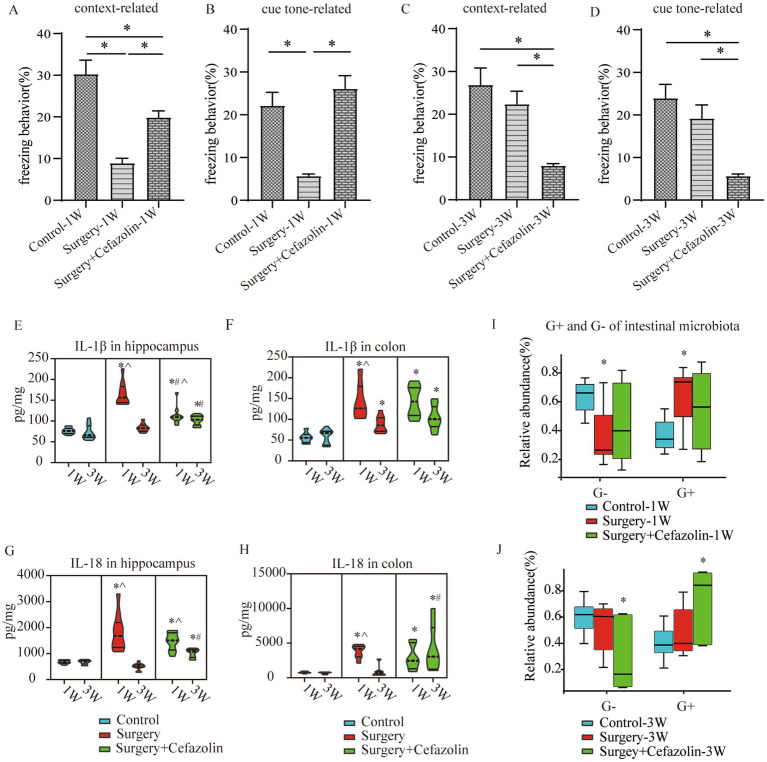
Figure 2.
Surgery/anesthesia stress-induced and perioperative cefazolin-induced gut dysbacteria, inflammation, and cognitive dysfunction, respectively. (A,B) Surgery/anesthesia stress decreased context-related (q = 9.737, p < 0.0001) and cue tone-related (q = 6.635, p = 0.0002) freezing behavior at 1 week, while cefazolin could improve context-related (q = 4.996, p = 0.0041) and cue tone-related (q = 8.229, p < 0.0001) freezing behavior (n = 10, ANOVA with Tukey’s multiple comparisons test). (C,D) At 3 weeks after surgery, surgery/anesthesia stress-induced freezing behavior recovered, while cefazolin decreased context-related (vs. control, q = 6.671, p = 0.0002; vs. surgery, q = 5.078, p = 0.0036) and cue tone-related (vs. control, q = 7.029, p < 0.0001; vs. surgery, q = 5.193, p = 0.0029) freezing behavior (n = 10, ANOVA with Tukey’s multiple comparisons test). (E,F) ELISA: surgery/anesthesia stress increased the level of IL-1β in the hippocampus (q = 13.66, p < 0.0001) and colon (q = 6.832, p = 0.0004) at 1 week, respectively; at 3 weeks, only IL-1β in the colon (q = 4.177, p = 0.0171) was elevated by surgery/anesthesia stress; cefazolin could alleviate increasing IL-1β in the hippocampus (q = 8.005, p < 0.0001) at 1 week, but at 3 weeks, could enhance IL-1β in the hippocampus (q = 6.925, p = 0.0001) and colon (q = 6.437, p = 0.0003), respectively (n = 10, ANOVA with Tukey’s multiple comparisons test). (G,H) ELISA: surgery/anesthesia stress increased the level of IL-18 in the hippocampus (q = 7.902, p < 0.0001) and colon (q = 6.803, p = 0.0004) at 1 week, respectively; at 3 weeks, cefazolin could enhance IL-18 in the hippocampus (q = 8.352, p < 0.0001) and colon (q = 4.697, p = 0.0101), respectively (n = 10, ANOVA with Tukey’s multiple comparisons test). (I,J) Surgery/anesthesia stress increased the relative abundance of gram-positive bacteria (q = 0.0638, p = 0.0142) and decreased the relative abundance of gram-negative bacteria (q = 0.0638, p = 0.0142) of intestinal microbiota at 1 week. In contrast, cefazolin increased the relative abundance of gram-positive bacteria (q = 0.0733, p = 0.0244). It decreased the relative abundance of gram-negative bacteria (q = 0.0733, p = 0.0244) of intestinal microbiota at 3 weeks after surgery (n = 9, KW rank sum test with Wilcoxon rank sum test). G+: gram-positive bacteria; G−: gram-negative bacteria. *Compared with control, p < 0.05; #compared with surgery, p < 0.05; ^compared with 3 weeks, p < 0.05.