Figure 6:
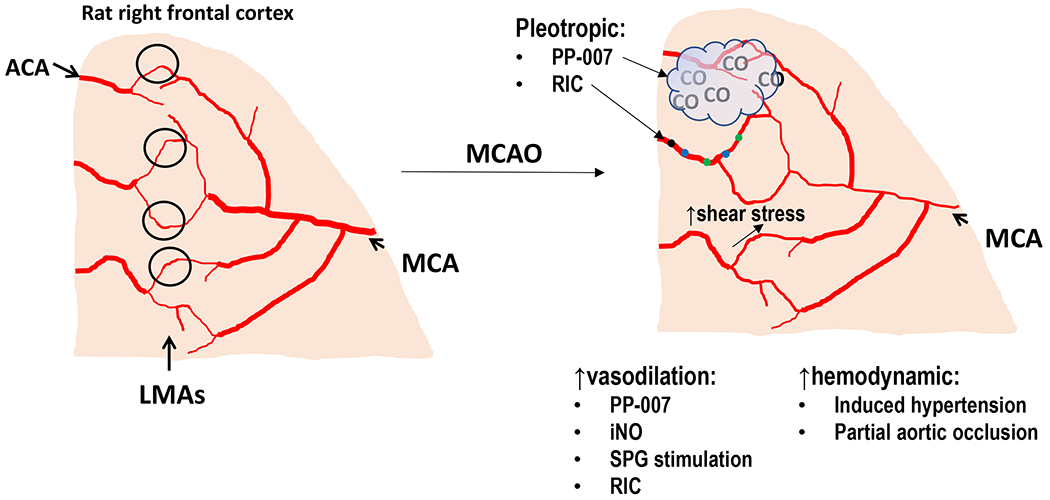
Summary of known and potential mechanisms of collateral enhancing therapies. (A) Diagram of the pial surface of the cortex showing branches of the MCA and ACA. LMAs are distal connections between these arterial territories (black circles). Under normal physiological conditions, there is little flow and shear stress within LMA due to a lack of pressure differential between MCA and ACA. As shown, LMAs are larger in diameter than pial arterioles that do not anastomose. (B) During MCAO, distal branches of the MCA are smaller in diameter due to proximal occlusion that decreases pressure and flow. Also shown are collateral enhancing therapies and potential mechanism by which collateral flow increases. They can be categorized into vasodilators that increase collateral flow through LMA vasodilation or hemodynamically increasing flow through increased cerebral perfusion pressure. Some therapies have multiple beneficial effects (pleotropic). PP-007 causes vasodilation of LMAs and also releases small amounts of CO gas that has anti-inflammatory effects. RIC also increases collateral flow through increased circulating humoral factors and enhanced peripheral immune system activity that likely has other beneficial effects on mitigating ischemic injury. Flow and shear stress are also potent vasodilators that increases collateral flow during MCAO. Flow-induced dilation appears mediated by shear stress-induced activation of TRPV4, NO and IKCa channels.
