Abstract
Introduction
Women’s mental health has a significant impact on the health of society. Due to the prevalence of mental health problems in women with PCOS, this study aimed to determine the effect of cognitive behavioral therapy on depression and anxiety (primary outcomes) and quality of life (secondary outcomes) in women with polycystic ovary syndrome.
Methods
This randomized controlled trial was performed on 84 patients with PCOS referred to Al-Zahra Hospital in Tabriz-Iran, 2021. Participants were randomly assigned to intervention (n = 42) and control (n = 42) groups. Counseling with cognitive behavioral therapy was provided in 8 sessions of 60–90 min weekly in groups with 5 to 7 people in each group for the intervention group. Spielberger State-Trait Anxiety, Beck Depression, and Quality of Life Questionnaire for women with polycystic ovary syndrome (PCOSQ) were used to collect data. Independent t-test and ANCOVA were used to compare the outcomes between the two groups.
Results
After the intervention, based on ANCOVA test with adjusting the baseline values, mean scores of depression (mean difference (MD): -18.6; 95% confidence interval (95% CI): -19.4 to -17.8: P < 0.001), trait anxiety (MD: -15.0; 95% CI: -16.0 to -13.9; P < 0.001), and state anxiety (MD: -15.3; 95% CI: -16.2 to -14.3; P < 0.001), were significantly lower in the intervention group compared to the control group. The mean score of quality of life (MD: 19.25; 95% CI: 17.66 to 20.84; P < 0.001) was significantly higher in the intervention group compared to the control group.
Conclusion
This study showed that CBT was effective in reducing depression and anxiety and improving the quality of life. Therefore it is recommended that health care providers use this approach to improve the mental health and quality of life of women with PCOS.
Trial registration
Iranian Registry of Clinical Trials (IRCT): IRCT20110826007418N7. Date of registration: 25/10/2021. URL: https://en.irct.ir/trial/57348; Date of first registration: 25/10/2021.
Keywords: Polycystic ovary syndrome, Cognitive behavioral therapy, Depression, Anxiety, Quality of life
Background
Polycystic ovary syndrome is characterized by hyperandrogenism, polycystic ovary, oligomenorrhea, and amenorrhea. This syndrome is the most common endocrine disorder of women of reproductive age, and various factors are involved in its occurrence [1]. This disease may link to a genetic predisposition, influenced by environmental factors such as eating habits, lifestyle, and social status [2]. The prevalence of PCOS ranges between 2.2 and 26% in various countries, which can be due to different processes and methodologies in population-based studies [3]. The prevalence of this disease is between 7.1 and 14.6% in Iranian population [4]. Three criteria commonly used to evaluate the prevalence of polycystic ovary syndrome are NIH (National Institute of Health), AES (Androgen Excess Society), and Rotterdam. In some studies, PCOS is diagnosed on ultrasound modalities [5].
In PCOS, ovaries are enlarged and may contain multiple small cysts, with one or more symptoms of irregular menstruation, excessive hair growth, and infertility [6, 7]. The disease is associated with a wide range of symptoms related to reproductive and endocrine disorders. Obesity and insulin resistance are the main physiological features in patients with PCOS [8, 9]. According to studies, women with PCOS are more likely to suffer from mood disorders than healthy ones [10, 11]. Also, the prevalence of depression is higher 4–5 times in these patients [12].
Depression is one of the most important issues studied by psychologists, psychiatrists, and behavioral scientists worldwide [13]. According to the World Health Organization (WHO), depression is a common mental disorder associated with decreased mood, loss of interest, blameworthiness, worthlessness, sleep disturbance, eating problems, tiredness, and poor concentration. The prevalence of depression in women with PCOS is 37%, compared to 14.2% in healthy women [14]. PCOS is associated with inflammation; prolonged inflammation is associated with higher cortisol levels, which increases the risk of depression [15].
Anxiety is also a common mental condition today. It is an uncomfortable feeling of uneasiness and worry accompanied by physical symptoms such as shortness of breath, palpitations, high blood pressure, etc. [16]. Excessive and long-term anxiety is usually associated with physiological responses such as increased metabolism, cardiovascular function, and decreased immunity. The prevalence of anxiety symptoms is 42% in women with PCOS, compared to 8.5% in healthy women [14]. Secondary depression seems to be the most common anxiety complication [17]. Women with PCO also encounter fertility problems, leading to anticipatory anxiety about whether they can have children [18].
Relaxation, logotherapy, medication, and electroconvulsive therapy are proven to help treat people with anxiety and depression [19, 20]. Cognitive-behavioral therapy (CBT) is a combination of cognitive and behavioral approaches. CBT can help the patient recognize his distorted thoughts and ineffective behaviors. Skill acquisition and homework assignments are provided to change these thoughts and behaviors [21]. CBT is still at the forefront of psychological treatments for depressive disorders [22]. The mechanism of depression and anxiety in PCOS may be linked to the clinical features of PCOS, including obesity, insulin resistance, hyperandrogenism, inflammation, and infertility [23]. CBT is believed to repair processes that maintain depression and anxiety, such as rumination, overgeneralization, and self-focused attention [24].
So far, very little research has been done on the effect of psychological interventions, especially CBT, on depression and anxiety in women with PCOS [25, 26]; most of them have studied the prevalence and symptoms of the disease. Considering the impact of CBT on depression and anxiety and the high prevalence of mental issues in women with PCOS, we aimed to investigate the effect of this method on depression and anxiety (primary outcomes) and the quality of life (secondary outcome) of women with polycystic ovary syndrome. It was hypothesized that the CBT will alleviate depression and anxiety a well as it will improve quality of life in women with polycystic ovary syndrome.
Methods
Study design and participants
This randomized controlled trial with was performed in a parallel design on 84 patients with polycystic ovary syndrome referred to Al-Zahra Hospital in Tabriz-Iran, from July 2021 to October 2021.
Inclusion criteria included a minimum of secondary education, diagnosis of polycystic ovary syndrome by a gynecologist (hyperandrogenism, ovulatory dysfunction, and polycystic ovaries), and a medical record of PCOS. Exclusion criteria included having a history of mental illness according to the person’s statement, hypertension, iron deficiency anemia, diabetes, thyroid disease, epilepsy, pregnant and postpartum women.
In this study, the sample size was calculated based on both depression and anxiety variables using G-Power software. Based on the results of the study by Mehrabadi et al. (2018) [27] with considering m1 = 17.35 (mean score of anxiety before the intervention) and with a default reduction of 35% in anxiety score after the intervention (m2 = 11.27) SD1 = SD2 = 10.44, one-sided α = 0.05, power = 80%, sample size was calculated as 38 people in each group. The final sample size was 42, considering a drop-out rate of 10%. Based on the depression variable [25] with considering m1 = 20.35 (mean score of depression before the intervention) and with a default reduction of 35% in depression score after the intervention (m2 = 13.22), SD1 = SD2 = 9.82, one-sided α = 0.05, power = 90%, sample size was calculated as 34 people in each group. The final sample size was 37, considering a drop-out rate of 10%. The sample size calculated with the anxiety variable was higher; thus, the final sample size was 42 people in each group.
Sampling
The sampling was started after the approval of the Ethics committee of Tabriz University of Medical Sciences (IR.TBZED.REC.1400.229) and registration in Iranian Registry of Clinical Trials (IRCT20110826007418N7). The researcher was referred to the gynecology & infertility clinic of Al-Zahra Hospital and given the list of women with PCOS. She contacted them and briefly explained the goals and method of the research. They were assessed based on the inclusion and exclusion criteria. Eligible and willing women were invited to attend the clinic at a specific time. The goals and methods were fully explained at the meeting then a written consent form was signed by the ones willing to participate in the study. The questionnaires of Spielberger State-Trait Anxiety Inventory (STAI) and Beck Depression Inventory (BDI) were completed. Women who scored 35–65 on STAI and above 20 on BDI were included. Then the questionnaires of socio-demographic characteristics and quality of life for women with polycystic ovary syndrome (PCOSQ) were completed. Women scored 65 or higher on STAI were referred to a psychiatrist.
Randomization
The participants were divided into the intervention and control groups using block randomization, with 4 and 6 block sizes and an allocation ratio of 1:1; within each of these “blocks,” the conditions occurred in a random order. Random sequence generation was conducted by a person not involved in sampling and data collection. Opaque, sealed envelopes were used for allocation concealment. The envelopes were revealed sequentially as the participants entered the study.
Intervention
The researcher conducted the group counseling in 8 sessions of 60–90 min weekly with 5–7 women in each group in a quiet room. All health and safety protocols were observed to prevent the spread of COVID-19. Online counseling was also available for whom wanted to participate due to pandemic conditions; it was provided in eight calls of 45 min weekly. Additionally, the counseling was conducted in the native language. The content of the sessions included mood screening, introducing cognitive-behavioral patterns, practicing skills, challenging thoughts, generalizing and maintaining, following up, and evaluating after the intervention. The content of the sessions was as follows:
Session 1: The researcher attempted to establish a proper relationship with the participants. She explained the number and duration of each session, group rules, problem identification, cognitive-behavioral patterns, problem description, the concept of stress and its effects, objectives, and receiving feedback from counseling sessions.
Session 2: Mood checking, presenting the progressive muscle relaxation and its practice, homework assignment: planning for progressive muscle relaxation twice a day, and receiving feedback.
Session 3: Reviewing the cognitive-behavioral pattern according to the problem, mood checking, asking the participants to explain their issues, introduction of imagery practice, homework assignment: progressive muscle relaxation, and imagery practice.
Session 4: Mood checking, reviewing the imagery practice, introduction of the first three columns of the thought record sheet (situation – automatic thoughts - emotions and mood) and the concept of hot thoughts, practicing the sheet using one of the events of last week, homework assignment: imagery practice, and receiving feedback.
Session 5: Mood checking, discussing the treatment process, reviewing the homework, introducing cognitive distortions, completing the three columns of thought record sheet (situation - automatic thoughts - emotions and mood), identification and challenging hot thoughts, homework assignment: completing the three columns of thought record sheet, and receiving feedback.
Session 6: Mood checking, reviewing the homework, presenting thought challenging and the seven-column thought record sheet (situation – automatic thoughts - emotions and mood - confirming evidence - rejecting evidence - alternative thinking - re-evaluating), completing the columns during the session, introducing the concept of challenging hot thoughts, homework assignment: relaxation techniques, and receiving feedback.
Session 7: Mood checking, reviewing the homework, completing the seven-column thought record sheet, homework assignment: completing the seven-column thought record sheet, and receiving feedback.
Session 8: Mood checking, reviewing the homework and treatment process (cognitive behavioral techniques), prevention, introducing self-management sessions, homework assignment: self-management practice.
The validity of the intervention program (CBT sessions) was reviewed and approved by the research consultant professor (third author as a psychologist) and the reviewer of the research project (another psychologist). The control group received routine drug treatments related to the disease. After the intervention, STAI, BDI, and PCOSQ questionnaires were completed again by both groups.
Data collection tools
Socio-demographics and obstetric characteristics questionnaire, STAI, BDI, and PCOSQ were used for data collection before and after the intervention.
Socio-demographics and obstetric characteristics questionnaire
It included questions about the age, ethnicity, marital status, childbearing, the level of education and occupation of the couples, average length of the menstrual cycle, average days of menstruation, menstrual flow volume, income sufficiency, the impact of stress on life, disease symptoms, first supporter, sexual satisfaction, infertility and evaluations in this field, duration of pregnancy attempt, PCOS duration, and the treatments used. Content and face validity were used to determine the validity of this questionnaire. It was provided to the faculty members of Tabriz University of Medical Sciences; adjustments were made based on their feedback.
Spielberger state-trait anxiety inventory (STAI)
The concepts of state and trait anxiety were first presented by Cattell and then in further detail by Spielberger (1970). STAI has been used widely in clinical research. It includes separate self-assessment scales to measure state and trait anxiety. Scores 20–31 indicate mild anxiety, 32–42 moderate to low anxiety, 43–53 moderate anxiety, 54–64 moderately severe anxiety, and 65–75 severe anxiety. The Persian version of this tool had good validity and reliability in the research of Mehram (1373) and Panahi (1372) [28, 29].
Beck Depression Inventory (BDI)
BDI is a self-assessment questionnaire that measures the severity of depressive symptoms. It includes 21 items, each containing four options, scored on a scale of 0 to 3. A higher score indicates the severity of the symptoms. The minimum and maximum scores are 0 and 63, respectively. BDI is designed for people aged 13 and over [30]. Scores 0–13 indicate low depression, 14–19 mild depression, 20–28 moderate depression, and 29–63 severe depression [31]. In the study of Taheri et al., psychometric properties had a high internal consistency based on Cronbach’s alpha (0.93); the correlation coefficient was calculated as 0.81 [32] .
Quality of life questionnaire for women with polycystic ovary syndrome (PCOSQ)
PCOSQ was developed by Cronin et al. (1998) to measure the quality of life of women with PCOS. It consists of 26 items that evaluate five domains: emotions (items 2, 4, 6, 11, 14, 17, 18, 20), hirsutism (items 1, 9, 15, 16, 26), weight (items 3, 10, 12, 22, 24), infertility problems (items 5, 13, 23, 25), and menstrual problems (items 7, 8, 19, 21) [33]. The scoring is based on the 7-point Likert scale; 1: Intense / All Time − 7: No Problem / Never. A high score indicates a poorer quality of life. The Persian version of this questionnaire was presented by Amini et al. (2012); cronbach’s alpha coefficient was higher than 0.7 in the domains of emotions, hirsutism, weight, and infertility problems [33] .
In this study, the reliability of questionnaires was confirmed by testing on 20 people and determining internal consistency. Cronbach’s alpha coefficients were 0.894, 0.772, and 0.832 for STAI, BDI and PCOSQ.
Statistical analysis
Statistical analysis was performed using SPSS version 24. The normality of the quantitative data was assessed using the Kolmogorov-Smirnov (K-S) test. Independent t tests, chi-square, chi-square by trend and Fisher’s exact tests were used to assess the homogeneity of the study groups. To compare the groups in terms of mean scores of anxiety, depression, and quality of life, independent t-test was performed before the intervention and ANCOVA test after the intervention by adjusting baseline values. All analyses were performed based on Intention-to-Treat by including all randomized patients in the analysis, regardless of what intervention they received. P < 0.05 was considered significant.
Results
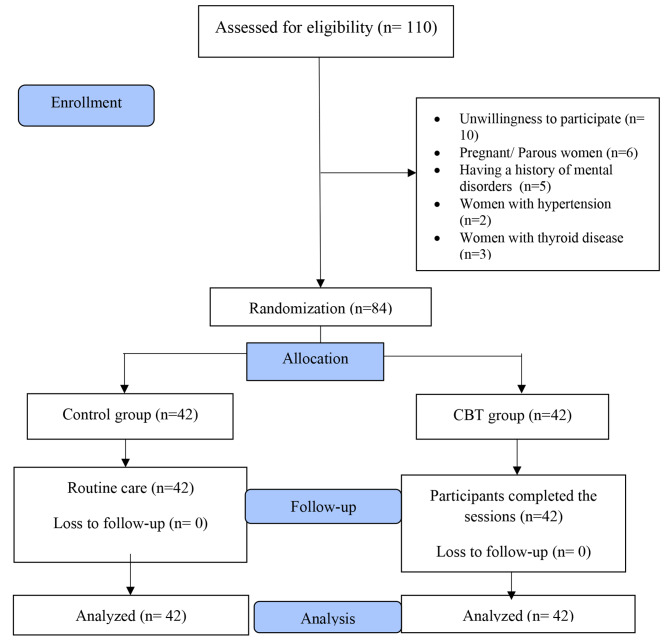
The sampling was conducted from July through October 2021. A total of 110 women were assessed in this study. 26 women were excluded from the study due to unwillingness to participate (n = 10), having a history of childbearing (n = 6), mental illness (n = 5), hypertension (n = 2), and thyroid disease (n = 3). Among the 84 women assigned to the CBT group, all participated in 8 counseling sessions; there was no dropout from the study (Fig. 1).
Fig. 1.
Flow chart of the study
The socio-demographic and obstetric characteristics of the participants are shown in Table 1. The mean (SD) age of the women was 30.3 (5.5) in the CBT group and 32.0 (4.8) in the control group. The average duration of pregnancy attempt was 5.0 (2.9) in the CBT group and 4.7 (2.5) in the control group. The average duration of the disease was 5.9 (4.8) in the CBT group and 6.8 (4.4) in the control group. The average duration of treatment was 5.0 (4.1) in the CBT group and 6.8 (4.4) in the control group. The majority of participants in both groups (97.6% in the CBT group and 97.7% in the control group) were Turk. Most of them (82.9% in the CBT group and 72.1% in the control group) were living in urban areas. All participants in the CBT group (100%) and 97.7% of the control group were married. About half of the women in the intervention group (43.9%) had a diploma; 44.2% of the control group had a university degree. Nearly half of the spouses in the control group (45.2%) had a university degree; more than a third of the intervention group (39%) had a diploma. The majority of participants in both groups (75.6% in the CBT group and 81% in the control group) had no history of childbearing. Most of them (90.2% in the CBT group and 96.8% in the control group) were housewives. Most women (92.7% in the CBT group and 83.7% in the control group) had menstrual periods of 3–7 days. The majority (75.6% in the CBT group and 83.7% in the control group) had menstrual cycles of 21–35 days. More than half of the patients in both groups (68.3% in the CBT group and 60.5% in the control group) had a moderate menstrual flow volume. More than half of them (68.3% in the CBT group and 60.5% in the control group) had somewhat sufficient income. The highest rate of complaints (53.7% in the CBT group and 72.1% in the control group) was related to infertility issues. More than half of the participants (70.7% in the CBT group and 51.2% in the control group) introduced their spouses as their first supporter. Most of them (92.6% in the CBT group and 95.2% in the control group) had moderate or complete satisfaction with their sexual lives. The majority of participants in both groups (97.6% in the CBT group and 97.6% in the control group) had infertility problems. Most of them in the intervention group (92.7%) and more than two thirds of the control group (66.7%) were not evaluated for infertility issues. There was no statistically significant difference between the groups in terms of socio-demographic and obstetric characteristics except for the couples occupation, stress role, and infertility evaluation, which was adjusted using ANCOVA (P < 0.05).
Table 1.
Social-demographic and obstetric characteristics of participants
| Characteristic | CBT* (n = 42) |
Control (n = 42) |
P-value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Age (Year) | 30.3 (5.5) | 32.0 (4.8) | 0.091† |
| Duration of pregnancy attempt (Year) | 5.0 (2.9) | 4.7 (2.5) | 0.55† |
| Duration of disease (Year) | 5.9 (4.8) | 6.8 (4.4) | 0.34† |
| Duration of treatment (Year) | 5.0 (4.1) | 6.8 (4.4) | 0.53† |
| Number (Percent) | Number (Percent) | ||
| Ethnicity | 1.0¥ | ||
| Turk | 40 (97.6) | 42 (97.7) | |
| Kurd | 1 (2.4) | 1 (2.3) | |
| Region | 0.23‡ | ||
| City | 34 (82.9) | 31 (72.1) | |
| Town | 7 (17.1) | 12 (27.9) | |
| Marital status | 1.0¥ | ||
| Single | 0 (0.0) | 1 (2.3) | |
| Married | 41 (100) | 42 (97.7) | |
| Spouse’s education | 0.37¥ | ||
| Elementary | 4 (9.8) | 2 (4.8) | |
| Intermediate | 2 (4.9) | 0 (0.0) | |
| High school | 7 (17.1) | 8 (19.0) | |
| Diploma | 16 (39.0) | 13 (31.0) | |
| University | 12 (29.3) | 19 (45.2) | |
| Having child | 0.55§ | ||
| Yes | 10 (24.4) | 8 (19.0) | |
| No | 31 (75.6) | 34 (81.0) | |
| Spouse’s job | 0.003¥ | ||
| Unemployed | 2 (4.9) | 0 (0.0) | |
| Worker | 18 (43.9) | 9 (21.4) | |
| Employee | 6 (14.6) | 10 (23.8) | |
| Shopkeeper | 3 (7.3) | 15 (35.7) | |
| Retired | 0 (0.0) | 0 (0.0) | |
| Other | 12 (29.3) | 8 (19.0) | |
| Woman job | 0.02§ | ||
| House wife | 37 (90.2) | 30 (96.8) | |
| Employed | 4 (9.8) | 13 (30.2) | |
| Woman education | 0.19‡ | ||
| Intermediate | 7 (17.1) | 4 (9.3) | |
| High school | 6 (14.6) | 9 (20.9) | |
| Diploma | 18 (43.9) | 11 (25.6) | |
| University | 10 (24.4) | 19 (44.2) | |
| Days of menstruation | 0.48¥ | ||
| < 3 days | 1 (2.4) | 4 (9.3) | |
| 3–7 days | 38 (92.7) | 36 (83.7) | |
| > 7 days | 2 (4.9) | 3 (7.0) | |
| Length of the menstrual cycle | 0.26¥ | ||
| < 21 days | 5 (12.2) | 1 (2.3) | |
| 21–35 days | 31 (75.6) | 36 (83.7) | |
| > 35 days | 5 (12.2) | 6 (14.0) | |
| Menstrual flow volume | 0.72¥ | ||
| Light | 4 (9.8) | 7 (16.3) | |
| Moderate | 28 (68.3) | 26 (60.5) | |
| Heavy | 9 (22.0) | 9 (20.9) | |
| Very heavy | 0 (0.0) | 1 (2.3) | |
| Income sufficiency | 0.10¥ | ||
| Not sufficient | 12 (29.3) | 10 (23.3) | |
| Somewhat sufficient | 28 (68.3) | 26 (60.5) | |
| Sufficient | 1 (2.4) | 7 (16.3) | |
| Stress Role | 0.003§ | ||
| Low | 8 (19.5) | 2 (4.7) | |
| Moderate | 15 (36.6) | 31 (72.1) | |
| High | 18 (43.9) | 10 (23.3) | |
| Disease symptoms | 0.21¥ | ||
| Obesity | 2 (4.9) | 4 (9.3) | |
| Hirsutism | 3 (7.3) | 2 (4.7) | |
| Acne | 3 (7.3) | 2 (4.7) | |
| Menstrual problems | 11 (26.8) | 4 (9.3) | |
| Infertility problems | 22 (53.7) | 31 (72.1) | |
| First supporter | 0.18¥ | ||
| Mother | 5 (12.2) | 10 (23.3) | |
| Father | 1 (2.4) | 1 (2.3) | |
| Mother & Father | 5 (12.2) | 10 (23.3) | |
| Spouse | 29 (70.7) | 22 (51.2) | |
| Health personnel | 1 (2.4) | 0 (0.0) | |
| Sexual satisfaction | 0.11¥ | ||
| Dissatisfied | 0 (0.0) | 0 (0.0) | |
| Rarely satisfied | 3 (7.3) | 2 (4.8) | |
| Somewhat satisfied | 19 (46.3) | 29 (69.0) | |
| Satisfied | 19 (46.3) | 11 (26.2) | |
| Infertility problems | 1.0¥ | ||
| Yes | 40 (97.6) | 41 (97.6) | |
| No | 1 (2.4) | 1 (2.4) | |
| Infertility evaluation | 0.003§ | ||
| Yes | 3 (7.3) | 14 (33.3) | |
| No | 38 (92.7) | 28 (66.7) |
* Cognitive Behavioral Therapy; †Independent t-test; ‡Chi-square for trend; §Chi-square; ¥ Fisher’s exact test
The mean (SD) depression score was 24.4 (5.0) before the intervention in the CBT group which decreased to 6.7 (4.3) after the intervention. It was 23.3 (3.2) and 24.5 (2.8) in the control group before and after the intervention, respectively. Based on the independent t-test, there was no statistically significant difference between the groups before the intervention (P = 0.25). Based on the ANCOVA test with adjusting the baseline scores, the mean depression score in the CBT group was significantly less than the control one after the intervention (MD: -18.6; 95% CI: -19.4 to -17.8; P < 0.001) (Table 2).
Table 2.
Comparison of the mean score of depression and anxiety among study groups
| Variable | CBT* (n = 42) Mean (SD†) |
Control (n = 42) Mean (SD†) |
Mean Difference (95% Confidence Interval) | P-value |
|---|---|---|---|---|
| Depression (Score range: 0 to 63) | ||||
| Before intervention | 24.4 (5.0) | 23.3 (3.2) | -1.0 (2.9 to 0.7) | 0.25‡ |
| After intervention | 6.7 (4.3) | 24.5 (2.8) | -18.6 (-19.4 to -17.8) | < 0.001§ |
| State anxiety (Score range: 20 to 80) | ||||
| Before intervention | 42.9 (2.9) | 42.2 (2.9) | 0.7 (-2.0 to 0.5) | 0.27‡ |
| After intervention | 29.0 (3.9) | 42.3 (2.8) | -15.3 (-16.2 to -14.3) | < 0.001§ |
| Trait anxiety (Score range: 20 to 80) | ||||
| Before intervention | 41.8 (2.8) | 41.1 (2.9) | 0.7 (-1.9 to 0.5) | 0.25‡ |
| After intervention | 29.3 (4.3) | 41.3 (2.9) | -15.0 (-16.0 to -13.9) | < 0.001§ |
* Cognitive Behavioral Therapy; † Standard Deviation; ‡Independent t-test; § ANCOVA with adjusting the baseline value and the variables of couples occupation, stress role, and infertility evaluation
The mean (SD) state anxiety score was 42.9 (2.9) before the intervention in the CBT group which decreased to 29.0 (3.9) after the intervention. It was 42.2 (2.9) and 42.3 (2.8) in the control group before and after the intervention, respectively. Based on the independent t-test, there was no statistically significant difference between the groups before the intervention (P = 0.27). According to the ANCOVA test and adjusting the baseline scores, the mean state anxiety score in the CBT group was significantly less than the control one after the intervention (MD: -15.3; 95% CI: -16.2 to -14.3; P < 0.001) (Table 2).
The mean (SD) trait anxiety score was 41.8 (2.8) before the intervention in the CBT group which decreased to 29.3 (4.3) after the intervention. It was 41.1 (2.9) and 41.3 (2.9) in the control group before and after the intervention, respectively. Based on the independent t-test, there was no statistically significant difference between the groups before the intervention (P = 0.25). According to the ANCOVA and adjusting the baseline scores, the mean trait anxiety score in the CBT group was significantly less than the control one after the intervention (MD: -15.0; 95% CI: -16.0 to -13.9; P < 0.001) (Table 2).
The mean (SD) quality of life score was 70.2 (13.3) before the intervention in the CBT group which increased to 89.0 (12.9) after the intervention. It was 71.9 (14.5) and 71.4 (4.1) in the control group before and after the intervention, respectively. Based on the independent t-test, there was no statistically significant difference between the groups before the intervention (P = 0.57). According to the ANCOVA with adjusting the baseline scores, the mean quality of life score in the CBT group was significantly more than the control one after the intervention (MD: 19.2; 95% CI: 17.6 to 20.8; P < 0.001). There was no statistically significant difference between the groups before the intervention in terms of quality of life domains. The mean score of all domains except hirsutism in the CBT group was significantly more than the control group after the intervention (Table 3).
Table 3.
Comparison of the mean scores of total quality of life and its subscales among study groups
| Variable | CBT* (n = 42) Mean (SD†) |
Control (n = 42) Mean (SD†) |
Mean Difference (95% Confidence Interval) | P-value |
|---|---|---|---|---|
| Hirsutism (Score range: 5 to 35) | ||||
| Before intervention | 14.8 (4.9) | 15.3 (6.1) | 0.5 (1.8 to 3.0) | 0.63‡ |
| After intervention | 14.5 (4.6) | 14.8 (6.1) | 0.3 (-0.5 to 0.9) | 0.61§ |
| Infertility problems (Score range: 4 to 28) | ||||
| Before intervention | 8.4 (3.4) | 9.8 (3.6) | 1.4 (1.0 to 2.9) | 0.06‡ |
| After intervention | 12.1 (2.8) | 9.4 (3.6) | 3.8 (3.0 to 4.6) | < 0.001§ |
| Weight (Score range: 5 to 35) | ||||
| Before intervention | 14.8 (3.9) | 13.7 (4.5) | 1.0 (2.9 to 0.7) | 0.24‡ |
| After intervention | 19.7 (3.9) | 14.3 (4.2) | 4.5 (3.5 to 5.4) | < 0.001§ |
| Emotions (Score range: 8 to 56) | ||||
| Before intervention | 21.9 (4.6) | 22.6 (5.3) | 0.7 (1.4 to 2.8) | 0.51‡ |
| After intervention | 29.2 (5.0) | 22.7 (4.7) | 7.1 (6.2 to 8.0) | < 0.001§ |
| Menstrual problems (Score range: 4 to 28) | ||||
| Before intervention | 10.1 (2.3) | 10.2 (2.6) | 0.03 (1.0 to 1.1) | 0.94‡ |
| After intervention | 13.3 (2.5) | 10.0 (2.5) | 3.3 (2.9 to 3.7) | < 0.001§ |
| Total Quality of life (Score range: 26 to 182) | ||||
| Before intervention | 70.2 (13.3) | 71.9 (14.5) | 1.7 (-4.3 to 7.7) | 0.57‡ |
| After intervention | 89.0 (12.9) | 71.4 (4.1) | 19.2 (17.6 to 20.8) | < 0.001§ |
* Cognitive Behavioral Therapy; † Standard Deviation; ‡Independent t-test; § ANCOVA with adjusting the baseline value and the variables of couples occupation, stress role, and infertility evaluation
Discussion
The results showed that CBT was effective in reducing depression and anxiety and promoting the quality of life of women with the PCOS.
CBT significantly reduced the mean depression score in this study. In a research by Rofey et al. (2009), women with PCOS, depression, and obesity participated in eight weekly CBT sessions focusing on lifestyle changes, medical history, and psychological education. The SECA (a calibrated weighing scale) and CDI (Children’s Depression Inventory) scales were used to measure changes in weight and depression. Follow-ups showed a significant decrease in mean weight and depression score after the intervention [34]. Correa et al. (2015) investigated the effect of the cognitive-behavioral approach on patients with PCOS. Beck Depression Inventory-II (BDI-II) questionnaire was used to measure the rate of depression before and after the intervention. The counseling sessions focused on teaching physiological and psychological symptoms, thought challenges, stress and anxiety management strategies, and self-concept. The mean score of depression was significantly reduced after the intervention; improvement of general function were also reported [35]. The results of both studies are in line with the present one. According to recent studies, the CBT approach can provide better improvements in depression than other approaches by affecting repetitive negative thinking (RNT) and focusing on reducing these thoughts [36]. It restructures negative thought patterns, corrects misconceptions, changes attentional direction, and creates adaptive coping thought patterns [37].
CBT significantly reduced the mean anxiety score in this study. Nobakht et al. (2018) investigated the effect of cognitive-behavioral counseling on anxiety in women with HIV. Six weekly counseling sessions were conducted based on a review of mood, awareness, self-image, and experiences, along with questions about the desire to change lifestyles, stress reduction strategies, mental focus, and relaxation. The Depression, Anxiety and Stress Scale (DASS-21) was used to measure anxiety. The results showed a significant reduction in anxiety scores and improvements in patient mood [38]. In a review study by Golshani et al. (2020), the results showed a significant reduction in the mean anxiety score in the intervention group with CBT in pregnant women with infertility history [39]. The results of both studies are consistent with the present one. CBT aims to stop negative cycles by breaking down issues that make the individual anxious or scared. Making concerns more manageable, CBT can help change negative patterns and improve feelings [40].
In this study, CBT significantly improved the mean score of quality of life in domains of menstrual problems, weight, infertility, and emotional problems. Cooney et al. (2018) studied the effect of CBT on obese women with PCOS and depressive symptoms. The counseling was provided in 8 sessions of 30 min weekly. PCOSQ scale was used to measure the quality of life before and after the intervention. The content of the sessions was based on planning and practicing cognitive skills such as identifying automatic thoughts and cognitive distortions. The participants in the counseling group reported a significant decrease in weight; the quality of life score was increased compared to the lifestyle change group [41]. Abdollahi et al. (2019) investigated the effect of cognitive-behavioral counseling on the quality of life of women with PCOS. The PCOSQ scale was used to measure the quality of life of study groups. The content of the meetings included cognitive-behavioral patterns, self-concept, breathing technique and timing, nutrition, lifestyle, muscle relaxation, stress management, and positive expression. After the intervention, the mean quality of life score in the counseling group increased significantly compared to the control group [25]. Another study by Jalilian et al. (2018) aimed to determine the effect of cognitive-behavioral counseling on the quality of life of women with PCOS. The PCOSQ scale was used to measure the quality of life in both groups. Counseling with CBT approach significantly improved the mean score of quality of life in hirsutism, weight, infertility, and emotional problems other than menstrual problems [42]. The results of all studies are consistent with the present one. CBT uses practical self-help strategies, designed to improve the quality of life. It focuses on increasing awareness, challenging thoughts, stress management skills, increasing hope, relaxation, and empowering women [43].
In recent years, psychological problems caused by PCOS has been drawn much attention from researchers worldwide. In addition to being a fertility and beauty issue for women, it can lead to psychological disorders such as depression and anxiety [44]. Physical symptoms caused by PCOS are one of the causes of psychological disorders in these women; they are three times more prone to psychological disorders and have a lower quality of life [45]. CBT approach can reduce depression and anxiety and improve the quality of life of women with PCOS using a combination of methods such as cognitive assessment techniques, identification of distortions, and coping skills [46].
Strengths and limitations
Observing all the principles of clinical trials, including random allocation and allocation concealment, was among the strengths of our study. Content design and consulting intervention were based on the cultural and moral values of the region. There was no drop-out from the study; all the participants were analyzed. Due to the nature of the intervention, blinding the participants, researcher, and outcome assessor was impossible.
Conclusion
In this study, CBT reduced the mean scores of anxiety and depression and improved the quality of life of women with PCOS. Due to the prevalence of mental disorders in these women, we recommend that health care providers develop programs based on CBT to promote the mental health and quality of life of women with PCOS.
Acknowledgements
The authors appreciate the assistance and cooperation of the participants of this study.
Abbreviations
- CBT
Cognitive-Behavioral Therapy
- ANCOVA
Analysis of Covariance
- 95% CI
95% confidence interval
- IRCT
Iranian Registry of Clinical Trials
- STAI
Spielberger State-Trait Anxiety Inventory
- BDI
Beck Depression Inventory
- PCOSQ
Quality of Life Questionnaire for women with polycystic ovary syndrome
- SD
standard deviation
Authors’ contributions
SM involved in the conception and design, acquisition of data and drafting the manuscript. PY (corresponding author) involved in the conception and design, acquisition of data, analysis of the data, interpretation of data and writing this manuscript. MF and MM involved in the conception and design, interpretation of the data and revising this manuscript. All authors gave their final approval of this version to be published.
Funding
This research is supported by Tabriz University of Medical Sciences. The funding source had no involvement in design of the study, data collection, data analysis, etc.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This research has been approved by the Ethics Committee of the Tabriz University of Medical Sciences, Tabriz, Iran (code number: IR.TBZED.REC.1400.229). All participants were ensured about the matter of confidentiality and signed the informed written consent form. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sheida Majidzadeh, Email: smajidzadeh30@gmail.com.
Mojgan Mirghafourvand, Email: mirghafourvand@gmail.com.
Mahmoud Farvareshi, Email: farvareshi.m@tbzmed.ac.ir.
Parisa Yavarikia, Email: yavarikiap@tbzmed.ac.ir.
References
- 1.Deeks AA, Gibson-Helm ME, Teede HJ. Anxiety and depression in polycystic ovary syndrome: a comprehensive investigation. Fertility and sterility. 2010;93(7):2421–2423. doi: 10.1016/j.fertnstert.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 2.Lim SS, Davies M, Norman RJ, Moran L. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Human reproduction update. 2012;18(6):618–637. doi: 10.1093/humupd/dms030. [DOI] [PubMed] [Google Scholar]
- 3.March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Human reproduction. 2010;25(2):544–551. doi: 10.1093/humrep/dep399. [DOI] [PubMed] [Google Scholar]
- 4.Behboodi Moghadam Z, Fereidooni B, Saffari M, Montazeri A. Polycystic ovary syndrome and its impact on iranian women’s quality of life: a population-based study. BMC women’s health. 2018;18(1):1–8. doi: 10.1186/s12905-018-0658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jonard S, Robert Y, Cortet-Rudelli C, Pigny P, Decanter C, Dewailly D: Ultrasound examination of polycystic ovaries: is it worth counting the follicles? Human reproduction 2003, 18(3):598–603. [DOI] [PubMed]
- 6.Barnard L, Ferriday D, Guenther N, Strauss B, Balen A, Dye L. Quality of life and psychological well being in polycystic ovary syndrome. Human reproduction. 2007;22(8):2279–2286. doi: 10.1093/humrep/dem108. [DOI] [PubMed] [Google Scholar]
- 7.Rashidi B, Haghollahi F, Shariat M, Zayerii F. The effects of calcium-vitamin D and metformin on polycystic ovary syndrome: a pilot study. Taiwan J Obstet Gynecol. 2009;48(2):142–147. doi: 10.1016/S1028-4559(09)60275-8. [DOI] [PubMed] [Google Scholar]
- 8.Association AP. Association, AP Diagnostic and statistical manual of mental disorders. Arlington, VA, US. In: American Psychiatric Publishing, Inc; 1995. [Google Scholar]
- 9.NASIRI AMIRI F, RAMEZANI TEHRANI F, SIMBAR M, THAMTAN M, ALI R. Concerns of women with polycystic ovary syndrome: a qualitative study. Iran. J. Endocrinol. Metab. 2013;15(1):41–51. [Google Scholar]
- 10.Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A: Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine 2018, 62(2):318–325. [DOI] [PubMed]
- 11.Kirmizi DA, Baser E, Onat T, Caltekin MD, Yalvac ES, Kara M, Gocmen AY: Sexual function and depression in polycystic ovary syndrome: is it associated with inflammation and neuromodulators? Neuropeptides 2020, 84:102099. [DOI] [PubMed]
- 12.Głowińska A, Zielona-Jenek M, Pawelczyk A, Banaszewska BE. Determinants of emotional problems and mood disorders in women with polycystic ovary syndrome. Ginekologia Polska. 2016;87(6):405–410. doi: 10.5603/GP.2016.0016. [DOI] [PubMed] [Google Scholar]
- 13.Azad-Marzabadi E, Salimi S. Study on job stress in a military unit. J Mil Med. 2005;6(4):279–284. [Google Scholar]
- 14.Dybciak P, Humeniuk E, Raczkiewicz D, Krakowiak J, Wdowiak A, Bojar I. Anxiety and depression in women with polycystic ovary syndrome. Medicina. 2022;58(7):942. doi: 10.3390/medicina58070942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farrell K, Antoni MH. Insulin resistance, obesity, inflammation, and depression in polycystic ovary syndrome: biobehavioral mechanisms and interventions. Fertility and sterility. 2010;94(5):1565–1574. doi: 10.1016/j.fertnstert.2010.03.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katzelnick DJ, Kobak KA, DeLeire T, Henk HJ, Greist JH, Davidson JR, Schneier FR, Stein MB, Helstad CP. Impact of generalized social anxiety disorder in managed care. Am.J. Psychiatry. 2001;158(12):1999–2007. doi: 10.1176/appi.ajp.158.12.1999. [DOI] [PubMed] [Google Scholar]
- 17.McKenna DJ, Jones K, Hughes K, Tyler VM: Botanical medicines: the desk reference for major herbal supplements: Routledge; 2012.
- 18.Cousineau TM, Domar AD. Psychological impact of infertility. Best practice & research Clinical obstetrics & gynaecology. 2007;21(2):293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Kajbaf MB, Ghasemiannejad Jahromi A, Ahmadi Forushani SH. The effectiveness of spiritual and existential group therapy on the rates of depression, death anxiety and afterlife belief among students: a study based on the reports of people with death experience. Knowledge & Research in Applied Psychology. 2017;16(4):4–13. [Google Scholar]
- 20.Shargh NA, Rostami B, Kosari B, Toosi Z, Majelan GA. Study of relationship between depression and quality of life in patients with chronic schizophrenia. Glob. J. Health Sci. 2016;8(3):224. doi: 10.5539/gjhs.v8n3p224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadock BJ: Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 2007.
- 22.Erickson TM, Newman MG. Cognitive behavioral psychotherapy for generalized anxiety disorder: a primer. Expert review of neurotherapeutics. 2005;5(2):247–257. doi: 10.1586/14737175.5.2.247. [DOI] [PubMed] [Google Scholar]
- 23.Ethirajulu A, Alkasabera A, Onyali CB, Anim-Koranteng C, Shah HE, Bhawnani N, Mostafa JA: Insulin resistance, hyperandrogenism, and its associated symptoms are the precipitating factors for depression in women with polycystic ovarian syndrome. Cureus 2021, 13(9). [DOI] [PMC free article] [PubMed]
- 24.Reddy YJ, Sudhir PM, Manjula M, Arumugham SS, Narayanaswamy JC. Clinical practice guidelines for cognitive-behavioral therapies in anxiety disorders and obsessive-compulsive and related disorders. Indian J. Psychiatry. 2020;62(Suppl 2):S230. doi: 10.4103/psychiatry.IndianJPsychiatry_773_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: a randomized controlled clinical trial. J Psychosom Obstet Gynaecol. 2019;40(4):283–293. doi: 10.1080/0167482X.2018.1502265. [DOI] [PubMed] [Google Scholar]
- 26.Phimphasone-Brady P, Palmer B, Vela A, Johnson RL, Harnke B, Hoffecker L, Coons HL, Epperson CN: Psychosocial interventions for women with polycystic ovarian syndrome: a systematic review of randomized controlled trials. F&S Reviews 2021.
- 27.Mehrabadi S, Jahanian Sadatmahalleh S, Kazemnejad A. Association of depression and anxiety with cognitive function in patients with polycystic ovary syndrome. J Mazandaran Univ Med Sci. 2017;27(147):159–170. [Google Scholar]
- 28.Gholami Booreng F, Mahram B, Kareshki H. Construction and validation of a scale of research anxiety for students. Iran J Psychiatry Behav Sci. 2017;23(1):78–93. [Google Scholar]
- 29.Panahi-shahri M: Spielberger State-Trait test standardization among students in Isfahan. MA thesis]. Tehran: Tarbiat-Modares University; 1994.
- 30.Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;1(42):559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA, Brown GK: BDI-II: Beck depression inventory: Pearson; 1996.
- 32.Hamidi R, Fekrizadeh Z, Azadbakht M, Garmaroudi G, Taheri Tanjani P, Fathizadeh S, Ghisvandi E. Validity and reliability Beck depression inventory-II among the iranian elderly population. J Sabzevar Univ Med Sci. 2015;22(1):189–198. [Google Scholar]
- 33.Cronin L, Guyatt G, Griffith L, Wong E, Azziz R, Futterweit W, Cook D, Dunaif A. Development of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS) J. Clin. Endocr. 1998;83(6):1976–1987. doi: 10.1210/jcem.83.6.4990. [DOI] [PubMed] [Google Scholar]
- 34.Rofey DL, Szigethy EM, Noll RB, Dahl RE, Lobst E, Arslanian SA. Cognitive–behavioral therapy for physical and emotional disturbances in adolescents with polycystic ovary syndrome: a pilot study. J. Pediatr. Psychol. 2009;34(2):156–163. doi: 10.1093/jpepsy/jsn057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Correa JB, Sperry SL, Darkes J. A case report demonstrating the efficacy of a comprehensive cognitive-behavioral therapy approach for treating anxiety, depression, and problematic eating in polycystic ovarian syndrome. Archives of women’s mental health. 2015;18(4):649–654. doi: 10.1007/s00737-015-0506-3. [DOI] [PubMed] [Google Scholar]
- 36.Spinhoven P, Klein N, Kennis M, Cramer AO, Siegle G, Cuijpers P, Ormel J, Hollon SD, Bockting CL. The effects of cognitive-behavior therapy for depression on repetitive negative thinking: a meta-analysis. Behaviour research and therapy. 2018;106:71–85. doi: 10.1016/j.brat.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 37.Roiser JP, Elliott R, Sahakian BJ. Cognitive mechanisms of treatment in depression. Neuropsychopharmacology. 2012;37(1):117–136. doi: 10.1038/npp.2011.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nobakht A, Mohraz M, Rahimzadeh M, Tehranizadeh M, Moghadam ZB, Saeieh SE. The effect of cognitive behavioural therapy on depression, anxiety, and stress in women with HIV. HIV & AIDS Review. Int J STD AIDS. 2018;17(3):218–223. [Google Scholar]
- 39.Golshani F, Mirghafourvand M, Hasanpour S, Biarag LS: The effect of cognitive behavioral therapy on anxiety and depression in iranian infertile women: a systematic and meta-analytical review. Iran J Psychiatry Behav Sci. 2020, 14(1).
- 40.Stallard P: Think good, feel good: a cognitive behavioural therapy workbook for children and young people: John Wiley & Sons; 2019.
- 41.Cooney LG, Milman LW, Hantsoo L, Kornfield S, Sammel MD, Allison KC, Epperson CN, Dokras A. Cognitive-behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome: a pilot randomized clinical trial. Fertility and sterility. 2018;110(1):161–171. doi: 10.1016/j.fertnstert.2018.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jalilian F, Kaboudi M, TehraniZadeh M, Naghizadeh Moghari F, Montazer A. The effect of cognitive behavioral counseling on quality of life in women with polycystic ovarian syndrome. Payesh (Health Monitor) 2018;17(6):667–676. [Google Scholar]
- 43.Ye M, Du K, Zhou J, Zhou Q, Shou M, Hu B, Jiang P, Dong N, He L, Liang S: A meta-analysis of the efficacy of cognitive behavior therapy on quality of life and psychological health of breast cancer survivors and patients. Psycho‐oncology 2018, 27(7):1695–1703. [DOI] [PubMed]
- 44.Jiskoot G, Timman R, Beerthuizen A, Dietz de Loos A, Busschbach J, Laven J. Weight reduction through a cognitive behavioral therapy lifestyle intervention in PCOS: the primary outcome of a randomized controlled trial. Obesity. 2020;28(11):2134–2141. doi: 10.1002/oby.22980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumarapeli V, Seneviratne RdA, Wijeyaratne C. Health-related quality of life and psychological distress in polycystic ovary syndrome: a hidden facet in south asian women. BJOG: Int J Gynaecol Obstet. 2011;118(3):319–328. doi: 10.1111/j.1471-0528.2010.02799.x. [DOI] [PubMed] [Google Scholar]
- 46.Jiskoot G, Benneheij S, Beerthuizen A, De Niet J, de Klerk C, Timman R, Busschbach J, Laven J. A three-component cognitive behavioural lifestyle program for preconceptional weight-loss in women with polycystic ovary syndrome (PCOS): a protocol for a randomized controlled trial. Reproductive health. 2017;14(1):1–12. doi: 10.1186/s12978-017-0295-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.