Figure 6.
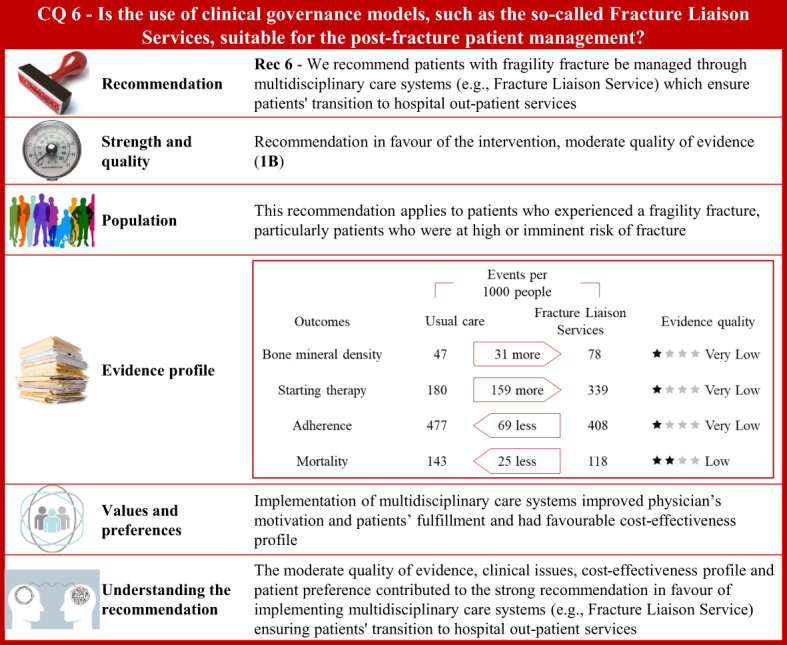
Visual summary for CQ6 (Is the use of clinical governance models, such as the so-called Fracture Liaison Services, suitable for patients’ post-fracture management)?. Rationale. Patients who experienced a fragility fracture should receive correct care planning after hospital discharge to ensure continuity of care through shared diagnostic-therapeutic pathways (284). According to the Fragility Fracture Network (285), global multidisciplinary collaborations should be carried out to improve the care of patients with fragility fractures (286). The Fracture Liaison Service (FLS) is a model of care designed to prevent recurrent fractures (44, 287–289) with coordinated strategies (290) and achieve optimal adherence to anti-osteoporotic medications (291, 292). The multidisciplinary team should be formed by the bone specialist (FLS coordinator), the orthopaedic surgeon, and the specialized bone nurse (43, 293, 294). Through updates of the most recently published systematic reviews on this issue (290, 295–298), and specific manual research, our systematic review included 77 publications on multidisciplinary care systems, such as nurse-led clinics, structured service delivery models, and FLS (299–375). Bone mineral density values, anti-osteoporotic therapy initiation, adherence to anti-osteoporotic therapy, and (re)fracture and mortality risk were the outcomes of interest. Clinical benefits. Compared with usual care, the multidisciplinary programs significantly increased body mineral density values, initiation to anti-osteoporotic treatment, and adherence to anti-osteoporotic therapy. Moreover, these coordinated models showed a reduction of fractures and a significant decrease in mortality risk. Quality of evidence was very low for body mineral density values, initiation to anti-osteoporotic treatment, and adherence to anti-osteoporotic therapy, and low for mortality rate. Values and preferences. Physicians’ motivation in implementing FLS is justified given barriers in treating fractures, gaps in osteoporosis knowledge, and difficulty in managing patients presenting with a fragility fracture observed by healthcare professionals (376). Chinese orthopaedic surgeons reported low sensitivity to the concept of fracture prevention as well as in the effectiveness of preventive measures for fragility fractures (377). Only 25% of patients who contacted their physician received anti-osteoporotic treatment, according to an RCT (378). Conversely, 61% of subjects with a low-trauma fracture were treated with an anti-osteoporotic medication according to a study investigating performance of FLS (Yates 2015) (379). However, the included studies considered various healthcare settings; thus, resource requirements might have limited generalizability across different countries. A decreased refracture risk and favourable cost-effectiveness profile of FLS models compared to usual care was reported from a systematic review evaluating FLS programs in the Asia-Pacific region (298). Compared to usual care or no treatment, FLS resulted in a favourable cost-effectiveness profile from another systematic review (Wu 2018) including osteoporotic patients aged 50 and above from Canada, Australia, the US, UK, Japan, Taiwan, and Sweden (380). FLS-based management of fragility fractures had been reported to be cost-effective in Canada with the reduction of subsequent hip fractures and a net hospital cost savings (381). The implementation of hip FLS co-managed by a nurse and physician showed a $54 incremental cost/patient with a modest gain of eight QALYs/1,000 patients (382). For every 10,000 patients that participated in FLS, an additional 400 patients would be treated with bisphosphonates, resulting in the avoidance of around four hip fractures. Furthermore, the proportion of patients who appropriately received bisphosphonate treatment increased in the year following fracture, from 4.3% to 17.5% (383). The FLS implementation in the USA resulted in 153 fewer fractures, 37.4 QALY gained, and $66,879 in cost savings for every 10,000 patients (384). An FLS implemented in UK was estimated to prevent at least 18 fractures and save £21,000 for every 1,000 patients (385). FLS organizations ensure that patients, affected by osteoporosis or fractures, receive appropriate evaluation and treatment (386, 387) although failures in entry registration, male gender, frailty, education level, living alone, or lack of motivation could be independent factors for FLS non-attendance (388). Additional potential barriers include lack of communication between patients and physicians or the need for patient education intervention (389). Some patients might refuse treatment because of concerns with costs or side effects. Thus, person-centred care should support the interaction between patients and healthcare professionals (389). Understanding the recommendation. The moderate quality of evidence, clinical issues, cost-effectiveness profile, and patient’s preference contributed to the strong recommendation in favour of implementing multidisciplinary care systems (e.g., Fracture Liaison Service) ensuring patients’ transition to hospital outpatient services.
