Abstract
Objective: Since the advent of the Mulcahy technique of three-piece inflatable penile prosthesis (IPP) salvage, there have been multiple iterations of salvage prosthesis procedures reported in the literature. All of these techniques employ traditional antibiotic irrigation with or without rechanneling. We present our technique of salvage IPP using 0.05% chlorhexidine gluconate (Irrisept®) with corporal rechanneling for length preservation. Materials and Methods: Our technique of IPP salvage begins with access via a 5 cm vertical midline scrotal incision. Dissection down to the corpora is performed with a combination of blunt dissection and dissection with fine tipped Metzenbaum scissors. Each component of the prior IPP is sequentially removed starting with the cylinders, followed by the pump, and finally the reservoir. Irrisept® is used to copiously irrigate out both cavernosal bodies as well as the scrotal compartment and prior reservoir location. A two minute dwell time of the Irrisept® is employed after mechanical irrigation. A penrose drain is placed from the space of Retzius through a separate stab incision in the scrotum. Corporotomies are closed, followed by Dartos fascia and scrotal skin. A complete change in gown and gloves of all members of the surgical team and a new set of drapes and instruments is performed. Through a separate subcoronal incision, two new corporotomies are made and separate channels created using nine inch Metzenbaum scissors. These channels are irrigated with Irrisept®. A 9 mm malleable penile prosthesis (MPP) is inserted and corporotomies and skin incision are closed. Results: A total of four men with prior penoscrotal IPP placement underwent salvage IPP with MPP from January 2022 to October 2022. Median operative time was 165 minutes. Median preoperative cylinder size was 23.5 cm. Median postoperative malleable cylinder size was 23 cm. Median length of follow up was 4.8 months. There were no cases of MPP erosion or infection. Two patients elected to undergo repeat IPP insertion after 6 months with same cylinder size. Conclusion: IPP salvage with chlorhexidine irrigation and soak as well as separate corporal channeling in a noninfected field for MPP insertion is a viable strategy for infected prostheses given the ease of performance, low risk of repeat infection of the malleable device, and maintenance of corporal length of any subsequent prostheses.
Keywords: Erectile dysfunction, inflatable penile prosthesis, infection, chlorhexidine gluconate
Introduction
Since the advent of the Mulcahy technique of three-piece inflatable penile prosthesis (IPP) salvage, there have been multiple iterations of salvage prosthesis procedures reported in the literature [1,2]. All of these techniques employ traditional antibiotic irrigation with or without rechanneling. The original salvage technique involved explantation of the infected prosthesis, copious wound pressure irrigation with betadine, hydrogen peroxide, and kanamycin/bacitracin antibiotic solution, and immediate replacement with a new three piece prosthesis [3]. This technique resulted in an 82% infection-free salvage rate while at the same time minimizing corporal scarring and resultant penile shortening [3]. In the original series, 75% of patients were infected with S. epidermidis and this represented the landmark study dictating future antibiotic prophylaxis for prosthetic surgery [4].
Over time, the technique of wound irrigation and immediate reimplantation has been modified to include different antibiotic soaks as well as the use of malleable penile prosthesis (MPP) for preservation of corporal length. The malleable prosthesis can be exchanged at a later date, if patient desired, with a new three-piece device [1]. The benefit of salvaging with a MPP is avoiding the scrotal compartment altogether to allow for optimal healing, and to mitigate the risk of pump erosion and fistula formation through the scrotum [5]. What has been established to be most important in salvage prosthetic surgery is a vigorous mechanical (to remove biofilm) and antimicrobial irrigation (aimed at eradicating bacterial presence) lavage of the wound [6].
Irrisept® (Innovation Technologies, Inc., Lawrenceville, Georgia, USA) is a solution of .05% chlorhexidine gluconate that has been extensively studied in the orthopedic literature as a soaking solution for implants and devices [7,8]. Irrisept® has been shown to be an effective bactericidal method for skin sterilization by binding to anionic molecules in bacteria cell walls, further decreasing microbial load in vitro when compared to povidone iodine [9]. The solution causes minimal tissue reactivity and has a broad spectrum of action against gram positive bacteria, gram negative bacteria, and fungal organisms [10]. Furthermore, Irrisept® has experienced increased utilization by prosthetic urologists for their implant surgeries. However, there is no description of Irrisept® use in the salvage setting. We describe a case series of three-piece IPP salvage using Irrisept® as well as corporal rechanneling with MPP for corporal length preservation.
Methods
Explantation of infected device
Prior to surgical incision, patients are administered broad spectrum intravenous antibiotics, with ampicillin-sulbactam as our antibiotic of choice in the salvage setting given regional antibiogram. Our technique of IPP salvage begins with access via a 5 cm vertical midline scrotal incision (Figure 2). Dissection down to the corpora is performed with a combination of blunt dissection and dissection with fine tipped Metzenbaum scissors. When purulence is encountered, wound cultures are sent for microbial analysis and antibiotic sensitivity testing. Each component of the prior IPP is sequentially removed starting with the cylinders, followed by the pump, and finally the reservoir. The scrotal pseudocapsule around the pump and tubing is sharply excised.
Figure 2.
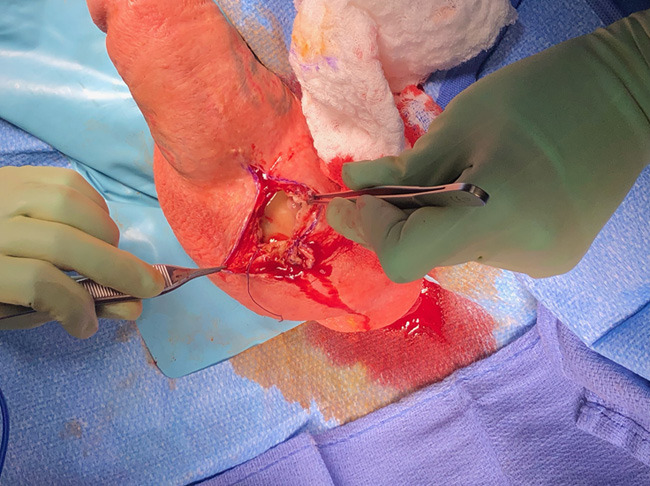
Vertical midline incision with access into scrotal compartment for IPP explantation.
Wound irrigation
Irrisept® is used to copiously irrigate both cavernosal bodies as well as the scrotal compartment and prior reservoir location. After mechanical irrigation and drainage, the wounds are flooded with Irrisept® and allowed to dwell for at least two minute as per the manufacturer recommendations [11]. A penrose drain is placed from the reservoir space, through the path of prior tubing and pump, and out via a separate stab incision on the most dependent part of the scrotum. The corpora are irrigated and corporotomies are closed using PDS sutures. The scrotum is closed in 2 layers and skin reapproximated using 3-0 chromic in a vertical mattress. The drapes are completely removed and discarded.
Malleable prosthesis insertion
All members of the surgical team change their gowns and gloves, and a new set of sterile instruments is used. The patient is then re-prepped and draped as if a virgin case were being performed. Care is taken to exclude the scrotum, and the prior scrotal incision, using antimicrobial iodophor impregnated adhesive incise drapes (3MTM IobanTM 2, St. Paul, MN, USA). At this point a separate subcoronal incision is made and the penis degloved to 3 cm proximal to the coronal sulcus, sharply and bluntly. Care is taken not to enter the scrotal compartment accessed during the explantation. Distal corporotomies are made approximately 3 cm distal to the penoscrotal junction and separate channels created using nine inch Metzenbaum scissors for corporal tunneling (Figure 1). These channels are irrigated with Irrisept® again. The authors prefer the smallest caliber MPP device to minimize postoperative priapismic pain caused from larger implants. A 9 mm MPP is inserted and corporotomies and skin incision closed. Penrose drain is removed after 48 hours. Patients are typically continued on an oral fluoroquinolone for a total of 7 days.
Figure 1.
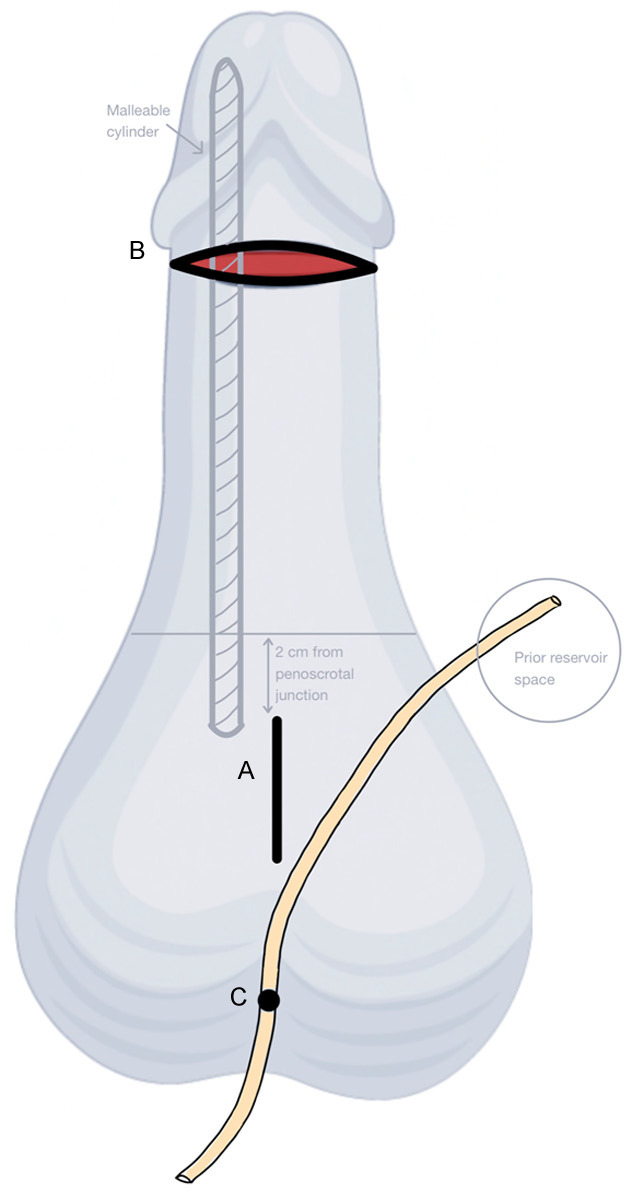
A. Location of vertical midline incision for initial IPP explant. B. Location of subcoronal incision for MPP insertion. C. Penrose shown exiting most dependent portion of scrotum. Proximal end of drain remains in space previously occupied by reservoir.
Results
A total of four men with prior penoscrotal IPP placement underwent salvage IPP with MPP from January 2022 to October 2022. At the time of initial IPP placement, all patients underwent prosthesis soak and surgical site irrigation with Irrisept® mixed with methylene blue. Methylene blue was utilized by the surgeon to better visualize the coating of the solution on the prosthesis device.
None of the infected devices had evidence of overlying skin necrosis or device erosion. At the time of IPP salvage surgery, median operative time was 165 minutes. Median preoperative cylinder size was 23.5 cm. Median postoperative cylinder size was 23 cm. Median follow-up was 7.1 months. There were no cases of subsequent MPP erosion or infection. After 6 months, patients were offered exchange of MPP for a new IPP. Ultimately, two patients successfully underwent repeat IPP insertion with the same cylinder size as their original IPP. Two explanted prostheses grew pansensitive Prevotella bivia. The remaining two implants had no growth on wound cultures.
Discussion
Rates of reinfection after salvage IPP range from 3-20% using the standard Mulcahy technique and other antibiotic modifications [1]. Utilization of a malleable implant in place of a three-piece prosthesis was first described at length in a multicenter series by Gross et al. and reported a 93% infection free rate with subsequent rate of replacement to three-piece IPP of 31%. This suggests that over two-thirds of patients are content with their malleable devices after salvage [12].
Our technique employs the same principles of mechanical irrigation and antiseptic dwell time, however there are some distinctions. We perform MPP insertion through two separate incisions with separate corporal tunneling. This is an attempt to ensure that the implanted MPP does not occupy the same channel previously occupied by the infected IPP. We believe this further decreases the risk of repeat prosthetic infection by avoiding or incising the existing pseudocapsule and potentially its associated biofilm. Additionally, we irrigate the corporal bodies, pump location, and retropubic space where the reservoir sits. If a Jackson-Pratt (JP) drain is placed, then further irrigation with Irrisept® and clamping of the JP tubing can allow for appropriate dwell time of the solution within the reservoir cavity, with subsequent drainage once reconnected to suction.
Chlorhexidine gluconate (CHG) is a cationic bisbiguanide salt and the Irrisept® solution is kept at a pH of 5.0-7.0. CHG works by destroying the bacterial cell membrane and precipitating cell contents. The attraction of the positively charged CHG molecule to negatively charged bacterial cell wall causes disruption of the cell membrane and subsequent cellular death [13]. While we have employed Irrisept® as the sole antimicrobial agent for prosthetic coating and wound irrigation for over one year, we believe that our initial practice of mixing with methylene blue for improved visualization (Irrisept® is clear) caused neutralization of the solution and thus rendered its anti-microbial qualities ineffective. We hypothesize that this combination of Irrisept® and methylene blue selected for unique bacterial morphotypes such as Prevotella, an organism more commonly seen in oral, vaginal, and gastrointestinal flora [14]. Historically the most common microbes found at the time of IPP salvage were skin flora, specifically staphylococcal and streptococcal species, and urinary tract organisms such as Escherichia and Klebsiella [15,16]. As such, we strongly recommend against mixing any other agent to Irrisept® solution. Subsequent salvage procedures using Irrisept® as described in this manuscript were performed without mixing with other agents.
Conclusion
Three-piece penile prosthesis salvage with chlorhexidine irrigation and soak as well as separate corporal channeling in a noninfected field for MPP insertion is a viable strategy for infected prostheses given the ease of performance, low risk of repeat infection of the malleable device, and maintenance of corporal length and space for any subsequent IPP exchange.
Disclosure of conflict of interest
None.
References
- 1.Mellon MJ, Broghammer JR, Henry GD. The Mulcahy salvage: past and present innovations. J Sex Med. 2015;12(Suppl 7):432–6. doi: 10.1111/jsm.12986. [DOI] [PubMed] [Google Scholar]
- 2.Swanton AR, Gross MS, Munarriz RM, Mulcahy JJ. Penile prosthesis salvage: a historical look at the Mulcahy technique and a review of the latest literature. Int J Impot Res. 2022 doi: 10.1038/s41443-021-00515-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Mulcahy JJ. Long-term experience with salvage of infected penile implants. J Urol. 2000;163:481–2. [PubMed] [Google Scholar]
- 4.Brant MD, Ludlow JK, Mulcahy JJ. The prosthesis salvage operation: immediate replacement of the infected penile prosthesis. J Urol. 1996;155:155–7. doi: 10.1016/s0022-5347(01)66580-7. [DOI] [PubMed] [Google Scholar]
- 5.Köhler TS, Modder JK, Dupree JM, Bush NC, McVary KT. Malleable implant substitution for the management of penile prosthesis pump erosion: a pilot study. J Sex Med. 2009;6:1474–8. doi: 10.1111/j.1743-6109.2009.01236.x. [DOI] [PubMed] [Google Scholar]
- 6.Darouiche RO, Bella AJ, Boone TB, Brock G, Broderick GA, Burnett AL, Carrion R, Carson C 3rd, Christine B, Dhabuwala CB, Hakim LS, Henry G, Jones LA, Khera M, Montague DK, Nehra A. North American consensus document on infection of penile prostheses. Urology. 2013;82:937–42. doi: 10.1016/j.urology.2013.05.048. [DOI] [PubMed] [Google Scholar]
- 7.Premkumar A, Nishtala SN, Nguyen JT, Bostrom MPG, Carli AV. The AAHKS best podium presentation research award: comparing the efficacy of irrigation solutions on staphylococcal biofilm formed on arthroplasty surfaces. J Arthroplasty. 2021;36:S26–S32. doi: 10.1016/j.arth.2021.02.033. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqi A, Abdo ZE, Springer BD, Chen AF. Pursuit of the ideal antiseptic irrigation solution in the management of periprosthetic joint infections. J Bone Jt Infect. 2021;6:189–198. doi: 10.5194/jbji-6-189-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Driesman A, Shen M, Feng JE, Waren D, Slover J, Bosco J, Schwarzkopf R. Perioperative chlorhexidine gluconate wash during joint arthroplasty has equivalent periprosthetic joint infection rates in comparison to betadine wash. J Arthroplasty. 2020;35:845–848. doi: 10.1016/j.arth.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Lung BE, Le R, Callan K, McLellan M, Issagholian L, Yi J, McMaster WC, Yang S, So DH. Chlorhexidine gluconate lavage during total joint arthroplasty may improve wound healing compared to dilute betadine. J Exp Orthop. 2022;9:67. doi: 10.1186/s40634-022-00503-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irrimax Corporation. Wound Debridement Instructions for Use. Irrisept Antimicrobial Lavage. 2022. https://www.irrisept.com/irrisept/overview/directions-for-use/
- 12.Gross MS, Phillips EA, Balen A, Eid JF, Yang C, Simon R, Martinez D, Carrion R, Perito P, Levine L, Greenfield J, Munarriz R. The malleable implant salvage technique: infection outcomes after Mulcahy salvage procedure and replacement of infected inflatable penile prosthesis with malleable prosthesis. J Urol. 2016;195:694–7. doi: 10.1016/j.juro.2015.08.091. [DOI] [PubMed] [Google Scholar]
- 13.McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12:147–79. doi: 10.1128/cmr.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tett A, Pasolli E, Masetti G, Ercolini D, Segata N. Prevotella diversity, niches and interactions with the human host. Nat Rev Microbiol. 2021;19:585–599. doi: 10.1038/s41579-021-00559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Licht MR, Montague DK, Angermeier KW, Lakin MM. Cultures from genitourinary prostheses at reoperation: questioning the role of staphylococcus epidermidis in periprosthetic infection. J Urol. 1995;154:387–90. [PubMed] [Google Scholar]
- 16.Palmisano F, Boeri L, Ievoli R, Sánchez-Curbelo J, Spinelli MG, Gregori A, Granata AM, Ruiz-Castañé E, Montanari E, Sarquella-Geli J. Ten-year experience with penile prosthetic surgery for the treatment of erectile dysfunction: outcomes of a tertiary referral center and predictors of early prosthetic infection. Asian J Androl. 2022;24:32–39. doi: 10.4103/aja.aja_27_21. [DOI] [PMC free article] [PubMed] [Google Scholar]


