In Europe there are increasing numbers of old (more than 65 years old) and very old (more than 80 years old) patients (very old intensive care patients – VIPs) (Figure 1). In addition to combinations of chronic conditions (multi-morbidity), there are geriatric disabilities and functional limitations, with a profound impact on management in the ICU and afterwards [1].
FIGURE 1.
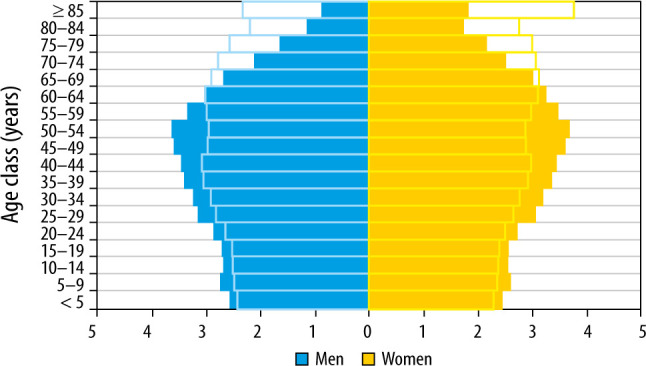
Population pyramids in Europe in 2018 versus 2050
THE ORIGINS OF THE VIP NETWORK
The rapid increase in the number of publications, as shown by the slope of the graph in Figure 2, indicates the increased interest in the area of VIPs.
FIGURE 2.
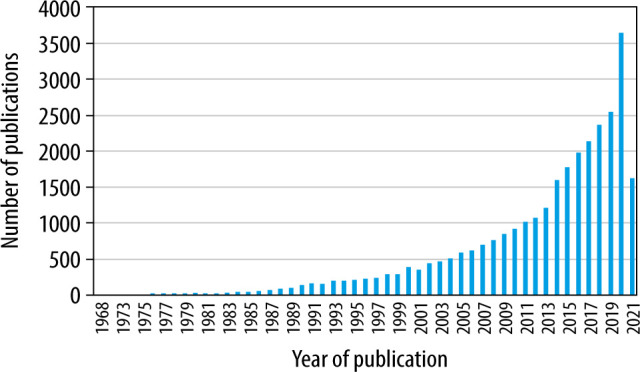
Number of publications in PubMed with the search terms “old” and “intensive care” 1968–2021
A group based on the Health Service Research and Outcome Section (HSRO) of the European Society of Intensive Care Medicine (ESICM) decided to further advance the study of VIPs, and an initiative was launched at the HSRO Section meeting in Milan in October 2016. We describe herein the development and progress of the research network (VIP Network) that has grown out of these initial efforts.
The new VIP Network, with financial support from the ESICM (ESICM Research award for 2017), identified knowledge gaps both in how best to treat VIPs and in outcomes (survival and quality of life).
The VIP Network is led by a steering group which meets in person from time to time (e.g. at international research meetings, as well as at dedicated network meetings in Bergen, Norway, and Jerusalem, Israel [2]) and weekly by videoconference to discuss the research agenda. The steering group emphasizes shared decision-making and inclusiveness. The task of leading research projects has been distributed amongst the group members. Interested researchers from outside the core group are often invited to join projects. The steering group sets the agenda and the direction of study. Then, each country has a national co-ordinator to recruit suitable and interested ICUs. Such a system captures a very wide spectrum of countries and ICUs, but will still be affected by some degree of bias, in that only units with an interest in the topic and with the resources to carry out a project will be involved. This approach has resulted in the inclusion of tens of countries, hundreds of ICUs, and thousands of patients. The entire network is based on interest in the subject, collegiality, and goodwill.
Access to data and authorship of papers are both important for the smooth functioning of the network. Once collated, the de-identified data is available for use by all members of the network. Production of publications is open to all members of the network, with authorship (inclusion in the list of authors and order of inclusion) reflecting contribution to the publication.
THE MAIN VIP NETWORK STUDIES – VIP1, VIP2, AND COVIP
The VIP Network has undertaken 3 major studies (VIP1 [3], VIP2 [4], and COVIP [5]), in a multi-national setting involving approximately 30 European and Middle Eastern countries and in hundreds of intensive care units. These studies have been set up with modest funding (see Table 1) and despite the hurdles of differing ethical review board requirements in different jurisdictions. Clinical studies in Europe have faced the additional challenges of the General Data Privacy Regulation (GDPR) by the European Union since May 2018 [6]. The GDPR regards the protection of personal data as a fundamental right.
TABLE 1.
Funding sources for the VIP group 2017–2021
| Funding source | Funding amount € | |
|---|---|---|
| General use | National use | |
| ESICM Research Award 2017 | 20,000 | |
| EOSC funding. From the European Union’s Horizon | 50,000 | |
| Programme call H2020-INFRAEOSC-05-2018-2019, | ||
| grant Agreement number 831644 | ||
| Fondation Assistance Publique-Hôpitaux de Paris pour la recherche | 111,000 | |
| Health Region West (Norway) 2018–2020 | *450,000 | |
As a part of funding research of elderly ICU patients in Norway, 3-year project
The VIP1 study was undertaken rapidly after establishment of the VIP Network, with the first paper accepted for publication by September 2017 [3]. The focus of the study [3] (over 5000 patients) was the over 80-year-old group of patients presenting to the ICU. The main finding was that frailty, as measured by the Clinical Frailty Scale (CFS), was highly associated with 30-day mortality.
VIP2 (approximately 4000 patients) focused only on emergency admissions of VIPs to the ICU [4]. The occurrence of other “geriatric” syndromes such as co-morbidity, polypharmacy, activity of daily life, and cognition were also included. Frailty was again the best predictor of outcome.
The COVIP study (4000 patients) [5] was conducted during 2 time periods in 2020, coinciding with the initial 2 surges of the Covid-19 pandemic in Europe, and investigated the main predictors of hospital outcome in VIPs with Covid-19. The study also captured 30- and 90-day outcomes, as well as differences between the first and second surges of the pandemic.
The results of the above studies have been published widely (Appendix 1). The conduct of studies has been streamlined over time, with eCRFs and central data management, allowing for rapid data analysis and publication of results, whilst maintaining compliance with GDRP.
FUTURE PROGRESS
Current work is focused on further sub-analyses and publication of the COVIP data. The group is also strengthening alliances with multi-disciplinary groups, in particular geriatricians and rehabilitation experts, recognizing that intensive care is only one segment of the health trajectory of geriatric patients.
The group is exploring 2 further important areas of research. Firstly, the use of artificial intelligence to improve prediction of outcome at the individual level [7, 8]. Secondly, we are planning a study of time-limited trials (TLT) in VIPs. Because the outcome is so difficult to predict, the VIP is admitted to the ICU and given the benefit of full treatment. If he/she responds to treatment, then treatment continues at the same intensity, but if it becomes clear that the patient is deteriorating despite treatment, then de-escalation or palliation are considered. Other areas of interest for future study by the VIP Network are listed in Table 2.
TABLE 2.
Future areas of study by the VIP Network [9]
| 1. What does the consumer think? What is the opinion of the very elderly about admission to the ICU in the event of a severe acute illness or deterioration of organ function (end-stage organ disease)? |
|---|
| 3. The role of geriatricians in the pre-admission assessment of very old patients presenting to the ICU, ongoing care in the ICU (together with intensivists), and follow-up after discharge from the ICU. Will this improve care of the very elderly patient and result in more efficient use of ICU resources? |
| 4. Examining syndromes more common in the very elderly ICU patient, such as delirium, and the best pharmacological and non-pharmacological methods to treat these syndromes, as well as preventative measures to avoid the syndromes. |
| 5. Studying the burden of intensive care on very elderly patients, their families, caregivers, and society. |
| 6. End of life care in the very old – how to better predict outcomes and take care of very old patients at the end of their lives. |
| 7. The incidence and outcomes of sepsis in very old ICU patients. |
| 8. Studies to determine the incidence, outcomes, prevention, and treatment of neuro-cognitive derangements as a result of admission to the ICU. |
| 9. Pharmacokinetic studies of medications commonly used in the ICU in very old people, including antibiotics, sedatives, and analgesics. |
| 10. Study examining the use of time-limited trials – checking the trajectory of individual very old patients in the ICU to see if they are responding to therapy over the course of a few days, and then deciding on subsequent treatment strategy. |
The VIP group is making a concerted effort to engage legal and political entities, such as the Konrad Adenauer Foundation in Germany, with the ethical challenges faced by all intensivists.
CONCLUSIONS
The VIP study network is an example of a group of like-minded intensivists who are self-organized into an international network, recognizing a growing area of intensive care practice with unanswered questions, then tackling those questions by working together collegially and efficiently. Bureaucracy and funding to expand the focus of planned studies remain challenges. A great deal of work remains.
ACKNOWLEDGEMENTS
Financial support and sponsorship
none.
APPENDIX 1. Main publications by the VIP Network, the main outcome, and the number of citations per publication
| Reference | Main outcome | Number of citations |
|---|---|---|
| Frailty is associated with long-term outcome in patients with sepsis who are over 80 years old: results from an observational study in 241 European ICUs Haas LEM, Boumendil A, Flaatten H, et al.; VIP2 study group Age Aeing 2021; Mar 20; afab036 [Online ahead of print] | There is substantial long-term mortality in VIPs admitted with sepsis. Frailty, age, and disease severity were identified as predictors of long-term mortality in VIPs admitted with sepsis. | 0 |
| Reliability of the Clinical Frailty Scale in very elderly ICU patients: a prospective European study Flaatten H, Guidet B, Andersen FH, et al. Ann Intensive Care 2021; 11: 22 | Overall, we documented a high reliability using CFS in this setting. This frailty score could be used more frequently in elderly ICU patients in order to create a more holistic and realistic impression of the patient´s condition prior to ICU admission. | 3 |
| Frailty as a prognostic indicator in intensive care Jung C, Bruno RR, Wernly B, Wolff G, Beil M, Kelm M Dtsch Ärztebl Int 2020; 117: 668-673 | In Germany, frailty in intensive-care patients is currently best assessed on a simple visual scale (CFS). | 3 |
| Sex-specific outcome disparities in very old patients admitted to intensive care medicine: a propensity matched analysis Wernly B, Bruno RR, Kelm M, et al.; VIP2 Study Group. Sci Rep 2020; 10: 18671 | Male sex was associated with adverse 30-day mortality but not ICU mortality. | 0 |
| The wave of very old people in the intensive care unit – a challenge in decision-making van Heerden PV, Sviri S, Beil M, et al. J Crit Care 2020; 60: 290-293 | There is a wave of very old people arriving in the intensive care unit, and we have much to do to prepare for it and for the ethical, fair, and appropriate care of these critically ill, but elderly, patients. | 1 |
| Prognostication in older ICU patients: mission impossible? Flaatten H, Beil M, Guidet B Br J Anaesth 2020; 125: 655-657 | Editorial – In the real word, ICU physicians do not use prognostic scores in isolation for their individual prognostications but add a lot of other information about the patient before a decision is made. | 1 |
| Therapy limitation in octogenarians in German intensive care units is associated with a longer length of stay and increased 30 days mortality: a prospective multicenter study Bruno RR, Wernly B, Beil M, et al. J Crit Care 2020; 60: 58-63 | In German ICUs, any limitation of life-sustaining therapy in VIPs is associated with a significantly increased ICU length of stay and mortality. CFS reliably predicts the outcome. | 0 |
| Elderly patients in the intensive care unit Flaatten H, Beil M, Guidet B Semin Respir Crit Care Med 2020; 42: 10-19 | The major challenge for the coming decades will be the question of whom to treat and the quest for better triage criteria not based on age alone. Challenges with the level of care during the ICU stay will also be discussed. A stronger relationship with geriatricians should be promoted. | 0 |
| Comments to “Frailty is associated with hospital readmission in geriatric patients: a prognostic study” : Assessment of frailty in geriatric patients: let’s keep it simple Bruno RR, Wernly B, Guidet B, Flaatten H, De Lange DW, Jung C Eur Geriatr Med 2020; 11: 885-886 | The CFS was already successfully applied in large clinical trials on older patients by our group. One of the most important findings was that assessing ADL and counting comorbidities did not improve the predictive value of the CFS | 0 |
| Inhibitors of the renin–angiotensin–aldosterone system and COVID-19 in critically ill elderly patients Jung C, Bruno RR, Wernly B, et al. COVIP study group Eur Heart J Cardiovasc Pharmacother 2021; 7: 76-77 | The univariate association of previous ACE-I therapy with lower mortality (OR 0.46, 95% CI: 0.26–0.84; P = 0.01) in patients with COVID-19 remained statistically significant after propensity score adjustment (aOR 0.32, 95% CI: 0.15–0.67; P = 0.002). | 3 |
| Frailty assessment in very old intensive care patients: the Hospital Frailty Risk Score answers another question Bruno RR, Guidet B, Wernly B, Flaatten H, Jung C Intensive Care Med 2020; 46: 1514-1515 | Triage decisions in intensive care medicine must be quick and reliable. Ideally, we assess our patients in multiple dimensions. Frailty research is still in its infancy, but the CFS seems to be a rapid and multidimensional tool. | 2 |
| Sepsis at ICU admission does not decrease 30-day survival in very old patients: a post-hoc analysis of the VIP1 multinational cohort study Ibarz M, Boumendil A, Haas LEM, et al.; VIP1 study Ann Intensive Care 2020; 10: 56 | After adjusting for organ dysfunction, sepsis at admission was not independently associated with decreased 30-day survival in this multinational study of 3869 VIPs. Age, frailty, and SOFA score were independently associated with survival. | 0 |
| The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study Guidet B, de Lange DW, Boumendil A, et al.; VIP2 study group. Intensive Care Med 2020; 46: 57-69 | Frailty assessment using the CFS can predict short-term mortality in elderly patients admitted to the ICU. Other geriatric syndromes do not improve the prediction model. Because CFS is easy to measure, it should be routinely collected for all elderly ICU patients, particularly in connection to advanced care plans, and should be used in decision- making | 46 |
| Validation of the clinical frailty score (CFS) in French language Abraham P, Courvoisier DS, Annweiler C, et al. BMC Geriatr 2019; 19: 322 | The French cultural adaptation of this CFS has adequate psychometric properties for doctors or nurses to evaluate frailty in very old intensive care patients. | 8 |
| Frailty increases mortality among patients ≥ 80 years old treated in Polish ICUs Fronczek J, Polok KJ, Nowak-Kózka I, et al. Anaesthesiol Intens Ther 2018; 50: 245-251 | Measuring frailty in critically ill older adults can facilitate making more informed clinical decisions and help avoid futile interventions. | 8 |
| The hospital frailty risk score is of limited value in intensive care unit patients Bruno RR, Wernly B, Flaatten H, Schölzel F, Kelm M, Jung C Crit Care 2019; 23: 239 | Frailty is complex and its detection crucial, but automatic electronic addition of ICD codes cannot replace the clinical assessment. | 9 |
| Huge variation in obtaining ethical permission for a non- interventional observational study in Europe de Lange DW, Guidet B, Andersen FH, et al. BMC Med Ethics 2019; 20: 39 | Getting ethical approval for low-risk, non-interventional, observational studies varies enormously across European countries. | 5 |
| A comparison of very old patients admitted to intensive care unit after acute versus elective surgery or intervention Jung C, Wernly B, Muessig JM, et al.; VIP1 study group J Crit Care 2019; 52: 141-148 | VIPs admitted to ICU after elective surgery showed favourable outcomes over patients after acute surgery even after correction for relevant confounders. Frailty might be used to guide clinicians in risk stratification in both patients admitted after elective and acute surgery. | 16 |
| Cumulative prognostic score predicting mortality in patients older than 80 years admitted to the ICU de Lange DW, Brinkman S, Flaatten H, et al.; VIP1 study group J Am Geriatr Soc 2019; 67: 1263-1267 | A predictive model of cumulative events predicts 30-day mortality in patients older than 80 years admitted to ICUs. | 9 |
| How does frailty affect ICU outcome? Flaatten H, Jung Ch, Vallet H, Guidet B Curr Anesthesiol Rep 2019; 9: 144-150 | Frailty may be more important than age alone in predicting outcomes for patients admitted to the ICU. | 4 |
| Caring for the critically ill patients over 80: a narrative review Guidet B, Vallet H, Boddaert J, et al. Ann Intensive Care 2018; 8: 114 | According to previous considerations, we provide an algorithm presented as a guide to aid in the decision-making process for the caring of the critically ill older patients. | 26 |
| Frailty: We need valid and reliable tools in critical care Flaatten H, Clegg A Intensive Care Med 2018; 44: 1973-1975 | Given the importance of frailty in the context of critical care, we must be confident that the instruments used to identify the condition are robust and properly validated. | 18 |
| Clinical Frailty Scale (CFS) reliably stratifies octogenarians in German ICUs: a multicentre prospective cohort study Muessig JM, Nia AM, Masyuk M, et al. BMC Geriatr 2018; 18: 162 | The CFS is an easy, determinable, valuable tool for prediction of 30-day ICU survival in octogenarians; thus, it may facilitate decision-making for intensive care givers in Germany. | 20 |
| Predicting outcomes in very old ICU patients: time to focus on the past? Flaatten H, Oeyen S, deLange DW Intensive Care Med 2018; 44: 1344-1345 | Recently pre-ICU factors were found to have prognostic value for quality of life in 1-year survivors after critical illness. If developed properly, such a new score may also guide the process of pre-ICU triage because most of these variables are already known, with less focus on acutely deranged physiology and organ dysfunction, although the latter remains important for short-term survival. It may be time to focus on the past in order to avoid unnecessary suffering in the future. | 6 |
| Clinical Frailty Scale (CFS) reliably stratifies octogenarians in German ICUs: a multicentre prospective cohort study Muessig JM, Nia AM, Masyuk M, et al. BMC Geriatr 2018; 18: 162 | The CFS is an easy, determinable, valuable tool for prediction of 30-day ICU survival in octogenarians; thus, it may facilitate decision-making for intensive care givers in Germany. | 20 |
| Withholding or withdrawing of life-sustaining therapy in older adults (≥ 80 years) admitted to the intensive care unit Guidet B, Flaatten H, Boumendil A, et al.; VIP1 study group Intensive Care Med 2018; 44: 1027-1038 | Given the limited survival chances of very old patients and the cost and scarcity of ICU resources, an active policy for limiting life-sustaining therapy should be advocated for patients who are not responding to treatment or not willing to continue ICU treatment. This should be accompanied by a campaign encouraging patients to express their preferences and wishes before they become ill. | 36 |
| Should this elderly patient be admitted to the ICU? Guidet B, de Lange DW, Flaatten H Intensive Care Med 2018; 44: 1926-1928 | Editorial | 13 |
| The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years) Flaatten H, De Lange DW, Morandi A, et al.; VIP1 study group Intensive Care Med 2017; 43: 1820-1828 | Among very old patients (≥ 80 years) admitted to the ICU, the consecutive classes in Clinical Frailty Scale were inversely associated with short-term survival. | 120 |
| The status of intensive care medicine research and a future agenda for very old patients in the ICU Moreno R, Christensen S, Joynt GM, et al. Intensive Care Med 2017; 43: 1319-1328 | "Very old intensive care patients” (abbreviated to VOPs; greater than 80 years old) are probably the fastest expanding subgroup of all intensive care unit (ICU) patients. Until recently, most ICU physicians have been reluctant to admit these VOPs. The general consensus was that there was little survival to gain, and the incremental life expectancy of ICU admission was considered too small. Several publications have questioned this belief, but others have confirmed the poor long-term mortality rates in VOPs. More appropriate triage (resource limitation enforced decisions), admission decisions based on shared decision-making and improved prediction models are also needed for this particular patient group. | 78 |
| The good, the bad, and the ugly: pandemic priority decisions and triage Flaatten H, van Heerden V, Jung C, et al. J Med Ethics 2020; medethics-2020-106489 [Online ahead of print] | Usual medical triage and priority setting may not be sufficient to decrease inflow and there may not be enough intensive care unit beds available. In this phase different criteria must be applied using a utilitarian approach for triage. We argue that this is an important transition where society, and not physicians, must provide guidance to support triage that is no longer based on medical priorities alone. | 9 |
| Frailty is associated with an increased mortality among patients ≥ 80 years old treated in Polish ICUs Fronczek J, Polok KJ, Nowak-Kózka I, et al. Anaesthesiol Intensive Ther 2018; 50: 245-251 | Frailty is associated with increased mortality among patients ≥ 80 years old treated in Polish ICUs. | 8 |
Conflicts of interest
none.
References
- 1.Damluji AA, Forman DE, van Diepen S, et al. Older adults in the cardiac intensive care unit. Circulation 2020; 141: e6-e32. doi: 10.1161/CIR.0000000000000741. [DOI] [PubMed] [Google Scholar]
- 2.van Heerden PV, Sviri S, Beil M, et al. The wave of very old people in the intensive care unit–a challenge in decision-making. J Crit Care 2020; 60: 290-293. doi: 10.1016/j.jcrc.2020.08.030. [DOI] [PubMed] [Google Scholar]
- 3.Flaatten H, De Lange DW, Morandi A, et al.; VIP1 study group. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med 2017; 43: 1820-1828. doi: 10.1007/s00134-017-4940-8. [DOI] [PubMed] [Google Scholar]
- 4.Guidet B, de Lange DW, Boumendil A, et al.; VIP2 study group . The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med 2020; 46: 57-69. doi: 10.1007/s00134-019-05853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jung C, Flaatten H, Fjølner J, et al.; COVIP study group . The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care 2021; 25: 149. doi: 10.1186/s13054-021-03551-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.https://eur-lex.europa.eu/legalcontent/EN/TXT/PDF/?uri=CELEX:32016R0679
- 7.Flaatten H, Beil M, Guidet B. Prognostication in older ICU patients: mission impossible? Br J Anaesth 2020; 125: 655-657. doi: 10.1016/j.bja.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beil M, Sviri S, Flaatten H, et al. On predictions in critical care: The individual prognostication fallacy in elderly patients. J Crit Care 2021; 61: 34-38. doi: 10.1016/j.jcrc.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flaatten H, de Lange DW, Artigas A, et al. The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med 2017; 43: 1319-1328. doi: 10.1007/s00134-017-4718-z. [DOI] [PubMed] [Google Scholar]


