Fig. 1 |. Herniation syndromes.
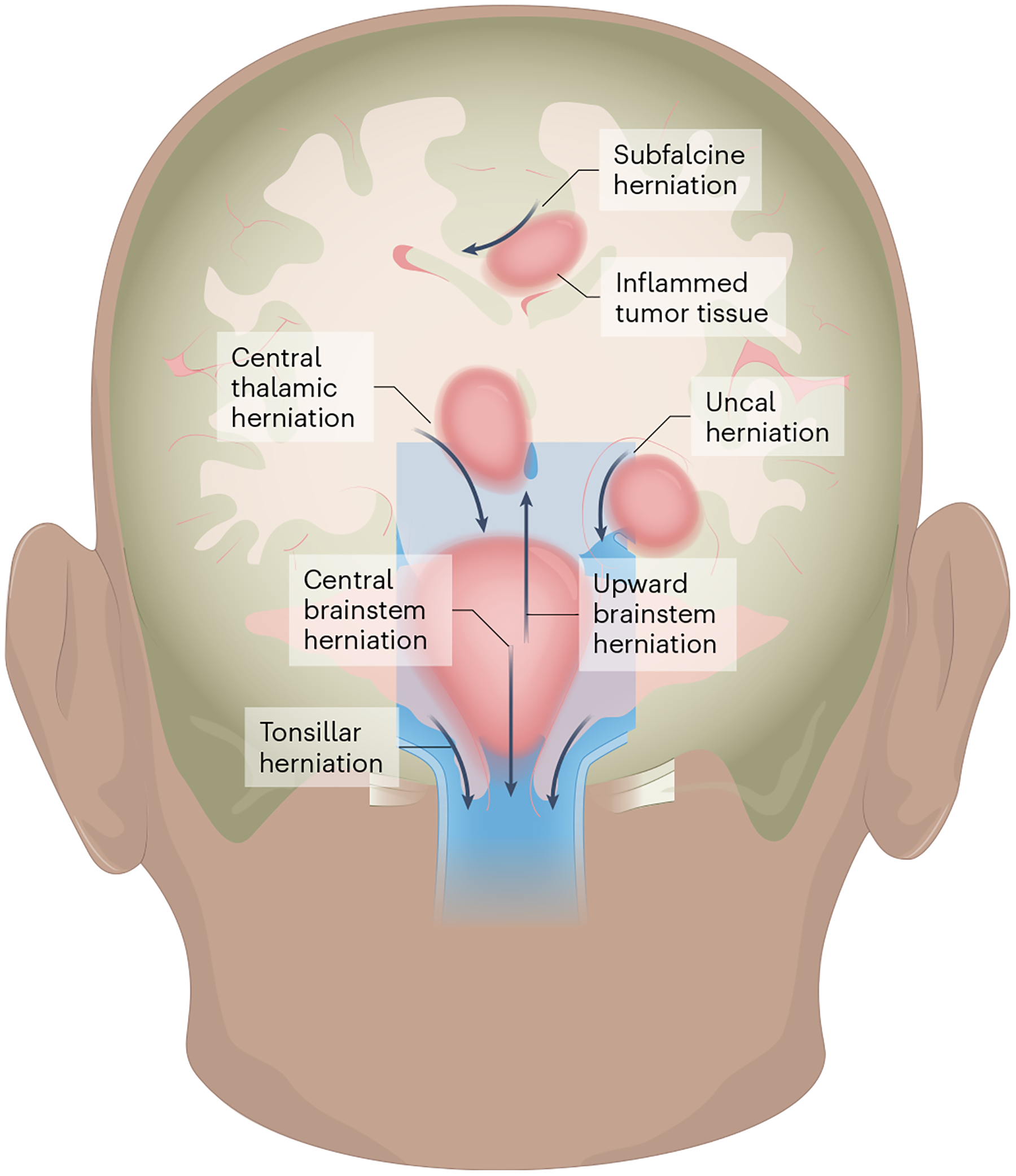
Edema caused by localized therapy-related inflammation depends on the location of the tumor (dark pink) and can cause herniation of brain tissue in the direction indicated by the arrows. Subfalcine herniation: arises when the peri-tumor mass effect compresses and displaces the cingulate gyrus under the falx cerebri and can clinically manifest with altered mental status, aphasia and contralateral leg weakness. Central thalamic herniation: represents downward displacement through the notch of the tentorium cerebelli and resulting compression of the diencephalon, which can lead to decreased arousal and coma. Uncal herniation: occurs when there is downward, transtentorial displacement of the uncus with consequent compression of the midbrain, resulting in a fixed and dilated pupil, a cranial nerve III palsy resulting in a ‘down and out’ eye, and new onset of hemiparesis. Upward brainstem herniation: occurs when a posterior fossa tumor pushes the cerebellar vermis and midbrain upwards, causing herniation through the tentorial notch with impairment of vertical eye movements and decreased level of consciousness. Central brainstem herniation: occurs when there is downward displacement of the brainstem, which can lead to Cushing’s triad (hypertension, bradycardia, abnormal respirations), a decreased level of consciousness (somnolence, with decreased response to noxious stimuli) and pathologic posturing. Tonsillar herniation: occurs because of compression of the cerebellar tonsils against the medulla and through the foramen magnum, compressing the medulla and resulting in Cushing’s triad, a decreased level of consciousness and pathologic extensor posturing36. Dural structures are shown in light blue, CSF in darker blue. The illustration was created by SciStories LLC.
