The paper by Robin Greinert et al. [1] touches upon a topic that is increasingly attracting interest from different perspectives (e.g. neurology, nephrology, ethics), but that at the same time is still in need of more focused and deeper analysis. To illustrate its relevance, the connection between chronic kidney disease (CKD) and cognitive impairment (CI) is the subject of an ongoing COST Action (CONNECT, Cognitive Decline in Nephro-Neurology, https://connectcost.eu/) which is devoted to clarifying the causal mechanisms of cognitive decline in CKD in order to improve its clinical treatment, in terms of both prevention and care.
The paper by Greinert and colleagues reports the result of an interview study involving 62 patients, which shows a high prevalence of CI associated with decreased mobility and muscle strength, increased frailty, and reduced Health Related Quality of Life (HRQoL). Importantly, the research by Greinert et al. sheds new light on the relationship between CI and frailty, which, among other things, is key in order to plan appropriate clinical and therapeutic approaches. The clinical translation of these data is still to be considered, but results like these are important to plan relevant strategies.
In order to maximize the effectiveness of these plans, it is necessary to implement a multi-disciplinary collaboration (see Fig. 1), including neuroscientific research on the molecular and cognitive dimensions of CI, neurological and neuro-psychological assessments of related physiological and behavioral factors, nephrological research on the relevant pato-pshysiological mechanisms, and ethico-legal reflection on the emerging ethical and regulatory issues.
Figure 1:
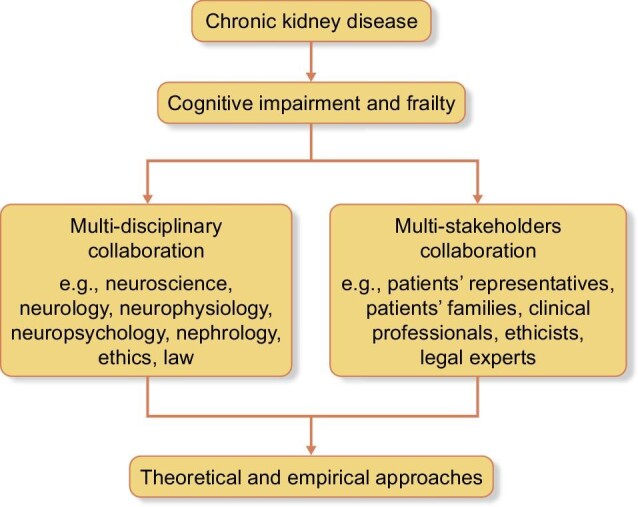
A model for addressing ethical and legal issues arising from CKD.
A preliminary condition for this kind of multi-disciplinary approach is a specific conceptual clarification of key terms, which are relevant to all the involved disciplines but risk being interpreted differently and eventually giving rise to mutual misunderstanding. Frailty in particular deserves specific attention.
The classical definition of frailty is as a syndrome of decreased physiologic reserve characterized by functional decline in different physiological systems and reduced capacity to resist to stressors [2, 3]. The data collected by Greinert et al. confirm that frailty is associated with some indicators of reduced healthy condition, like increased risk of falls, hospitalizations, CI, reduced HRQoL and even mortality [4].
Since the availability of kidneys for transplantation does not meet the need for organs actually required, some criteria for including patients in kidney transplantation list and for setting priorities among them are necessary. Frailty and CI are increasingly used for this purpose [5–7].
One possibility is referring to frailty and CI to select and prioritize patients within a utilitarian framework, for instance giving priority to less frail and younger patients with life expectancy and potential quality of life that at first glance are better. Yet things are not so straightforward. In fact, data indicate that ‘Frailty is more prevalent among older hemodialysis patients, KT candidates, and KT recipients; however, there is a high prevalence of frailty among younger patients as well’ [3]. Furthermore, the fact that post-transplant outcome is overall worse for frail patients is importantly counterbalanced by the fact that sometimes frailty is improved in transplanted patients. In fact, the assessment of frailty at evaluation and/or during transplantation admission combined with appropriate clinical management significantly improve the rate of positive outcome [8].
The above raises a clinical as well as an ethical concern: frailty cannot be assumed as an absolute factor in deciding about the patient's inclusion in the transplantation waitlist, because such a condition may be improved by the transplantation itself. Therefore, a multi-perspective (e.g. involving professionals, patients’ associations and patients’ families) and multi-disciplinary reflection is needed, and additional factors should be evaluated in making a final decision about the transplantation.
Like frailty, also CI is increasingly used to place patients on waitlists and to set priorities among them. However, CI also cannot be assumed as an absolute factor, since data indicate that cognitive functions improve after kidney transplantation [9]. Thus, as stressed by Shrestha et al., the use of both frailty and CI in kidney allocation deserves an ethical analysis, analogous to what has already done in other medical fields [10]. Such ethical analysis should combine both theoretical (e.g. principle-based) reflection and empirical investigation (e.g. about the stakeholders’ opinion). In their paper, Shrestha and colleagues investigate the patients’ opinions about the ethical principles that should be considered in using frailty and CI for allocating kidneys for transplantation. Four themes emerged in particular ‘in which participants: (1) valued maximizing a scarce resource (utility); (2) prioritized equal access to all patients (equity); (3) appreciated a proportional approach to the use of equity and utility (precautionary utility); and (4) sought to weigh utility- and equity-based concerns regarding social support’ [3]. The tendency of the patients is to balance a utilitarian and an egalitarian approach, and they tend to call for planning strategies in order to improve frailty and cognitive function both before and after the transplantation.
These data are extremely useful in order to plan ethically informed clinical strategies for the assessment of frailty and CI in the allocation of kidneys for transplantation. However, other stakeholders should also be consulted (see Fig. 1). For this reason, a survey about ‘Cognitive decline related to chronic kidney disease as an exclusion factor from kidney transplantation’ is currently in progress as part of the abovementioned COST Action CONNECT. Preliminary results (154 respondents from 41 countries so far) indicate that:
There is currently a lack of consensus on the necessity and the modality of psychological assessment of kidney transplant candidates, with international guidelines not consistent on this point
The majority of respondents think that all patients with CKDs should have a face-to-face psychological assessment performed by a professional in collaboration with the patient's family before being admitted to kidney transplantation
Importantly, the majority of respondents think that cognitive decline can become a contraindication to kidney transplantation.
There are plenty of clinical, ethical and legal issues arising from the connection between frailty, CI and kidney transplantation. These issues regard not only the choice of which patients to eventually include on waitlists, but also if and how frailty and CI impact on some ability traditionally considered as key for ethical and legal requirements like autonomy and self-determination (e.g. through informed consent).
The paper by Greinert et al. is the kind of empirical research needed for informing this debate. It provides useful data and indicates the direction to further explore to advance in the discussion and to eventually improve the healthcare and the quality of life of affected patients.
ACKNOWLEDGEMENTS
COST Action CA19127—Cognitive decline in Nephro-Neurology European Cooperative Target (CONNECT). M.F. was supported by the European Union's Horizon 2020 Framework Programme for Research and Innovation under the Specific Grant Agreement No. (945539) (Human Brain Project SGA3).
Appendix
CONNECT Consortium Collaborators:
Members of the COST Action CA19127-Cognitive Decline in Nephro-Neurology: European Cooperative Target (CONNECT) Consortium:
Alexandre Andrade; Maie Bachmann; Inga Bumblyte; Adrian Constantin Covic; Pilar Delgado; Nicole Endlich; Andreas Engvig; Denis Fouque; Casper Franssen; Sebastian Frische; Liliana Garneata; Loreto Gesualdo; Konstantinos Giannakou; Dimitrios Goumenos; Ayşe Tuğba Kartal; Laila-Yasmin Mani; Hans-Peter Marti; Christopher Mayer; Rikke Nielsen; Vesna Pešić; Merita Rroji (Molla); Giorgos Sakkas; Goce Spasovski; Kate I. Stevens; Evgueniy Vazelov; Davide Viggiano; Lefteris Zacharia; Ana Carina Ferreira; Jolanta Malyszko; Ewout Hoorn; Andreja Figurek; Robert Unwin; Carsten Wagner; Christoph Wanner; Annette Bruchfeld; Marion Pepin; Andrzej Wieçek; Dorothea Nitsch; Ivo Fridolin; Gaye Hafez; Maria José Soler; Michelangela Barbieri; Bojan Batinić; Laura Carrasco; Sol Carriazo; Ron Gansevoort; Gianvito Martino; Francesco Mattace Raso; Ionut Nistor; Alberto Ortiz; Giuseppe Paolisso; Daiva Rastenytė; Gabriel Stefan; Gioacchino Tedeschi; Ziad A. Massy; Boris Bikbov; Karl Hans Endlich; Olivier Godefroy; Jean-Marc Chillon; Anastassia Kossioni; Justina Kurganaite; Norberto Perico; Giuseppe Remuzzi; Tomasz Grodzicki; Francesco Trepiccione; Carmine Zoccali; Mustafa Arici; Peter Blankestijn; Kai-Uwe Eckardt; Danilo Fliser; EugenioGutiérrez Jiménez; Maximilian König; Ivan Rychlik; Michela Deleidi; George Reusz.
Contributor Information
Michele Farisco, Biogem, Biology and Molecular Genetics Institute, Ariano Irpino (AV), Italy; Centre for Research Ethics and Bioethics, Uppsala University, Uppsala, Sweden.
Irene Zecchino, Department of Science and Technology, University of Sannio, Benevento, Italy.
Giovambattista Capasso, Biogem, Biology and Molecular Genetics Institute, Ariano Irpino (AV), Italy; Department Translational Medical Science, University Campania Luigi Vanvitelli, Naples, Italy.
the CONNECT Consortium:
Alexandre Andrade, Maie Bachmann, Inga Bumblyte, Adrian Constantin Covic, Pilar Delgado, Nicole Endlich, Andreas Engvig, Denis Fouque, Casper Franssen, Sebastian Frische, Liliana Garneata, Loreto Gesualdo, Konstantinos Giannakou, Dimitrios Goumenos, Ayşe Tuğba Kartal, Laila-Yasmin Mani, Hans-Peter Marti, Christopher Mayer, Rikke Nielsen, Vesna Pešić, Merita Rroji (Molla), Giorgos Sakkas, Goce Spasovski, Kate I Stevens, Evgueniy Vazelov, Davide Viggiano, Lefteris Zacharia, Ana Carina Ferreira, Jolanta Malyszko, Ewout Hoorn, Andreja Figurek, Robert Unwin, Carsten Wagner, Christoph Wanner, Annette Bruchfeld, Marion Pepin, Andrzej Wieçek, Dorothea Nitsch, Ivo Fridolin, Gaye Hafez, Maria José Soler, Michelangela Barbieri, Bojan Batinić, Laura Carrasco, Sol Carriazo, Ron Gansevoort, Gianvito Martino, Francesco Mattace Raso, Ionut Nistor, Alberto Ortiz, Giuseppe Paolisso, Daiva Rastenytė, Gabriel Stefan, Gioacchino Tedeschi, Ziad A Massy, Boris Bikbov, Karl Hans Endlich, Olivier Godefroy, Jean-Marc Chillon, Anastassia Kossioni, Justina Kurganaite, Norberto Perico, Giuseppe Remuzzi, Tomasz Grodzicki, Francesco Trepiccione, Carmine Zoccali, Mustafa Arici, Peter Blankestijn, Kai-Uwe Eckardt, Danilo Fliser, EugenioGutiérrez Jiménez, Maximilian König, Ivan Rychlik, Michela Deleidi, and George Reusz
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Greinert R, Greinert D, Eger A-Let al. . Subclinical cognitive impairment in chronic kidney disease is associated with frailty and reduced quality of life. Nephrol Dial Transplant 2022;gfac303. doi: 10.1093/ndt/gfac303. Online ahead; of print. [DOI] [PubMed] [Google Scholar]
- 2. Fried LP, Tangen CM, Walston Jet al. . Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Med Sci 2001;56:M146–57. [DOI] [PubMed] [Google Scholar]
- 3. Shrestha P, Van Pilsum Rasmussen SE, Fazal Met al. . Patient perspectives on the use of frailty, cognitive function, and age in kidney transplant evaluation. AJOB Empir Bioeth 2022;13:263–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McAdams-DeMarco MA, Olorundare IO, Ying Het al. . Frailty and postkidney transplant health-related quality of life. Transplantation 2018;102:291–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McAdams-DeMarco MA, Van Pilsum Rasmussen SE, Chu NMet al. . Perceptions and practices regarding frailty in kidney transplantation: results of a national survey. Transplantation 2020;104:349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gupta A, Montgomery RN, Bedros Vet al. . Subclinical cognitive impairment and listing for kidney transplantation. Clin J Am Soc Nephrol 2019;14:567–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harhay MN, Rao MK, Woodside KJet al. . An overview of frailty in kidney transplantation: measurement, management and future considerations. Nephrol Dial Transplant 2020;35:1099–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen X, Liu Y, Thompson Vet al. . Transplant centers that assess frailty as part of clinical practice have better outcomes. BMC Geriatr 2022;22:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chu NM, Gross AL, Shaffer AAet al. . Frailty and changes in cognitive function after kidney transplantation. J Am Soc Nephrol 2019;30:336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wilkinson DJC. Frailty triage is rationing intensive medical treatment on the grounds of frailty ethical? Am J Bioeth 2021;21:48–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


