is prepared. FiberTape (Arthrex) and FibreWire 2-0 (Arthrex) are passed through the remnant of the lateral meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew). The FiberTape is introduced through the anteromedial portal and the FiberWire is also introduced through the anteromedial portal (Fig 3C). This is to obtain the best trajectory to pass the suture through good meniscus tissue. A guide wire is inserted at the footprint of the LMPHR using a low-profile jig set at 50°. The LMPHR tunnel is reamed using a 4.5-mm reamer. The FiberTape and the FiberWire pulled out through the LMPHR tunnel. This is followed by ACL reconstruction and passage of ACL graft. The orientation of the tunnel in the proximal tibia from medial to lateral are the MMPHR tunnel, LMPHR tunnel, and ACL tunnel. The medial and lateral meniscus roots are tensioned individually and tied over the cortical button, following which, the ACL graft is fixed with a tibial interference screw.
References
- 1.West R.V., Kim J.G., Armfield D., Harner C.D. Lateral meniscal root tears associated with anterior cruciate ligament injury: Classification and management. Arthroscopy. 2004;20:e32–e33. [Google Scholar]
- 2.Kim Y.J., Kim J.G., Chang S.H., Shim J.C., Kim S.B., Lee M.Y. Posterior root tear of the medial meniscus in multiple knee ligament injuries. Knee. 2010;17:324–328. doi: 10.1016/j.knee.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 4.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 5.Da Silva Campos V.C., Guerra Pinto F., Constantino D., Andrade R., Espregueira-Mendes J. Medial collateral ligament release during knee arthroscopy: Key concepts. EFORT Open Rev. 2021;6:669–675. doi: 10.1302/2058-5241.6.200128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okazaki Y., Furumatsu T., Kodama Y., Kamatsuki Y., Masuda S., Ozaki T. Description of a surgical technique of medial meniscus root repair: A fixation technique with two simple stiches under an expected initial tension. Eur J Orthop Surg Traumatol. 2019;29:705–709. doi: 10.1007/s00590-018-2347-z. [DOI] [PubMed] [Google Scholar]
- 7.Shybut T.B., Vega C.E., Haddad J., et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43:905–911. doi: 10.1177/0363546514563910. [DOI] [PubMed] [Google Scholar]
- 8.Petersen W., Forkel P., Feucht M.J., Zantop T., Imhoff A.B., Brucker P.U. Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg. 2014;134:237–255. doi: 10.1007/s00402-013-1873-8. [DOI] [PubMed] [Google Scholar]
- 9.Shekhar A., Tapasvi S., Williams A. Outcomes of combined lateral meniscus posterior root repair and anterior cruciate ligament reconstruction. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221083318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feucht M.J., Salzmann G.M., Pestka J.M., Südkamp N.P., Niemeyer P. Simultaneous avulsion fracture of the posterior medial and posterior lateral meniscus root: A case report and review of the literature. Arch Orthop Trauma Surg. 2014;134:509–514. doi: 10.1007/s00402-013-1915-2. [DOI] [PubMed] [Google Scholar]
- 11.Chernchujit B., Prasetia R. Both Posterior root lateral-medial meniscus tears with anterior cruciate ligament rupture: The step-by-step systematic arthroscopic repair technique. Arthrosc Tech. 2017;6:e1937–e1943. doi: 10.1016/j.eats.2017.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Osti M., Krawinkel A., Hoffelner T., Benedetto K.P. Quantification of tibial bone loss in antegrade versus retrograde tunnel placement for anterior cruciate ligament reconstruction. Int Orthop. 2015;39:1611–1614. doi: 10.1007/s00264-015-2668-z. [DOI] [PubMed] [Google Scholar]
- 13.Ulku T.K., Kaya A., Kocaoglu B. Suture configuration techniques have no effect on mid-term clinical outcomes of arthroscopic meniscus root repairs. Knee. 2020;27:676–682. doi: 10.1016/j.knee.2020.04.017. [DOI] [PubMed] [Google Scholar]
- 14.Li M., Li Z., Li Z., et al. Transtibial pull-out repair of lateral meniscus posterior root is beneficial for graft maturation after anterior cruciate ligament reconstruction: A retrospective study. BMC Musculoskel Disord. 2022;23:445. doi: 10.1186/s12891-022-05406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okazaki Y., Furumatsu T., Kamatsuki Y., et al. Transtibial pullout repair of the lateral meniscus posterior root tear combined with anterior cruciate ligament reconstruction reduces lateral meniscus extrusion: A retrospective study. Orthop Traumatol Surg Res. 2020;106:469–473. doi: 10.1016/j.otsr.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Buckley P.S., Kemler B.R., Robbins C.M., et al. Biomechanical comparison of 3 novel repair techniques for radial tears of the medial meniscus: The 2-tunnel transtibial technique, a "hybrid" horizontal and vertical mattress suture configuration, and a combined "hybrid tunnel" technique. Am J Sports Med. 2019;47:651–658. doi: 10.1177/0363546518816949. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is in the supine position with the knee in near extension with valgus stress applied. Pie crusting of the medial collateral ligament is performed to improve the visualization of the medial meniscus posterior horn root (MMPHR) tear. FiberTape (Arthrex, Naples, FL) and FiberWire 2-0 (Arthrex) are passed through the remnant of the medial meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew, London UK). The tape and sutures are passed with an antegrade suture passer, working from the anteromedial portal and visualizing from the anterolateral portal. The footprint for the MMPHR is prepared, and a guide wire is passed using a low-profile jig set at 50°. The MMPHR tunnel is reamed with a 4.5-mm reamer. The suture and tape passed through the MMPHR are shuttled out and pulled out through the tibia tunnel. With the MMPHR reduced, three all-inside devices; Fastfix 360 (Smith & Nephew) are used to repair the complex horizontal meniscus tear and the posteromedial junction radial tear. These stitches—two to the posterior capsule and the third to the posteromedial capsule—helps to reinforce the medial meniscus to the posterior capsule. We then proceed to do the LMPHRT repair. In a figure-of-four positions, lateral meniscus posterior root tear is visualized. The footprint of the lateral meniscus root is prepared. FiberTape (Arthrex) and FibreWire 2-0 (Arthrex) are passed through the remnant of the lateral meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew). The FiberTape is introduced through the anteromedial portal and the FiberWire is also introduced through the anteromedial portal (Fig 3C). This is to obtain the best trajectory to pass the suture through good meniscus tissue. A guide wire is inserted at the footprint of the LMPHR using a low-profile jig set at 50°. The LMPHR tunnel is reamed using a 4.5-mm reamer. The FiberTape and the FiberWire pulled out through the LMPHR tunnel. This is followed by ACL reconstruction and passage of ACL graft. The orientation of the tunnel in the proximal tibia from medial to lateral are the MMPHR tunnel, LMPHR tunnel, and ACL tunnel. The medial and lateral meniscus roots are tensioned individually and tied over the cortical button, following which, the ACL graft is fixed with a tibial interference screw.
The patient is in the supine position with the knee in near extension with valgus stress applied. Pie crusting of the medial collateral ligament is performed to improve the visualization of the medial meniscus posterior horn root (MMPHR) tear. FiberTape (Arthrex, Naples, FL) and FiberWire 2-0 (Arthrex) are passed through the remnant of the medial meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew, London UK). The tape and sutures are passed with an antegrade suture passer, working from the anteromedial portal and visualizing from the anterolateral portal. The footprint for the MMPHR is prepared, and a guide wire is passed using a low-profile jig set at 50°. The MMPHR tunnel is reamed with a 4.5-mm reamer. The suture and tape passed through the MMPHR are shuttled out and pulled out through the tibia tunnel. With the MMPHR reduced, three all-inside devices; Fastfix 360 (Smith & Nephew) are used to repair the complex horizontal meniscus tear and the posteromedial junction radial tear. These stitches—two to the posterior capsule and the third to the posteromedial capsule—helps to reinforce the medial meniscus to the posterior capsule. We then proceed to do the LMPHRT repair. In a figure-of-four positions, lateral meniscus posterior root tear is visualized. The footprint of the lateral meniscus root is prepared. FiberTape (Arthrex) and FibreWire 2-0 (Arthrex) are passed through the remnant of the lateral meniscus root using an antegrade suture passing device; Firstpass Mini (Smith & Nephew). The FiberTape is introduced through the anteromedial portal and the FiberWire is also introduced through the anteromedial portal (Fig 3C). This is to obtain the best trajectory to pass the suture through good meniscus tissue. A guide wire is inserted at the footprint of the LMPHR using a low-profile jig set at 50°. The LMPHR tunnel is reamed using a 4.5-mm reamer. The FiberTape and the FiberWire pulled out through the LMPHR tunnel. This is followed by ACL reconstruction and passage of ACL graft. The orientation of the tunnel in the proximal tibia from medial to lateral are the MMPHR tunnel, LMPHR tunnel, and ACL tunnel. The medial and lateral meniscus roots are tensioned individually and tied over the cortical button, following which, the ACL graft is fixed with a tibial interference screw.