Table 1.
General considerations and reports on antidepressant-induced adverse effects during pregnancy and lactation.
| Medication | Structure | General considerations and reports on adverse effects |
|---|---|---|
| SSRI | ||
| Fluoxetine (Prozac) |

|
Earlier studies indicated minor malformations in neonates. Colic, seizures, irritability, withdrawal symptoms, and cyanosis during lactation. Long half-life with the stereoselective disposition of fluoxetine and norfluoxetine in the mother, fetus, breast milk, and infant |
| Paroxetine (Paxil) |

|
Temporary neonatal respiratory distress associated with late third trimester. Potential to increase risk in cardiovascular malformations. No adverse effects have been reported during lactation. With short half-life and high protein binding difficulty accounts for its small excretion in milk or negligible infant serum concentrations |
| Fluvoxamine (Luvox) |
|
With limited data, it is not associated with an increased risk of malformations, lower birth weights, or younger gestational age and adverse effects. Shortest half-life among all SSRIs |
| Sertraline (Zoloft) |

|
Not associated with increased risk of malformations, lower birth weights, or younger gestational age and adverse effects. Negligible effect on platelet serotonin transport in breastfed infants |
| Citalopram (Celexa) |

|
Rate of congenital anomalies was no higher than that for other SSRI exposures. Irritability, restlessness, uneasy sleep during lactation decreased feeding. Concentrations in milk is higher than in maternal plasma |
| Escitalopram (Lexapro) |
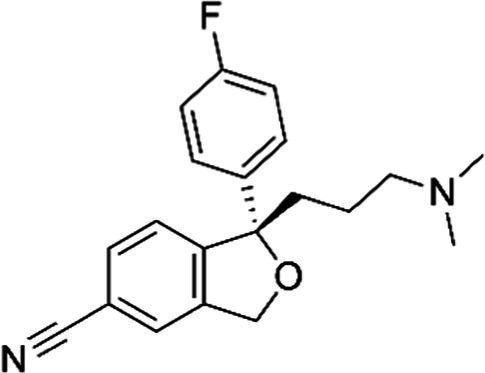
|
Active S-isomer of citalopram. Low potential for causing adverse effects as limited information indicates that maternal doses produce low levels of milk |
| SNRI | ||
| Venlafaxine (Effexor) |

|
Infants receive venlafaxine and its active metabolite in breastmilk; however, concurrent side effects have rarely been reported. Breastfed infants should be monitored for excessive sedation and adequate weight gain with moderate effects of neonatal withdrawal syndrome in infants exposed to the drug during pregnancy |
| Desvenlafaxine (Pristiq) |

|
Venlafaxine’s metabolite. Neonates exposed late in the third trimester may require respiratory support. Breastfed infants should be monitored for excessive sedation and adequate weight gain |
| Milnacipran (Savella) |

|
Unavailable data |
| Tricyclic antidepressants | ||
| Nortriptyline (Aventyl) |
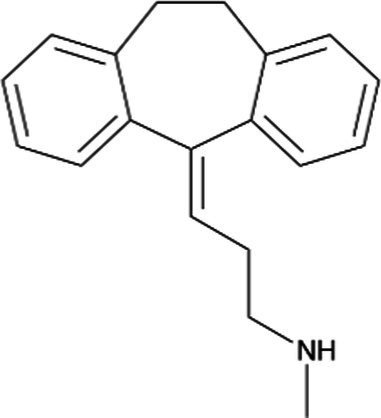
|
Less anticholinergic, consequently less orthostatic hypotension and constipation |
| Imipramine (Trofanil) |
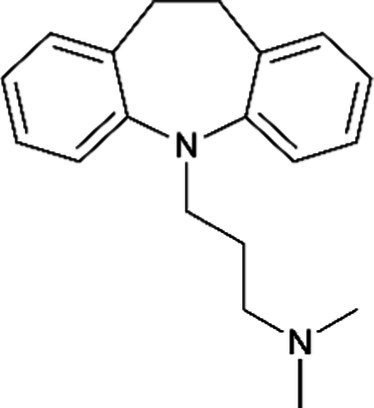
|
There have been clinical reports of congenital malformations. Limited data suggest that imipramine is likely to be excreted in human breast milk |
| Monoamine oxidase inhibitors | ||
| Isocarboxazid (Marplan) |
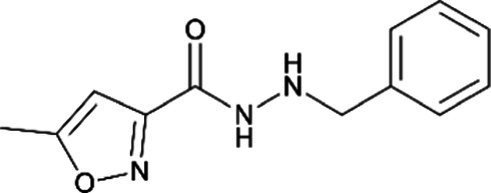
|
Interacts with some medications and foods to cause a life-threatening hypertensive crisis |
| Phenelzine (Nardil) |
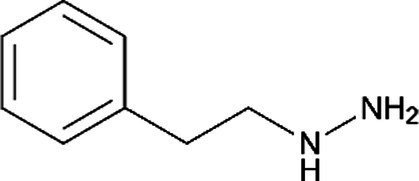
|
Interacts with some medications and foods to cause a life-threatening hypertensive crisis |
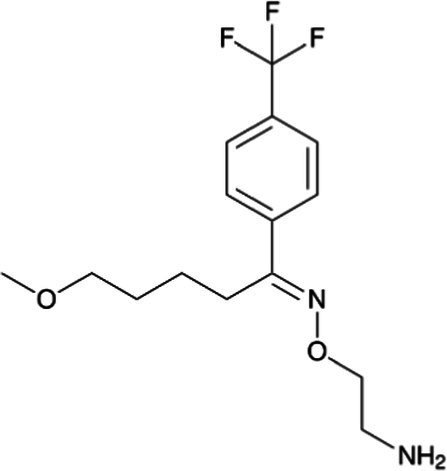
| Others | ||
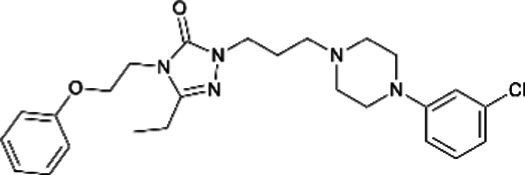
| Trazodone (Donaren) |

|
No differences in the rate of major malformations |
| Nefazodone (Serzone) |
|
No differences in the rate of major malformations |
| Mirtazapine (Remeron) |

|
No adverse effects in infants have been reported |
| Bupoprion (Wellbutrin) |
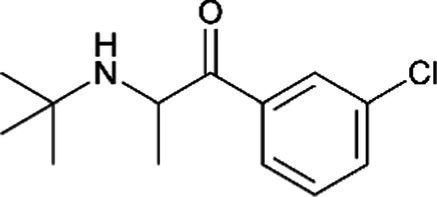
|
Increased risk of seizure, especially in those with a history of seizure. Limited information indicates that maternal bupropion daily produces low levels in breastmilk. Hence, more information about its use is needed |
Some of these reports still have limited clinical trials, or child outcomes, and underpowered samples. SSRIs, selective serotonin reuptake inhibitors; SNRIs, serotonin norepinephrine reuptake inhibitors (34–39). All structures were designed from the name found in literature data using the ChemDraw JS program.
