Abstract
Objective
To investigate all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality in Qatar during the COVID-19 pandemic.
Methods
A national, retrospective cohort analysis and national, matched, retrospective cohort studies were conducted between 5 February 2020 and 19 September 2022.
Results
There were 5025 deaths during a follow-up time of 5 247 220 person-years, of which 675 were COVID-19 related. Incidence rates were 0.96 (95% CI 0.93 to 0.98) per 1000 person-years for all-cause mortality, 0.13 (95% CI 0.12 to 0.14) per 1000 person-years for COVID-19 mortality and 0.83 (95% CI 0.80 to 0.85) per 1000 person-years for all-cause non-COVID-19 mortality. Adjusted HR, comparing all-cause non-COVID-19 mortality relative to Qataris, was lowest for Indians at 0.38 (95% CI 0.32 to 0.44), highest for Filipinos at 0.56 (95% CI 0.45 to 0.69) and was 0.51 (95% CI 0.45 to 0.58) for craft and manual workers (CMWs). Adjusted HR, comparing COVID-19 mortality relative to Qataris, was lowest for Indians at 1.54 (95% CI 0.97 to 2.44), highest for Nepalese at 5.34 (95% CI 1.56 to 18.34) and was 1.86 (95% CI 1.32 to 2.60) for CMWs. Incidence rate of all-cause mortality for each nationality group was lower than the crude death rate in the country of origin.
Conclusions
Risk of non-COVID-19 death was low and was lowest among CMWs, perhaps reflecting the healthy worker effect. Risk of COVID-19 death was also low, but was highest among CMWs, largely reflecting higher exposure during first epidemic wave, before advent of effective COVID-19 treatments and vaccines.
Keywords: SARS, Cohort study, Epidemiology
WHAT IS ALREADY KNOWN ON THIS TOPIC.
SARS-CoV-2 infection causes COVID-19 mortality.
COVID-19 deaths may occur due to factors related to the virus, the host or availability of vaccinations and treatments.
There appear to be large variations in COVID-19 mortality and all-cause mortality rates across countries during the COVID-19 pandemic for reasons that remain inadequately understood.
Qatar, with a multinational population of 2.8 million people, has a unique sociodemographic structure.
About 60% of the population consists of craft and manual workers.
Mortality rates among these low-socioeconomic status workers have been subject to debate in the absence of epidemiological assessment.
WHAT THIS STUDY ADDS
Risk of COVID-19 death was very low in the population of Qatar during the COVID-19 pandemic at 0.13 deaths for every 1000 individuals per year.
Risk of COVID-19 death was highest among craft and manual workers and lowest among Qataris who have a high socioeconomic status, but this difference largely reflected differential exposure to the first epidemic wave.
Risk of all-cause death was low in the population of Qatar during the COVID-19 pandemic at 0.96 deaths for every 1000 individuals per year.
Risk of non-COVID-19 death was highest among Qataris and lowest among craft and manual workers, apparently reflecting the healthy worker effect.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Craft and manual workers in Qatar are healthy by recruitment and maintain high levels of physical activity perhaps explaining their lowest rate of all-cause mortality.
Qataris are a typical national population that includes both healthy and unhealthy individuals, perhaps explaining their highest rate of all-cause mortality.
COVID-19 mortality rates show large variations within countries and across countries, with some countries like Qatar experiencing unusually low COVID-19 mortality rates.
Introduction
Qatar, with a multinational population of 2.8 million people, has a unique sociodemographic structure, where single-unit and family households including children, adults and/or older adults account for only 40% of the total population.1 2 This demographic segment of the population is commonly labelled in Qatar as the ‘urban population’ though socioeconomically it consists predominantly of white-collar workers and their families.3 Adults in the urban population typically work in the professional or service workforce, either private or governmental.1–3 The main defining feature of this part of the population is that its members are not migrant blue-collar craft and manual workers (CMWs). Migrant blue-collar CMWs comprise the remaining 60% of the population4 5 and are typically single men, 20–49 years of age, working in development projects2 and living in large shared accommodations.6 Both the urban and CMW populations live in urban areas, mostly in Doha, the capital city, with a negligible part of the population living outside urban areas.7
Nearly 89% of Qatar’s population are expatriates from over 150 countries.1 2 8 9 By nationality, Indians (28%), Bangladeshis (13%) and Nepalese (13%) are the most populous groups followed by Qataris (11%) and Filipinos (7%).1 2 8 9 Nearly all Bangladeshis and Nepalese are part of the CMW population. Meanwhile, Indians and Filipinos are distributed among the CMW and urban populations, but with most Indians being part of the CMW population and most Filipinos being part of the urban population.1 2 8 9 Most remaining nationalities, along with Qataris, are part of the urban population.1 2 8 9 Females account for only a quarter of Qatar’s population, the majority of whom are part of the urban population.7
The first documented community transmission case of SARS-CoV-2 in Qatar was identified on 6 March 2020 and was linked to a cluster of about 300 infections among CMWs living in a high-density housing accommodation.9 10 Since then, Qatar experienced six SARS-CoV-2 epidemic waves dominated sequentially by the original virus (2020),11 Alpha (2021),12 Beta (2021),13 Omicron BA.1 and BA.2 (end of 2021 and 2022),14 Omicron BA.4 and BA.5 (2022)15 and Omicron BA.2.75.2 (2022),16 in addition to a prolonged low-incidence phase dominated by Delta (mid to end of 2021) (online supplemental figure S1).17 18 CMWs were the most affected population by the first epidemic wave, a consequence of living in large shared accommodations.3–5 9 19 20 By the end of the first wave, most CMWs had detectable antibodies against SARS-CoV-2.3–5 9 19 Subsequent waves affected all population sectors in the country.11–16
bmjgh-2023-012291supp001.pdf (682.8KB, pdf)
We investigated all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality in Qatar’s population since the onset of the COVID-19 pandemic. We further investigated differences in mortality risk by major nationality groups and socioeconomic sectors (CMW vs urban populations), after adjustment for confounding factors (sex, age and existing comorbid conditions).
Methods
Study population and data sources
This study was conducted in the population of Qatar and analysed the national mortality database managed by Hamad Medical Corporation, the principal public healthcare provider in Qatar. This database includes all death records in Qatar, including deaths occurring at healthcare facilities and elsewhere. The database also includes forensic deaths investigated by Qatar’s Ministry of Interior.
The study also analysed the national, federated databases for COVID-19 laboratory testing, vaccination, hospitalisation and death, retrieved from the integrated, nationwide, digital health information platform (online supplemental section S1). Databases include all SARS-CoV-2-related data and associated demographic information, with no missing information, since the pandemic onset, such as all PCR tests, and starting from 5 January 2022 onwards, medically supervised rapid antigen tests. Detailed descriptions of Qatar’s SARS-CoV-2 databases have been reported previously.9 13 15 17 21–23
Study design and cohorts
A national, retrospective cohort study was conducted to investigate the incidence of death in Qatar’s population. Selection of the national cohort was based on presence of any record for a SARS-CoV-2 PCR or rapid antigen test, regardless of the test result, since the pandemic onset. Any individual with a record for a SARS-CoV-2 test between 5 February 2020 (earliest record for a SARS-CoV-2 test) and 19 September 2022 (end of study date) was eligible for inclusion in the study. Children <1 year old were excluded.
Testing for SARS-CoV-2 in Qatar is done at a mass scale, and mostly for routine reasons, whereby ~5% of the population is tested every week (online supplemental section S1).17 22 With various testing mandates implemented throughout the COVID-19 pandemic and the large number of tests (14 487 641 tests from pandemic onset until 19 September 2022), it is not conceivable that any citizen or resident in Qatar had not had at least one SARS-CoV-2 test since the start of the pandemic. Accordingly, the SARS-CoV-2 testing database provided a sampling frame for the population of Qatar based on which this study was implemented.
Mortality in the national cohort of Qatar
Incidence rates of all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality were assessed in the full national cohort. Individuals were followed from the calendar day of their first SARS-CoV-2 test until death or end of study censoring (19 September 2022). Outcomes were also assessed for major nationality groups (Bangladeshis, Filipinos, Indians, Nepalese and Qataris).
Incidence rate of death for all-cause mortality by nationality was compared with the crude death rate in countries of origin, as estimated by the United Nations (UN) World Population Prospects for 2021,24 and also after adjustment for the age structure of each nationality group in the national cohort in Qatar.
Differences in mortality by nationality
A series of national, matched, retrospective cohort studies was conducted comparing incidence of death among each major nationality group in Qatar with incidence of death among Qataris. For each of these studies, individuals in the investigated nationality group cohort were exact matched one-to-one by sex, 10-year age group, existing comorbid conditions (none, one, two, three, four, five and six or more comorbidities; online supplemental section S1), SARS-CoV-2 testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test to Qatari individuals.
Matching was performed to balance observed confounders between the two exposure groups for factors that affect mortality risk, namely sex, age and comorbid conditions. That is, matching was only used to create similar cohorts and was not a criterion for conduct of further analysis. Matching by SARS-CoV-2 testing method was done because persons reporting symptoms are more likely to receive PCR than rapid antigen testing. Rapid antigen testing is mostly implemented in routine SARS-CoV-2 testing. Matching by calendar week of the SARS-CoV-2 test was done to ensure that paired individuals were in Qatar at the same time and to control for time-variable differences in mortality risk.
Matching was performed iteratively such that the identified match was alive at the start of follow-up. Matching was iterated with as many replications as needed until exhaustion of the sample, that is, until no more matched pairs with controls that fulfil the eligibility criteria could be identified. Each matched pair was followed from the calendar day of the SARS-CoV-2 test for the Qatari individual until death or end of study censoring (19 September 2022).
Differences in mortality by socioeconomic population sector
Two other national, matched, retrospective cohort studies were conducted comparing incidence of death among the CMW and urban populations with incidence of death among Qataris. These two studies used the same methods for matching and follow-up described above for differences in mortality by nationality.
Nationality is strongly associated with occupation in Qatar and provides a proxy for being a CMW and for socioeconomic status.3–5 9 19 Accordingly, CMW was proxied by Bangladeshi, Indian, Nepalese, Pakistani and Sri Lankan nationalities,3–5 9 19 while the urban population included all other expatriate nationalities residing in Qatar.
Classification of COVID-19 death
Classification of COVID-19 death followed WHO guidelines.25 Assessments were made by trained medical personnel independent of study investigators and using individual chart reviews, as part of a national protocol applied to every deceased patient with COVID-19 since the pandemic onset.
COVID-19 death was defined per WHO classification as ‘a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 disease (eg, trauma). There should be no period of complete recovery from COVID-19 between illness and death. A death due to COVID-19 may not be attributed to another disease (eg, cancer) and should be counted independently of preexisting conditions that are suspected of triggering a severe course of COVID-19’. Detailed WHO criteria for classifying COVID-19 deaths can be found in the WHO technical report.25
Patient and public involvement
Patients or the public were not directly involved in the design, conduct, reporting or dissemination plans of our research.
Statistical analysis
Cohorts were characterised using descriptive statistics and compared using standardised mean differences (SMDs). An SMD of ≤0.1 indicated adequate matching.26 Cumulative incidence of death (defined as proportion of individuals at risk, whose primary endpoint during follow-up was death) was estimated using the Kaplan-Meier estimator method.27 Incidence rate of death in each cohort, defined as number of deaths divided by number of person-years contributed by all individuals in the cohort, was estimated with corresponding 95% CI using a Poisson log-likelihood regression model with Stata V.17.0 stptime command.
HRs, comparing incidence of death in the cohorts and corresponding 95% CIs, were calculated using Cox regression adjusted for matching factors with Stata V.17.0 stcox command. Schoenfeld residuals and log-log plots for survival curves were used to test the proportional hazards assumption. Interactions were not considered. Adjusted HRs were estimated by 3-month intervals since start of follow-up by restricting ‘failures’ to sequential 3-month intervals. Statistical analyses were conducted using Stata/SE V.17.0 (Stata, College Station, Texas, USA).
Oversight
The study was reported following the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (online supplemental table S1).
Results
Mortality in the national cohort of Qatar
There were 5025 deaths recorded in the national cohort of all SARS-CoV-2-tested individuals over a follow-up time of 5 247 220 person-years, of which 675 were COVID-19 related. COVID-19 resulted in 682 deaths in Qatar from pandemic onset up to the end of the study, but six cases were diagnosed with SARS-CoV-2 after death, and thus were not part of the followed cohort. One additional COVID-19 death of a child <1 year old was excluded for age ineligibility.
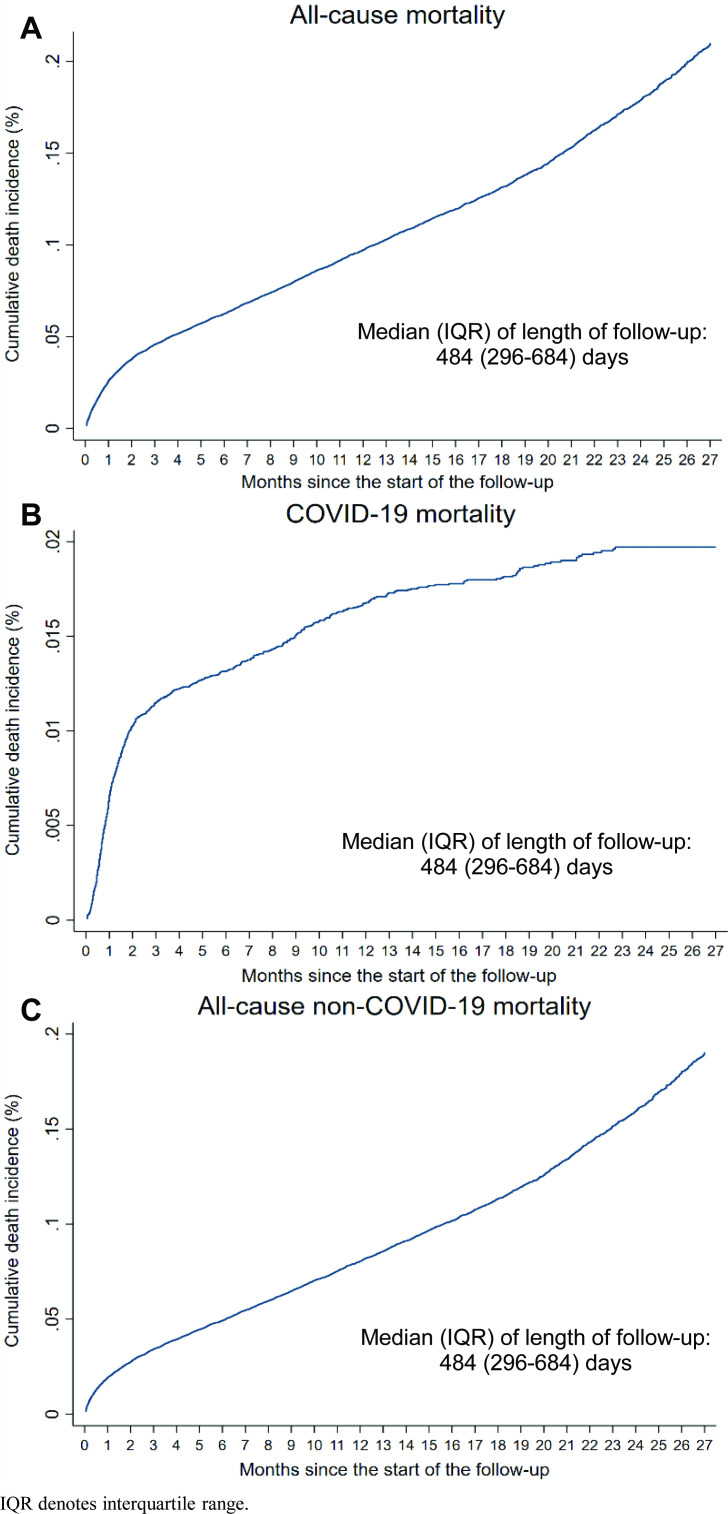
The median follow-up time in the national cohort was 484 days (IQR 296–684 days). Cumulative incidence of death was 0.21% (95% CI 0.20% to 0.22%) for all-cause mortality, 0.02% (95% CI 0.02% to 0.02%) for COVID-19 mortality and 0.19% (95% CI 0.18% to 0.20%) for all-cause non-COVID-19 mortality, after 27 months of follow-up (figure 1). The most rapid increase in COVID-19 mortality occurred just after the start of follow-up, during the first epidemic wave (figure 1 and online supplemental figure S1).
Figure 1.
Cumulative incidence of death for (A) all-cause mortality, (B) COVID-19 mortality and (C) all-cause non-COVID-19 mortality in the population of Qatar.
Incidence rate of death in this national cohort was 0.96 (95% CI 0.93 to 0.98) per 1000 person-years for all-cause mortality, 0.13 (95% CI 0.12 to 0.14) per 1000 person-years for COVID-19 mortality and 0.83 (95% CI 0.80 to 0.85) per 1000 person-years for all-cause non-COVID-19 mortality (table 1).
Table 1.
Incidence rates of death for all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality by nationality compared with both the unadjusted and age-adjusted crude death rates in the country of origin, as estimated by the United Nations World Population Prospects for the year 202124
| Nationality | Incidence rate of death per 1000 person-years (95% CI) | Crude death rate per 1000 persons in 2021 | |||
| All-cause mortality | COVID-19 mortality | All-cause non-COVID-19 mortality | United Nations World Population Prospects estimate | Age-adjusted* United Nations World Population Prospects estimate | |
| Bangladeshis | 0.78 (0.69 to 0.87) | 0.17 (0.14 to 0.22) | 0.60 (0.53 to 0.69) | 5.68 | 2.15 |
| Filipinos | 0.61 (0.53 to 0.69) | 0.14 (0.11 to 0.18) | 0.47 (0.40 to 0.54) | 7.31 | 4.70 |
| Indians | 0.49 (0.45 to 0.52) | 0.09 (0.07 to 0.11) | 0.40 (0.36 to 0.43) | 9.45 | 2.47 |
| Nepalese | 0.42 (0.37 to 0.48) | 0.05 (0.03 to 0.07) | 0.37 (0.32 to 0.43) | 7.77 | 3.11 |
| Qataris | 3.08 (2.94 to 3.24) | 0.24 (0.20 to 0.28) | 2.85 (2.71 to 2.99) | –† | –† |
| Total population | 0.96 (0.93 to 0.98) | 0.13 (0.12 to 0.14) | 0.83 (0.80 to 0.85) | – | – |
*Crude death rate in the country of origin as estimated by the United Nations World Population Prospects for the year 2021,24 but adjusted for the age structure of each nationality group in the national cohort of those ever tested for SARS-CoV-2 in Qatar.
†The United Nations World Population Prospects24 provides an estimate for only the total population of Qatar and does not provide an estimate for only Qataris. The estimate for the overall population is not representative of that of Qataris as Qataris comprise only 11% of the population of Qatar.1 2 8 9
By nationality, incidence rate of death for all-cause mortality was lowest among Nepalese at 0.42 (95% CI 0.37 to 0.48) per 1000 person-years and highest among Qataris at 3.08 (95% CI 2.94 to 3.24) per 1000 person-years (table 1). Incidence rate of death for COVID-19 mortality was lowest among Nepalese at 0.05 (95% CI 0.03 to 0.07) per 1000 person-years and highest among Qataris at 0.24 (95% CI 0.20 to 0.28) per 1000 person-years. Incidence rate of death for all-cause non-COVID-19 mortality was lowest among Nepalese at 0.37 (95% CI 0.32 to 0.43) per 1000 person-years and highest among Qataris at 2.85 (95% CI 2.71 to 2.99) per 1000 person-years.
Incidence rate of death for all-cause mortality for each expatriate nationality group was substantially lower than both the unadjusted and age-adjusted crude death rates in countries of origin (table 1).
Differences in mortality by nationality
Online supplemental tables S2 and S3 describe baseline characteristics of matched cohorts in national, matched, retrospective cohort studies comparing incidence of death among major expatriate nationality groups with incidence of death among Qataris.
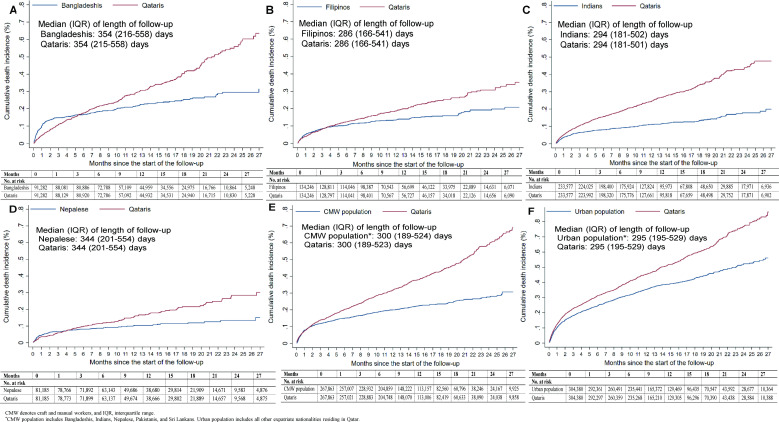
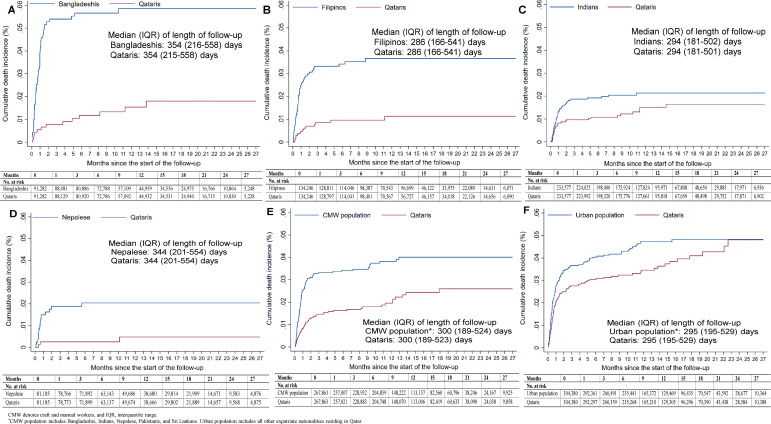
Cumulative incidence of death for all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality is shown in figures 2 and 3 and online supplemental figure S2, respectively. Corresponding incidence rates are shown in tables 2–4, respectively. Differences by nationality were observed. All-cause non-COVID-19 mortality was higher among Qataris than among the major expatriate nationality groups. However, COVID-19 mortality was higher among the major expatriate nationality groups than among Qataris.
Figure 2.
Cumulative incidence of death for all-cause mortality in major nationality groups in Qatar (panels A-F show, respectively, Bangladeshis, Filipinos, Indians, Nepalese, CMW population, and urban poulation) compared with Qataris.
Figure 3.
Cumulative incidence of death for COVID-19 mortality in major nationality groups in Qatar (panels A-F show, respectively, Bangladeshis, Filipinos, Indians, Nepalese, CMW population, and urban poulation) compared with Qataris.
Table 2.
HRs comparing risk of death for all-cause mortality in major nationality groups in Qatar relative to Qataris
| Pairwise comparison* | Cohort size | Deaths | Total follow-up time in person-years | Incidence rate of death per 1000 person-years (95% CI) |
Unadjusted HR (95% CI) |
Adjusted HR (95% CI)† |
| Bangladeshis versus Qataris | ||||||
| Bangladeshis | 91 282 | 196 | 97 020 | 2.02 (1.76 to 2.32) | 0.69 (0.58 to 0.83) |
0.69 (0.58 to 0.83) |
| Qataris | 91 282 | 284 | 96 980 | 2.93 (2.61 to 3.29) | ||
| Filipinos versus Qataris | ||||||
| Filipinos | 134 246 | 177 | 130 981 | 1.35 (1.17 to 1.57) | 0.71 (0.59 to 0.87) |
0.71 (0.59 to 0.87) |
| Qataris | 134 246 | 248 | 130 930 | 1.89 (1.67 to 2.15) | ||
| Indians versus Qataris | ||||||
| Indians | 233 577 | 245 | 218 735 | 1.12 (0.99 to 1.27) | 0.44 (0.38 to 0.51) |
0.44 (0.38 to 0.51) |
| Qataris | 233 577 | 553 | 218 451 | 2.53 (2.33 to 2.75) | ||
| Nepalese versus Qataris | ||||||
| Nepalese | 81 185 | 81 | 85 130 | 0.95 (0.77 to 1.18) | 0.62 (0.47 to 0.82) |
0.62 (0.47 to 0.82) |
| Qataris | 81 185 | 131 | 85 110 | 1.54 (1.30 to 1.83) | ||
| CMW population‡ versus Qataris | ||||||
| CMW population | 267 863 | 508 | 257 908 | 1.97 (1.81 to 2.15) | 0.60 (0.54 to 0.67) |
0.59 (0.53 to 0.66) |
| Qataris | 267 863 | 850 | 257 629 | 3.30 (3.08 to 3.53) | ||
| Urban population‡ versus Qataris | ||||||
| Urban population | 304 380 | 1006 | 294 500 | 3.42 (3.21 to 3.63) | 0.74 (0.69 to 0.81) |
0.74 (0.68 to 0.80) |
| Qataris | 304 380 | 1352 | 294 206 | 4.60 (4.36 to 4.85) | ||
*Cohorts were exact matched one-to-one by sex, 10-year age groups, comorbidity count, testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
†Cox regression analysis adjusted for sex, 10-year age groups, comorbidity count, SARS-CoV-2 testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
‡CMW population includes Bangladeshis, Indians, Nepalese, Pakistanis and Sri Lankans. Urban population includes all other expatriate nationalities residing in Qatar.
CMW, craft and manual worker.
Table 3.
HRs comparing risk of death for COVID-19 mortality in major nationality groups in Qatar relative to Qataris
| Pairwise comparison* | Cohort size | Deaths | Total follow-up time in person-years | Incidence rate of death per 1000 person-years (95% CI) |
Unadjusted HR (95% CI) |
Adjusted HR (95% CI)† |
| Bangladeshis versus Qataris | ||||||
| Bangladeshis | 91 282 | 51 | 97 020 | 0.53 (0.40 to 0.69) | 3.92 (2.13 to 7.22) |
4.00 (2.18 to 7.36) |
| Qataris | 91 282 | 13 | 96 980 | 0.13 (0.08 to 0.23) | ||
| Filipinos versus Qataris | ||||||
| Filipinos | 134 246 | 46 | 130 981 | 0.35 (0.26 to 0.47) | 3.54 (1.91 to 6.55) |
3.57 (1.93 to 6.61) |
| Qataris | 134 246 | 13 | 130 930 | 0.10 (0.06 to 0.17) | ||
| Indians versus Qataris | ||||||
| Indians | 233 577 | 46 | 218 735 | 0.21 (0.16 to 0.28) | 1.53 (0.97 to 2.43) |
1.54 (0.97 to 2.44) |
| Qataris | 233 577 | 30 | 218 451 | 0.14 (0.10 to 0.20) | ||
| Nepalese versus Qataris | ||||||
| Nepalese | 81 185 | 16 | 85 130 | 0.19 (0.12 to 0.31) | 5.33 (1.55 to 18.30) |
5.34 (1.56 to 18.34) |
| Qataris | 81 185 | 3 | 85 110 | 0.04 (0.01 to 0.11) | ||
| CMW population‡ versus Qataris | ||||||
| CMW population | 267 863 | 96 | 257 908 | 0.37 (0.30 to 0.45) | 1.85 (1.32 to 2.59) |
1.86 (1.32 to 2.60) |
| Qataris | 267 863 | 52 | 257 629 | 0.20 (0.15 to 0.26) | ||
| Urban population‡ versus Qataris | ||||||
| Urban population | 304 380 | 129 | 294 500 | 0.44 (0.37 to 0.52) | 1.24 (0.96 to 1.61) |
1.24 (0.96 to 1.61) |
| Qataris | 304 380 | 104 | 294 206 | 0.35 (0.29 to 0.43) | ||
*Cohorts were exact matched one-to-one by sex, 10-year age groups, comorbidity count, testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
†Cox regression analysis adjusted for sex, 10-year age groups, comorbidity count, SARS-CoV-2 testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
‡CMW population includes Bangladeshis, Indians, Nepalese, Pakistanis and Sri Lankans. Urban population includes all other expatriate nationalities residing in Qatar.
CMW, craft and manual worker.
Table 4.
HRs comparing risk of death for all-cause non-COVID-19 mortality in major nationality groups in Qatar relative to Qataris
| Pairwise comparison* | Cohort size | Deaths | Total follow-up time in person-years | Incidence rate of death per 1000 person-years (95% CI) |
Unadjusted HR (95% CI) |
Adjusted HR (95% CI)† |
| Bangladeshis versus Qataris | ||||||
| Bangladeshis | 91 282 | 145 | 97 020 | 1.49 (1.27 to 1.76) | 0.53 (0.44 to 0.65) |
0.53 (0.44 to 0.65) |
| Qataris | 91 282 | 271 | 96 980 | 2.79 (2.48 to 3.15) | ||
| Filipinos versus Qataris | ||||||
| Filipinos | 134 246 | 131 | 130 981 | 1.00 (0.84 to 1.19) | 0.56 (0.45 to 0.69) |
0.56 (0.45 to 0.69) |
| Qataris | 134 246 | 235 | 130 930 | 1.79 (1.58 to 2.04) | ||
| Indians versus Qataris | ||||||
| Indians | 233 577 | 199 | 218 735 | 0.91 (0.79 to 1.05) | 0.38 (0.32 to 0.45) |
0.38 (0.32 to 0.44) |
| Qataris | 233 577 | 523 | 218 451 | 2.39 (2.20 to 2.61) | ||
| Nepalese versus Qataris | ||||||
| Nepalese | 81 185 | 65 | 85 130 | 0.76 (0.60 to 0.97) | 0.51 (0.38 to 0.68) |
0.51 (0.38 to 0.68) |
| Qataris | 81 185 | 128 | 85 110 | 1.50 (1.26 to 1.79) | ||
| CMW population‡ versus Qataris | ||||||
| CMW population | 267 863 | 412 | 257 908 | 1.60 (1.45 to 1.76) | 0.52 (0.46 to 0.58) |
0.51 (0.45 to 0.58) |
| Qataris | 267 863 | 798 | 257 629 | 3.10 (2.89 to 3.32) | ||
| Urban population‡ versus Qataris | ||||||
| Urban population | 304 380 | 877 | 294 500 | 2.98 (2.79 to 3.18) | 0.70 (0.64 to 0.77) |
0.70 (0.64 to 0.76) |
| Qataris | 304 380 | 1248 | 294 206 | 4.24 (4.01 to 4.48) | ||
*Cohorts were exact matched one-to-one by sex, 10-year age groups, comorbidity count, testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
†Cox regression analysis adjusted for sex, 10-year age groups, comorbidity count, SARS-CoV-2 testing method (PCR vs rapid antigen testing) and calendar week of the SARS-CoV-2 test.
‡CMW population includes Bangladeshis, Indians, Nepalese, Pakistanis and Sri Lankans. Urban population includes all other expatriate nationalities residing in Qatar.
CMW, craft and manual worker.
Adjusted HR comparing all-cause mortality relative to Qataris was lowest for Indians at 0.44 (95% CI 0.38 to 0.51) and highest for Filipinos at 0.71 (95% CI 0.59 to 0.87) (table 2). Adjusted HR comparing COVID-19 mortality relative to Qataris was lowest for Indians at 1.54 (95% CI 0.97 to 2.44) and highest for Nepalese at 5.34 (95% CI 1.56 to 18.34) (table 3). Adjusted HR comparing all-cause non-COVID-19 mortality relative to Qataris was lowest for Indians at 0.38 (95% CI 0.32 to 0.44) and highest for Filipinos at 0.56 (95% CI 0.45 to 0.69) (table 4).
Differences in mortality by socioeconomic population sector
Online supplemental table S3 describes baseline characteristics of matched cohorts in national, matched, retrospective cohort studies comparing incidence of death among each of the CMW and urban populations with incidence of death among Qataris.
Cumulative incidence of death for all-cause mortality, COVID-19 mortality and all-cause non-COVID-19 mortality is shown in figures 2 and 3 and online supplemental figure S2, respectively. Corresponding incidence rates are shown in tables 2–4, respectively. All-cause non-COVID-19 mortality was higher among Qataris than among the CMW and urban populations, but COVID-19 mortality was lower among Qataris. COVID-19 mortality among CMWs increased rapidly initially during the first epidemic wave (online supplemental figure S1), but the increase slowed down over time of follow-up (figure 3).
Adjusted HR comparing all-cause mortality relative to Qataris was 0.59 (95% CI 0.53 to 0.66) for the CMW population and 0.74 (95% CI 0.68 to 0.80) for the urban population (table 2). Adjusted HR comparing COVID-19 mortality relative to Qataris was 1.86 (95% CI 1.32 to 2.60) for the CMW population and 1.24 (95% CI 0.96 to 1.61) for the urban population (table 3). Adjusted HR comparing all-cause non-COVID-19 mortality relative to Qataris was 0.51 (95% CI 0.45 to 0.58) for the CMW population and 0.70 (95% CI 0.64 to 0.76) for the urban population (table 4).
Adjusted HRs by 3-month intervals since the start of follow-up suggested a declining trend for all-cause non-COVID-19 mortality, particularly for CMWs (online supplemental figure S3). At all follow-up intervals, adjusted HRs were <1 for both the CMW and urban populations.
Discussion
Risk of death is low in the population of Qatar at ~1 death for every 1000 individuals per year, reflecting the population’s young demographic structure,1 24 and the high Human Development Index of 0.848.28 However, differences were observed in the risk of death by nationality and socioeconomic population sector. For non-COVID-19 mortality, the risk of death was highest among Qataris and lowest among CMWs and the major expatriate nationality groups that comprise this part of the population (Bangladeshis, Indians and Nepalese). Differences in risk of death were smaller between Qataris and the urban population, perhaps reflecting closer similarity in socioeconomic status. Risk of death for each major nationality group in Qatar was also substantially lower than in the country of origin (table 1).
These findings may be explained by the healthy worker effect.29 30 CMWs are healthy by recruitment and maintain higher levels of physical activity. CMWs may also have lower levels of comorbidities, such as diabetes and obesity.31 Meanwhile, Qataris are a typical national population that includes both healthy and unhealthy individuals. Studies also suggest high prevalence of specific comorbidities or risk factors among Qataris, such as diabetes, obesity, hypertension and physical inactivity.31–36 Deaths due to road injuries may affect Qataris and the urban population more than CMWs. CMWs are unlikely to own cars, but use buses for transportation, unlike Qataris and the urban population who have high socioeconomic status and car ownership ratios. Studies suggest considerable incidence of traffic injuries in Qatar, with higher rates among Qataris.37–39
COVID-19 mortality was substantially higher among CMWs than among Qataris and the urban population. CMWs were the most affected population by the first epidemic wave (figure 3),3–5 9 19 20 before advent of more effective COVID-19 treatments and availability of vaccines, and thereby at higher risk of COVID-19 death. All subsequent waves occurred in 2021 and thereafter (online supplemental figure S1),12–16 after onset of the national COVID-19 mass vaccination campaign and coincident with availability of new treatments and improved case management.17 21 40 41 Although all COVID-19 healthcare, including testing, treatment, vaccination and acute care and intensive care unit hospitalisations, was accessible and provided free of charge equally for citizens and residents in the public healthcare system, lower health awareness among CMWs may have contributed to delays in infection diagnosis and presentation to healthcare facilities, which may have exacerbated risk of COVID-19 death. It remains unknown whether some of the observed differences in risk of COVID-19 death by nationality could be due to unobserved biological or behavioural differences.
Nevertheless, the COVID-19 death rate in Qatar has been one of the lowest worldwide.42 As of 30 September 2022, six hundred and eighty-two COVID-19 deaths have been recorded in this country; <0.1% of documented infections ended in death. COVID-19 death has been rare, with a cumulative incidence of only two deaths per 10 000 individuals after more than 2 years of follow-up (figure 1). The young age profile of the population, with only 9% being ≥50 years of age, may explain the low COVID-19 mortality.9 43 The well-resourced universal public healthcare system, which remained below its threshold even during peaks of epidemic waves, may have also contributed to low COVID-19 mortality.9 Emphasis on broad SARS-CoV-2 testing coupled with proactive, early treatment may also have limited the number of people who required hospitalisation or developed severe or critical disease.9
Study findings are not consistent with CMWs in Qatar experiencing an elevated risk of death due to occupational hazards, such as falls in construction sites or working under severe heat stress, as suggested elsewhere.44 Results of the present study highlight the importance of rigorous control of confounding factors in analysing and comparing mortality rates. For example, incidence rates of COVID-19 death were lowest among Nepalese at only 0.05 per 1000 person-years and highest among Qataris at 0.24 per 1000 person-years (table 1). However, after controlling for differences in sex, age and existing comorbid conditions in matched cohort studies comparing the various nationality subpopulations, adjusted HRs of COVID-19 death were highest among Nepalese and lowest among Qataris (table 3). Risk of COVID-19 death was 5.34-fold higher among Nepalese than among Qataris, opposite the result of the uncontrolled comparison. For a rigorous understanding of causes of death in Qatar, a national project has recently been initiated to methodologically review and analyse all deaths that occurred in Qatar, whether at healthcare facilities or elsewhere, since 2018. The project aims to provide a fine-grained understanding of causes of death in this country, including those that relate to occupational hazards.
This study has limitations. As an observational study, investigated cohorts were neither blinded nor randomised, so unmeasured or uncontrolled confounding cannot be excluded. The study analysed all deaths that occurred in Qatar since onset of the COVID-19 pandemic, but some deaths may have occurred outside Qatar, while expatriates were abroad, such as when visiting family in home countries. These out-of-Qatar deaths could introduce differential ascertainment bias if their rates differed for non-Qataris versus Qataris. Some expatriates may have left Qatar permanently because of end of employment or other reasons after initiation of follow-up, but travel data were not available for our analysis. With the restrictions on travel and international recruitment of labour during the pandemic, such movements in and out of the country were probably limited in scale in the early phases of the pandemic but increased with time as restrictions were gradually lifted. Mid to end of 2022 (towards the end of this study) in particular was a time during which such migration movements may have increased substantially as more CMWs may have left Qatar with the end of World Cup 2022 construction projects. Such migration movements can bias results due to differential loss of follow-up for non-Qataris versus Qataris, as Qataris are less likely to have permanently left Qatar.
The study investigated mortality during the COVID-19 pandemic, but mortality during the pandemic may have differed from that in earlier years, and may not be representative of incidence of death prior to the pandemic. For instance, occupational injuries may have declined in recent years.45–47 Public health restrictions imposed during the pandemic may have further reduced deaths due to occupational hazards, in addition to reducing other causes of death, such as road traffic injuries.
These sources of potential bias tend overall to underestimate all-cause non-COVID-19 mortality among non-Qataris, and perhaps more for CMWs. Analysis of non-COVID-19 mortality by time of follow-up appears consistent with an effect for differential ascertainment bias and/or loss of follow-up bias (online supplemental figure S3). However, the analysis also confirmed lower non-COVID-19 mortality for both the CMW and urban populations at all times of follow-up, including times right after recruitment into the cohort, when the effect of such biases is presumed minimal. It also seems unlikely that these sources of bias can fully explain the large observed differences in mortality rates.
The national SARS-CoV-2 testing database provided a sampling frame for the population of Qatar, but this database does not include individuals who had no SARS-CoV-2 test done since the pandemic onset. However, with different testing mandates and large volume of testing, it does not seem likely that any citizen or resident in Qatar has not had at least one SARS-CoV-2 test sometime since the start of the pandemic. The CMW and urban populations were defined based on nationality rather than occupation or socioeconomic indicators. However, nationality is strongly associated with both occupation and socioeconomic status in Qatar.3–5 9 19 The study estimated documented COVID-19 mortality, but COVID-19 may have also caused excess deaths indirectly,48 but these could not have been quantified using the present study design.
In conclusion, risk of both COVID-19 and non-COVID-19 deaths was low in Qatar during the pandemic, but there were differences in these risks by nationality and socioeconomic population sector. Risk of COVID-19 death was highest among CMWs and lowest among Qataris, largely reflecting differential exposure to the first epidemic wave, before advent of effective COVID-19 treatments and vaccines. Meanwhile, risk of non-COVID-19 death was highest among Qataris and lowest among CMWs, perhaps reflecting the healthy worker effect.
Acknowledgments
We acknowledge the many dedicated individuals at Hamad Medical Corporation, the Ministry of Public Health, the Primary Health Care Corporation, Qatar Biobank, Sidra Medicine and Weill Cornell Medicine–Qatar for their diligent efforts and contributions to make this study possible.
Footnotes
Handling editor: Seye Abimbola
Contributors: AAA, SS and LJA-R conceived and codesigned the study. AAA led the development and compilation of the national mortality database. HC codesigned the study, performed the statistical analyses and cowrote the first draft of the article. LJA-R led the statistical analyses and cowrote the first draft of the article. LJA-R accepts full responsibility for the work and the conduct of the study, and had access to the data, and decision to publish. All authors contributed to data collection and acquisition, database development, discussion and interpretation of the results and the writing of the manuscript. All authors have read and approved the final manuscript.
Funding: The authors are grateful for institutional salary support from the Biomedical Research Program and the Biostatistics, Epidemiology, and Biomathematics Research Core, both at Weill Cornell Medicine–Qatar, as well as for institutional salary support provided by the Ministry of Public Health, Hamad Medical Corporation and Sidra Medicine. The authors are also grateful for the Qatar Genome Programme and Qatar University Biomedical Research Center for institutional support for the reagents needed for the viral genome sequencing.
Disclaimer: The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the article. Statements made herein are solely the responsibility of the authors.
Competing interests: AAB has received institutional grant funding from Gilead Sciences unrelated to the work presented in this paper.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. The data set of this study is a property of the Qatar Ministry of Public Health that was provided to the researchers through a restricted access agreement that prevents sharing the data set with a third party or publicly. The data are available under restricted access for preservation of confidentiality of patient data. Access can be obtained through a direct application for data access to Her Excellency, Minister of Public Health (https://www.moph.gov.qa/english/OurServices/eservices/Pages/Governmental-HealthCommunication-Center.aspx). The raw data are protected and are not available due to data privacy laws. Aggregate data are available within the paper and its supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Hamad Medical Corporation (HMC IRB number: MRC-01-20-1078) and Weill Cornell Medicine–Qatar (WCM-Q IRB number: 20-00017) Institutional Review Boards approved this retrospective study with a waiver of informed consent.
References
- 1. Planning and Statistics Authority- State of Qatar . Qatar monthly statistics. Available: https://www.psa.gov.qa/en/pages/default.aspx [Accessed 26 May 2020].
- 2. Planning and Statistics Authority- State of Qatar . Labor force sample survey. Available: https://www.psa.gov.qa/en/statistics/Statistical%20Releases/Social/LaborForce/2017/statistical_analysis_labor_force_2017_En.pdf [Accessed 1 May 2020].
- 3. Coyle PV, Chemaitelly H, Ben Hadj Kacem MA, et al. SARS-cov-2 seroprevalence in the urban population of Qatar: an analysis of antibody testing on a sample of 112,941 individuals. IScience 2021;24:102646. 10.1016/j.isci.2021.102646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Al-Thani MH, Farag E, Bertollini R, et al. SARS-cov-2 infection is at herd immunity in the majority segment of the population of Qatar. Open Forum Infect Dis 2021;8:ofab221. 10.1093/ofid/ofab221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jeremijenko A, Chemaitelly H, Ayoub HH, et al. Herd immunity against severe acute respiratory syndrome coronavirus 2 infection in 10 communities, Qatar. Emerg Infect Dis 2021;27:1343–52. 10.3201/eid2705.204365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Bel-Air F. Demography, migrationand labour market in Qatar. 2018. Available: https://www.researchgate.net/publication/323129801_Demography_Migration_and_Labour_Market_in_Qatar-_UPDATED_June_2017
- 7. Planning and Statistics Authority-State of Qatar . The simplified census of population, housing & establishments. Available: https://www.psa.gov.qa/en/statistics/Statistical%20Releases/Population/Population/2018/Population_social_1_2018_AE.pdf [Accessed 2 Apr 2020].
- 8. Priya Dsouza Communications . Population of Qatar by nationality-2019 report. 2019. Available: https://priyadsouza.com/population-of-qatar-by-nationality-in-2017/ [Google Scholar]
- 9. Abu-Raddad LJ, Chemaitelly H, Ayoub HH, et al. Characterizing the Qatar advanced-phase SARS-cov-2 epidemic. Sci Rep 2021;11. 10.1038/s41598-021-85428-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Al Kuwari HM, Abdul Rahim HF, Abu-Raddad LJ, et al. Epidemiological investigation of the first 5685 cases of SARS-Cov-2 infection in Qatar, 28 February-18 April 2020. BMJ open 2020;10:e040428. 10.1136/bmjopen-2020-040428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abu-Raddad LJ, Chemaitelly H, Coyle P, et al. SARS-cov-2 antibody-positivity protects against reinfection for at least seven months with 95 % efficacy. EClinicalMedicine 2021;35:100861. 10.1016/j.eclinm.2021.100861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abu-Raddad LJ, Chemaitelly H, Ayoub HH, et al. Introduction and expansion of the SARS-Cov-2 B.1.1.7 variant and Reinfections in Qatar: A nationally representative cohort study. Plos medicine 2021;18:e1003879. 10.1371/journal.pmed.1003879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chemaitelly H, Bertollini R, Abu-Raddad LJ. Efficacy of natural immunity against SARS-cov-2 reinfection with the beta variant. N Engl J Med 2021;385:2585–6. 10.1056/NEJMc2110300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chemaitelly H, Ayoub HH, Coyle P, et al. Protection of omicron sub-lineage infection against reinfection with another omicron sub-lineage. Nat Commun 2022;13. 10.1038/s41467-022-32363-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Altarawneh HN, Chemaitelly H, Ayoub HH, et al. Protective effect of previous SARS-cov-2 infection against omicron BA.4 and BA.5 subvariants. N Engl J Med 2022;387:1620–2. 10.1056/NEJMc2209306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chemaitelly H, Tang P, Coyle P, et al. Protection against Reinfection with the Omicron BA.2.75 Subvariant. The New England Journal of medicine 2023;388:665–7. 10.1056/NEJMc2214114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chemaitelly H, Tang P, Hasan MR, et al. Waning of bnt162b2 vaccine protection against SARS-cov-2 infection in Qatar. N Engl J Med 2021;385:e83. 10.1056/NEJMoa2114114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tang P, Hasan MR, Chemaitelly H, et al. BNT162b2 and mrna-1273 COVID-19 vaccine effectiveness against the SARS-cov-2 delta variant in Qatar. Nat Med 2021;27:2136–43. 10.1038/s41591-021-01583-4 [DOI] [PubMed] [Google Scholar]
- 19. Ayoub HH, Chemaitelly H, Seedat S, et al. Mathematical modeling of the sars-cov-2 epidemic in Qatar and its impact on the National response to covid-19. J Glob Health 2021;11:05005. 10.7189/jogh.11.05005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Abu-Raddad LJ, Dargham S, Chemaitelly H, et al. COVID-19 risk score as a public health tool to guide targeted testing: a demonstration study in Qatar. PLoS ONE 2022;17:e0271324. 10.1371/journal.pone.0271324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abu-Raddad LJ, Chemaitelly H, Ayoub HH, et al. Effect of mRNA vaccine boosters against SARS-Cov-2 Omicron infection in Qatar. The New England Journal of medicine 2022;386:1804–16. 10.1056/NEJMoa2200797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Altarawneh HN, Chemaitelly H, Ayoub HH, et al. Effects of previous infection and vaccination on symptomatic Omicron infections. The New England Journal of medicine 2022;387:21–34. 10.1056/NEJMoa2203965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chemaitelly H, Ayoub HH, Tang P, et al. Long-Term covid-19 booster effectiveness by infection history and clinical vulnerability and immune imprinting: a retrospective population-based cohort study. Lancet Infect Dis 2023:S1473-3099(23)00058-0. 10.1016/S1473-3099(23)00058-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. United nations population division . World population prospects. 2022. Available: https://esa.un.org/unpd/wpp/
- 25. World Health Organization (WHO) . International guidelines for certification and classification (coding) of COVID-19 as cause of death. Available: https://www.who.int/publications/m/item/international-guidelines-for-certification-and-classification-(coding)-of-covid-19-as-cause-of-death [Accessed 27 Feb 2023].
- 26. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics - Simulation and Computation 2009;38:1228–34. 10.1080/03610910902859574 [DOI] [Google Scholar]
- 27. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. JASA 1958;53:457–81. 10.1080/01621459.1958.10501452 [DOI] [Google Scholar]
- 28. UNDP . Human development report 2021-22. 2022. Available: http://report.hdr.undp.org [Accessed 1 Oct 2022].
- 29. Li CY, Sung FC. A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 1999;49:225–9. 10.1093/occmed/49.4.225 [DOI] [PubMed] [Google Scholar]
- 30. Chaabna K, Cheema S, Mamtani R. Migrants, healthy worker effect, and mortality trends in the Gulf cooperation Council countries. PLoS One 2017;12:e0179711. 10.1371/journal.pone.0179711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Awad SF, A Toumi A, A Al-Mutawaa K, et al. Type 2 diabetes epidemic and key risk factors in Qatar: a mathematical modeling analysis. BMJ Open Diabetes Res Care 2022;10:e002704. 10.1136/bmjdrc-2021-002704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Awad SF, Dargham SR, Toumi AA, et al. A diabetes risk score for Qatar utilizing a novel mathematical modeling approach to identify individuals at high risk for diabetes. Sci Rep 2021;11. 10.1038/s41598-021-81385-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Al-Thani MH, Al-Mutawa KA, Alyafei SA, et al. Characterizing epidemiology of prediabetes, diabetes, and hypertension in qataris: a cross-sectional study. PLoS One 2021;16:e0259152. 10.1371/journal.pone.0259152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Awad SF, O’Flaherty M, El-Nahas KG, et al. Preventing type 2 diabetes mellitus in Qatar by reducing obesity, smoking, and physical inactivity: mathematical modeling analyses. Popul Health Metr 2019;17:20. 10.1186/s12963-019-0200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Awad SF, O’Flaherty M, Critchley J, et al. Forecasting the burden of type 2 diabetes mellitus in Qatar to 2050: a novel modeling approach. Diabetes Res Clin Pract 2018;137:100–8. 10.1016/j.diabres.2017.11.015 [DOI] [PubMed] [Google Scholar]
- 36. Al-Thani MH, Sadoun E, Al-Thani A-A, et al. Change in the structures, dynamics and disease-related mortality rates of the population of Qatari nationals: 2007-2011. J Epidemiol Glob Health 2014;4:277–87. 10.1016/j.jegh.2014.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bener A. The neglected epidemic: road traffic accidents in a developing country, state of Qatar. Int J Inj Contr Saf Promot 2005;12:45–7. 10.1080/1745730051233142225 [DOI] [PubMed] [Google Scholar]
- 38. El-Menyar A, Consunji R, Abdelrahman H, et al. Predictors and time-based hospital mortality in patients with isolated and polytrauma brain injuries. World J Surg 2018;42:1346–57. 10.1007/s00268-017-4310-2 [DOI] [PubMed] [Google Scholar]
- 39. Bener A, Hussain SJ, Ghaffar A, et al. Trends in childhood trauma mortality in the fast economically developing state of Qatar. World J Pediatr 2011;7:41–4. 10.1007/s12519-010-0208-x [DOI] [PubMed] [Google Scholar]
- 40. Chemaitelly H, Ayoub HH, AlMukdad S, et al. Duration of mRNA vaccine protection against SARS-cov-2 omicron BA.1 and BA.2 subvariants in Qatar. Nat Commun 2022;13:3082. 10.1038/s41467-022-30895-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zaqout A, Almaslamani MA, Chemaitelly H, et al. Effectiveness of the neutralizing antibody sotrovimab among high-risk patients with mild-to-moderate SARS-cov-2 in Qatar. Int J Infect Dis 2022;124:96–103. 10.1016/j.ijid.2022.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johns Hopkins Coronavirus Resource . Mortality analyses. Available: https://coronavirus.jhu.edu/data/mortality [Accessed 0 Oct 2022].
- 43. Seedat S, Chemaitelly H, Ayoub HH, et al. SARS-cov-2 infection hospitalization, severity, criticality, and fatality rates in Qatar. Sci Rep 2021;11:18182. 10.1038/s41598-021-97606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pradhan B, Kjellstrom T, Atar D, et al. Heat stress impacts on cardiac mortality in nepali migrant workers in Qatar. Cardiology 2019;143:37–48. 10.1159/000500853 [DOI] [PubMed] [Google Scholar]
- 45. Al-Thani H, El-Menyar A, Consunji R, et al. Epidemiology of occupational injuries by nationality in Qatar: evidence for focused occupational safety programmes. Injury 2015;46:1806–13. 10.1016/j.injury.2015.04.023 [DOI] [PubMed] [Google Scholar]
- 46. Mekkodathil A, El-Menyar A, Kanbar A, et al. Epidemiological and clinical characteristics of fall-related injuries: a retrospective study. BMC Public Health 2020;20:1186. 10.1186/s12889-020-09268-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. International Labour Organization . One is too many: the collection and analysis of data on occupational injuries in Qatar. Available: https://www.ilo.org/beirut/countries/qatar/WCMS_828395/lang--en/index.htm [Accessed 3 Oct 2021].
- 48. Kiang MV, Irizarry RA, Buckee CO, et al. Every body counts: Measuring mortality from the COVID-19 pandemic. Annals of internal medicine 2020;173:1004–7. 10.7326/M20-3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-012291supp001.pdf (682.8KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The data set of this study is a property of the Qatar Ministry of Public Health that was provided to the researchers through a restricted access agreement that prevents sharing the data set with a third party or publicly. The data are available under restricted access for preservation of confidentiality of patient data. Access can be obtained through a direct application for data access to Her Excellency, Minister of Public Health (https://www.moph.gov.qa/english/OurServices/eservices/Pages/Governmental-HealthCommunication-Center.aspx). The raw data are protected and are not available due to data privacy laws. Aggregate data are available within the paper and its supplementary information.