Abstract
Definitive diagnosis of familial hypercholesterolemia (FH) is paramount for the risk management of patients and their relatives. The present study aimed to investigate the frequency of gene variants contributing to low-density lipoprotein cholesterol (LDL-C) metabolism and their clinical relevance in patients with early-onset coronary artery disease (EOCAD). Among 63 consecutive patients with EOCAD (men <55 years or women <65 years) who underwent percutaneous coronary intervention (PCI) from 2013 to 2019 at Keio University Hospital, 52 consented to participate in this retrospective study. Targeted sequencing of LDLR, PCSK9, APOB, and LDLRAP1 was performed. Of the 52 patients enrolled (42 men; mean age: 50 ± 6 years), one (LDLR, c.1221_1222delCGinsT) harbored a pathogenic mutation, and one (APOB, c.10591A>G) harbored variants of uncertain significance. Both the patients harboring the variants were male, showing no history of diabetes mellitus or chronic kidney disease, no family history of EOCAD, and no physical findings of FH (i.e., tendon xanthomas or Achilles tendon thickening). Patients harboring the LDLR variant had three-vessel disease, were on a statin prescription at baseline, and had stable LDL-C levels; however, the case showed a poor response to the intensification of medication after PCI. Approximately 3.8% of patients with EOCAD harbored variants of gene related to LDL-C metabolism; there were no notable indicators in the patients' background or clinical course to diagnose FH. Given the difficulty in diagnosing FH based on clinical manifestations and family history, genetic testing could enable the identification of hidden risk factors and provide early warnings to their relatives.
1. Introduction
Familial hypercholesterolemia (FH) is a prevalent autosomal dominant disorder that is mainly caused by a variant in the LDLR, PCSK9, or APOB gene, resulting in abnormal low-density lipoprotein cholesterol (LDL-C) metabolism. It is known as an important trigger of early-onset coronary artery disease (EOCAD) [1–5]. Early intervention and control of LDL-C levels in patients with FH can reduce cardiovascular events [6]. Therefore, determination of the genetic background of patients and strict management of the family profile are of vital importance.
Although evaluation of clinical diagnostic criteria is the cornerstone for diagnosing FH in daily clinical practice, patients with genetically diagnosed FH who do not meet the criteria are still at high risk of coronary artery disease (CAD) [7]. A survey revealed that less than half of patients with CAD who had definite or probable clinical FH showed pathogenic variants in FH-related genes [8, 9]. This discrepancy in clinical and genetic diagnoses can be partly explained by the fact that CAD triggers are largely environmental in origin, besides those of genetic origin [10–13]. Considering the necessity of risk stratification for family members, genetic diagnosis of FH in patients with EOCAD would be of utmost importance. In an era in which genetic tests can be performed easily and rapidly, reliance on clinical criteria is insufficient. However, very little is known about the exact prevalence and characteristics of genetically diagnosed FH in the general population with EOCAD.
The present study aimed to conduct a genetic analysis related to LDL-C metabolism and investigate the clinical characteristics of patients with EOCAD treated at a single institution in Tokyo.
2. Materials and Methods
2.1. Study Cohort
A total of 126 patients with EOCAD (men <55 years and women <65 years of age at the time of percutaneous coronary intervention (PCI)) underwent index PCI for CAD (acute coronary syndrome, exertional angina, and asymptomatic myocardial ischemia) from 2013 to 2019 at Keio University Hospital in Tokyo, Japan. Among the patients, 63 continued to visit the hospital at the time of study registration, and 52 out of the 63 provided informed consent for study enrolment. In this study, we used oral epithelial cells for genomic analysis targeting the following four genes related to LDL-C metabolism: LDLR, PCSK9, APOB, and LDLRAP1 (Figure 1).
Figure 1.
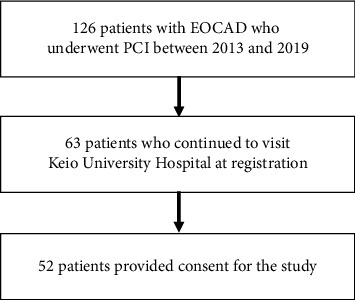
Flow diagram showing patient enrolment. CAD, coronary artery disease; PCI, percutaneous coronary intervention.
This study was conducted in accordance with the tenets of the Declaration of Helsinki, and approval was obtained from the institutional review board/ethics committee. The research was registered in the University Hospital Medical Information Network (registration number: UMIN000039852). All participants provided written informed consent.
2.2. Sequencing and Variant Selection
Sequencing was performed using an Illumina MiSeq sequencer (Illumina Inc., San Diego, CA, USA). Alignment against the reference sequence was performed using BWA-MEM [14], and variant calling was performed using VarScan. Variants with a minor allele frequency (MAF) below 1% were considered within a potential pathogenic range, and a quality score (Q) of 30 or higher was adopted. Synonymous variants were excluded if they were demonstrated to be nonpathogenic or benign. Variants were also predicted in silico using PolyPhen-2 and SIFT scores, as well as the combined annotation-dependent depletion (CADD) scoring model with a cut-off value of 15 as a computational prediction [15, 16]. Finally, we defined a causative variant for FH based on whether it fulfilled any of the following criteria: (a) rare (MAF below 1% in the East Asian population) protein-truncating variants (premature stop, frame-shifting insertions or deletions, or canonical splice-sites) at the LDLR gene; (b) rare damaging missense variants at the LDLR, PCSK9, or APOB gene (i.e., those predicted to be damaging by all three in-silico programs, namely, PolyPhen-2, SIFT score, and CADD scoring model); and (c) ClinVar-registered pathogenic or likely pathogenic variants, related to FH, in the LDLR, PCSK9, or APOB gene. In addition, we evaluated whether the variants were classified as pathogenic, with supporting evidence based on the American College of Medical Genetics (ACMG) criteria [17].
2.3. Clinical Evaluations
Patients with variants were compared with respect to their clinical background, including past medical history and family history of EOCAD (men <55 years and women <65 years of age at the time of CAD diagnosis). Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or prior use of antihypertensive medication. Diabetes mellitus was defined according to the diagnostic criteria described by the Japan Diabetes Society. Physical examination was used to confirm Achilles tendon thickening, tendon xanthoma, or corneal arcus. Data were expressed as median (interquartile range (IQR)) or frequency (percentage), depending on whether the variable was considered continuous or categorical, respectively.
3. Results
3.1. Study Population
The majority (80.8%, n = 42) of patients were men, and the median age was 50 years (IQR, 46–53). Ten patients (19.2%) had a family history of EOCAD. The mean baseline LDL-C level was 125 mg/dL (IQR, 114–158), and 13 patients (25.0%) had already been prescribed statins or ezetimibe for hypercholesterolemia at the time of enrolment.
3.2. Genetic Characteristics
From 52 genomic DNA samples, we sequenced four genes (namely, LDLR, PCSK9, APOB, and LDLRAP1), including exonic and splicing regions. We identified two variants, one of which was predicted to be harmful based on the CADD score. Overall, one patient showed pathogenic variants (PM: LDLR, c.1221_1222delCGinsT), and another showed variants of uncertain significance (VUS: APOB, c.10591A>G) (Table 1). No variants of PCSK9 and LDLRAP1 were detected. In our EOCAD cohort, none of the variants showed duplications or were observed together in a single case.
Table 1.
List of genetic variants.
| Gene | Chromosome | Nucleotide change | Amino acid change | Count | Variant type | In silico | ACMG criteria | Variant class | ||
|---|---|---|---|---|---|---|---|---|---|---|
| PolyPhen-2 | SIFT score | CADD score | ||||||||
| LDLR | 19 | c.1221_1222delCGinsT | p.Glu408ArgFs∗5 | 1 | Nonsense | NA | NA | NA | PVS1 + PM2 | PM |
| APOB | 2 | c.10591A>G | p.Lys3531Glu | 1 | Missense | 0.574 | 0 | 19.36 | PM1 + PM2 + PM6 | VUS |
CADD score, combined annotation-dependent depletion score; ACMG criteria, American college of medical genetics criteria; PM, pathogenic mutation; VUS, variant of uncertain significance.
3.3. Association between Genotype and Phenotype
Table 2 shows the comparison of baseline characteristics between patients harboring the variants and those from the total cohort. The proportion of men in the overall cohort was 80.8% (42 cases), and 10 cases (19.2%) had a family history of EOCAD. Both the patients harboring the variants were male, and neither of them had a family history of EOCAD. Although both patients were smokers, there were no environmental causes, such as diabetes mellitus or chronic kidney disease in either of the patients. Patients harboring the variants did not show FH-specific physical manifestations, such as tendon xanthomas or Achilles tendon thickening. The patient harboring the LDLR variant was treated with a statin at baseline, and his LDL-C level was relatively stable (119 mg/dL). However, he showed three-vessel disease and the intensified medication regimen after PCI was not sufficient to lower the LDL-C level, suggesting refractoriness (Table 2).
Table 2.
Baseline characteristics.
| Variables, n (%) | Total population (n = 52) | Case 1 | Case 2 |
|---|---|---|---|
| Responsible gene | NA | LDLR | APOB |
| CAD type | NA | EAP | UAP |
| Age, years (IQR) | 49 (46–53) | 59 | 39 |
| Male | 42 (80.8) | Male | Male |
| BMI, (kg/m2) (IQR) | 25.1 (23.5–27.7) | 24.5 | 21.9 |
| Family history of early-onset CAD | 10 (19.2) | No | No |
| Medical history | |||
| Smoking | 33 (63.5) | Yes | Yes |
| Hypertension | 25 (48.1) | No | Yes |
| Diabetes mellitus | 14 (26.9) | No | No |
| Stroke | 3 (5.8) | No | No |
| Peripheral artery disease | 2 (3.8) | No | No |
| Three-vessel disease | 15 (28.8) | Yes | No |
| Left main trunk lesion | 3 (5.8) | No | No |
| CAD relapse | 6 (11.5) | No | No |
| Laboratory findings at baseline | |||
| LDL-C, (mg/dL) (IQR) | 124 (112–163) | 119 | 108 |
| HDL-C, (mg/dL) (IQR) | 43 (37–48) | 62 | 37 |
| Triglycerides, (mg/dL) (IQR) | 152 (98–225) | 98 | 151 |
| HbA1c, % (IQR) | 5.9 (5.4–6.4) | 6.0 | 5.9 |
| Creatinine, (mg/dL) (IQR) | 0.80 (0.67–1.01) | 1.0 | 0.85 |
| eGFR, mL/min/1.73 m2 (IQR) | 77 (60–88) | 62 | 81 |
| Laboratory findings after medications | |||
| LDL-C, (mg/dL) (IQR) | 81 (65–96) | 121 | 75 |
| HDL-C, (mg/dL) (IQR) | 46 (40–54) | 77 | 47 |
| Triglycerides, (mg/dL) (IQR) | 146 (111–178) | 49 | 101 |
| Changes in LDL-C levels, (mg/dL) (IQR) | −50 (−73 to −23) | 2 | −33 |
| Baseline prescriptions | |||
| Statins | 12 (23.1) | Rosuvastatin, 5 mg | No |
| Ezetimibe | 1 (1.9) | No | No |
| Present prescriptions | |||
| Statins | 51 (98.1) | Rosuvastatin, 10 mg | Rosuvastatin, 5 mg |
| Ezetimibe | 18 (34.6) | No | Yes |
| EPA | 2 (3.8) | No | No |
| PCSK-9 inhibitor | 1 (1.9) | No | No |
PM, pathogenic mutation; VUS, variant of uncertain significance; EAP, effort angina pectoris; UAP, unstable angina pectoris; BMI, body mass index; CAD, coronary artery disease; eGFR, estimated glomerular filtration rate; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; HbA1c, hemoglobin A1c; EPA, eicosapentaenoic acid; PCSK-9, proprotein convertase subtilisin/kexin type 9; IQR, interquartile range.
4. Discussion
In this retrospective study, approximately 3.8% of patients with EOCAD had gene variants related to LDL-C metabolism. For the patients harboring the variants, only a few environmental factors contributed to the disease. In addition, there was no obvious clinical manifestation or a family history of EOCAD, based on the clinical diagnostic criteria. Thus, we found that genetic testing can not only identify patients with FH and reinforce individual risk management but also stratify the hidden risk of cardiovascular events and alert relatives to a potential need for intervention.
In daily clinical practice, FH is mainly diagnosed based on clinical diagnostic criteria (e.g., Dutch Lipid Clinic Network criteria (DLCNC), Simon Broome criteria, and Japan Atherosclerosis Society criteria). These criteria comprise of a family history of EOCAD, physical findings, and serum LDL-C levels [18–20]. Nanchen et al. have reported that among young patients with acute coronary syndromes in Switzerland, 1.6% had probable or definite FH, according to the clinical diagnostic criteria [21]. Regarding the differences between genetic diagnoses, some reports have shown a high diagnostic accuracy of clinical diagnostic criteria compared to that of genetic diagnosis, whereas others have shown discrepancies between the two [22, 23]. Although there are only a few reports of genetic testing in young CAD patients, the prevalence of FH-associated variants shows a relatively wide range depending on the type of gene targeted, the criteria used to determine the pathogenicity of the variants, and racial differences (2–21%) [4, 5]. It is necessary to develop further evidence, establish methods for identifying the pathogenicity of variants, improve comprehensive genetic analysis (including structural variations), and construct unified diagnostic criteria when making a genetic diagnosis of FH in EOCAD patients. Despite being an inexpensive and efficient tool to diagnose FH, clinical diagnosis alone may cause a certain number of patients with FH to be overlooked [7, 23]. In the present study, the two cases that tested genetically positive were clinically undiagnosed cases, showing relatively low or controlled LDL-C levels and no family history of EOCAD. Such underdiagnoses can lead to the overestimation of cardiovascular prognosis in patients with FH and their family members.
Genetic testing has recently become both inexpensive and rapid, and it is a feasible approach for patients with CAD. Combination of genetic testing with conventional clinical diagnostic criteria can improve the risk stratification of cardiovascular events in patients with hypercholesterolemia, suggesting an additive effect and true clinical importance of aggressive genetic testing [7]. Genetic testing is important not only for the assessment of cardiovascular risks or treatment strategies for patients with FH themselves but also for risk management in family members. The risk of CAD events in patients has been associated with cumulative LDL-C levels (mg/dL × years) [3]. This can be efficiently reduced by early intervention [6, 24, 25]. Therefore, verification of the risk of FH among relatives of patients with EOCAD and, if necessary, diagnosis using genetic testing can be a cost-effective strategy to prevent the disease in the active age group and can improve lifetime cardiovascular prognosis.
Naturally, genetic testing has certain limitations; for example, the number of candidate variants for FH is gradually increasing [26–28]. The current standard for determining pathogenicity is to refer to the ACMG guidelines; variants with established pathogenicity can be considered responsible for FH. However, we often see previously unreported variants, and their clinical relevance is difficult to evaluate. In our study, we found previously unreported variants of LDLR (c.1221_1222delCGinsT) and APOB (c.10591A>G). The pathogenicity of the variant detected in APOB was not definitive, but it was predicted to be damaging based on in-silico analysis and was indicated to have a high level of predicted pathogenicity, according to the ACMG guidelines [17]. The variant in LDLR was a truncated rare variant, which was also considered to be a highly pathogenic variant. Another factor that can confuse the decision-making process is a structural variant of the contributing variant itself. This would make it difficult to accurately diagnose using a conventional panel analysis, exome analysis, or whole genome analysis. Continued accumulation of functional analysis data and construction of a genetic database focusing on FH, including racial differences, would be helpful in overcoming these challenges.
The current study had several limitations. First, it was conducted retrospectively at a single center. Therefore, unmeasured confounding factors, such as mental disorders, FH-specific physical findings, or economic status, may have been present. Second, the number of patients who dropped out of the cohort was large due to the nature of the institution; patients are often referred to other medical facilities once conditions are deemed chronic. Third, no functional analysis was performed to validate the pathogenicity of FH-linked genetic variants in the present study; this is particularly desirable for the evaluation of APOB variants. We did not identify pathogenic variants in individuals with confirmed FH. We were not able to assess all relatives of patients with confirmed or suspected FH, despite our vigorous cascade screening. A lack of data might have led to a biased assessment. Fourth, the LDL-C level before statin administration was not available in the case with the LDLR variant. However, clinically implicating FH remained difficult, considering that the LDL-C level was relatively stable after treatment with 5 mg of rosuvastatin at the time of initial presentation. Fifth, the genetic analysis performed in the present study did not include the possible detection of large deletions or duplications in the LDLR gene, which may contribute to FH to some degree. Finally, the study was performed exclusively with Japanese patients; the results might not be applicable to other ethnicities.
5. Conclusions
Approximately 3.8% of patients with EOCAD had FH-related gene variants that were not diagnosed using clinical diagnostic criteria. Genetic testing can accurately identify patients with FH who present few clinical findings other than CAD and can reinforce risk management; moreover, it can stratify the cardiovascular risk of relatives and suggest intervention to prevent adverse outcomes.
Acknowledgments
The authors would like to thank Editage (https://www.editage.com) for their assistance with English language editing. This research was supported by an unrestricted research grant from Recordati S.p.A. The funders provided financial support to F.K. but played no additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
The data supporting the current study are available from the corresponding author upon request.
Conflicts of Interest
F.K. has a financial relationship with a research grant from Recordati S.p.A.
References
- 1.Trinder M., Li X., DeCastro M. L., et al. Risk of premature atherosclerotic disease in patients with monogenic versus polygenic familial hypercholesterolemia. Journal of the American College of Cardiology . 2019;74(4):512–522. doi: 10.1016/j.jacc.2019.05.043. [DOI] [PubMed] [Google Scholar]
- 2.Trinder M., Francis G. A., Brunham L. R. Association of monogenic vs polygenic hypercholesterolemia with risk of atherosclerotic cardiovascular disease. JAMA Cardiology . 2020;5(4):390–399. doi: 10.1001/jamacardio.2019.5954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khera A. V., Won H. H., Peloso G. M., et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. Journal of the American College of Cardiology . 2016;67(22):2578–2589. doi: 10.1016/j.jacc.2016.03.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Do R., Stitziel N. O., Won H. H., et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature . 2015;518(7537):102–106. doi: 10.1038/nature13917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bogsrud M. P., Øyri L. K. L., Halvorsen S., Atar D., Leren T. P., Holven K. B. Prevalence of genetically verified familial hypercholesterolemia among young (< 45 years) Norwegian patients hospitalized with acute myocardial infarction. Journal of Clinical Lipidology . 2020;14(3):339–345. doi: 10.1016/j.jacl.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y., Pletcher M. J., Vittinghoff E., et al. Association between cumulative low-density lipoprotein cholesterol exposure during young adulthood and middle age and risk of cardiovascular events. JAMA Cardiology . 2021;6(12):1406–1413. doi: 10.1001/jamacardio.2021.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tada H., Kawashiri M. A., Nohara A., Inazu A., Mabuchi H., Yamagishi M. Impact of clinical signs and genetic diagnosis of familial hypercholesterolaemia on the prevalence of coronary artery disease in patients with severe hypercholesterolaemia. European Heart Journal . 2017;38(20):1573–1579. doi: 10.1093/eurheartj/ehx004. [DOI] [PubMed] [Google Scholar]
- 8.Shin D. G., Han S. M., Kim D. I., et al. Clinical features of familial hypercholesterolemia in Korea: predictors of pathogenic mutations and coronary artery disease—a study supported by the Korean Society of Lipidology and Atherosclerosis. Atherosclerosis . 2015;243(1):53–58. doi: 10.1016/j.atherosclerosis.2015.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Li J. J., Li S., Zhu C. G., et al. Familial hypercholesterolemia phenotype in Chinese patients undergoing coronary angiography. Arteriosclerosis, Thrombosis, and Vascular Biology . 2017;37(3):570–579. doi: 10.1161/atvbaha.116.308456. [DOI] [PubMed] [Google Scholar]
- 10.Jackson R., Lawes C. M., Bennett D. A., Milne R. J., Rodgers A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. The Lancet . 2005;365(9457):434–441. doi: 10.1016/s0140-6736(05)70240-3. [DOI] [PubMed] [Google Scholar]
- 11.Lewington S., Clarke R., Qizilbash N. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet . 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 12.Almdal T., Scharling H., Jensen J. S., Vestergaard H. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Archives of Internal Medicine . 2004;164(13):1422–1426. doi: 10.1001/archinte.164.13.1422. [DOI] [PubMed] [Google Scholar]
- 13.Prescott E., Hippe M., Schnohr P., Hein H. O., Vestbo J. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ . 1998;316(7137):1043–1047. doi: 10.1136/bmj.316.7137.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Genomics . 2013;1303 [Google Scholar]
- 15.Itan Y., Shang L., Boisson B., et al. The mutation significance cutoff: gene-level thresholds for variant predictions. Nature Methods . 2016;13(2):109–110. doi: 10.1038/nmeth.3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kircher M., Witten D. M., Jain P., O’Roak B. J., Cooper G. M., Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nature Genetics . 2014;46(3):310–315. doi: 10.1038/ng.2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richards S., Aziz N., Bale S., et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of medical genetics and genomics and the association for molecular pathology. Genetics in Medicine . 2015;17(5):405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benn M., Watts G. F., Tybjærg-Hansen A., Nordestgaard B. G. Mutations causative of familial hypercholesterolaemia: screening of 98 098 individuals from the Copenhagen General Population Study estimated a prevalence of 1 in 217. European Heart Journal . 2016;37(17):1384–1394. doi: 10.1093/eurheartj/ehw028. [DOI] [PubMed] [Google Scholar]
- 19.Harada-Shiba M., Arai H., Ishigaki Y., et al. Guidelines for diagnosis and treatment of familial hypercholesterolemia 2017. Journal of Atherosclerosis and Thrombosis . 2018;25(8):751–770. doi: 10.5551/jat.cr003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tada H., Okada H., Nomura A., et al. Clinical diagnostic criteria of familial hypercholesterolemia—a comparison of the Japan Atherosclerosis Society and Dutch Lipid Clinic Network criteria. Circulation Journal . 2021;85(6):891–897. doi: 10.1253/circj.cj-20-0901. [DOI] [PubMed] [Google Scholar]
- 21.Nanchen D., Gencer B., Auer R., et al. Prevalence and management of familial hypercholesterolaemia in patients with acute coronary syndromes. European Heart Journal . 2015;36(36):2438–2445. doi: 10.1093/eurheartj/ehv289. [DOI] [PubMed] [Google Scholar]
- 22.Graham C. A., McIlhatton B. P., Kirk C. W., et al. Genetic screening protocol for familial hypercholesterolemia which includes splicing defects gives an improved mutation detection rate. Atherosclerosis . 2005;182(2):331–340. doi: 10.1016/j.atherosclerosis.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 23.Humphries S. E., Whittall R. A., Hubbart C. S., et al. Genetic causes of familial hypercholesterolaemia in patients in the UK: relation to plasma lipid levels and coronary heart disease risk. Journal of Medical Genetics . 2006;43(12):943–949. doi: 10.1136/jmg.2006.038356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tada H., Okada H., Nohara A., Yamagishi M., Takamura M. Effect of cumulative exposure to low-density lipoprotein-cholesterol on cardiovascular events in patients with familial hypercholesterolemia. Circulation Journal . 2021;85(11):2073–2078. doi: 10.1253/circj.cj-21-0193. [DOI] [PubMed] [Google Scholar]
- 25.Luirink I. K., Wiegman A., Kusters D. M., et al. 20-year follow-up of statins in children with familial hypercholesterolemia. New England Journal of Medicine . 2019;381(16):1547–1556. doi: 10.1056/nejmoa1816454. [DOI] [PubMed] [Google Scholar]
- 26.Usifo E., Leigh S. E., Whittall R. A., et al. Low-density lipoprotein receptor gene familial hypercholesterolemia variant database: update and pathological assessment. Annals of Human Genetics . 2012;76(5):387–401. doi: 10.1111/j.1469-1809.2012.00724.x. [DOI] [PubMed] [Google Scholar]
- 27.Raal F. J., Santos R. D. Homozygous familial hypercholesterolemia: current perspectives on diagnosis and treatment. Atherosclerosis . 2012;223(2):262–268. doi: 10.1016/j.atherosclerosis.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 28.Nordestgaard B. G., Chapman M. J., Humphries S. E., et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. European Heart Journal . 2013;34(45):3478–3490. doi: 10.1093/eurheartj/eht273. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the current study are available from the corresponding author upon request.


