Abstract
Background:
Due to associated trauma, exposure to intimate partner violence (IPV) is considered a form of child maltreatment, and is associated with heightened risk for mental health problems.
Objective:
To evaluate associations between exposure to interparental IPV and the prospective development of borderline features in adolescents.
Participants and setting:
A diverse sample of 1,042 adolescents were recruited from public high schools throughout southeastern United States and followed annually for 5 years. Baseline mean age was 15.09 (SD = .79; range 13–18), and 56 % of the sample was female; 31.4 % (n = 327) were Hispanic, 29.4 % (n = 306) were White/not Hispanic, 27.9 % (n = 291) were African American, 3.6 % (n = 38) were Asian or Pacific Islander, and 7.7 % (n = 80) were mixed or another race.
Methods:
Exposure to interparental IPV and the quality of the parent-child relationship were assessed at baseline. Borderline features were assessed annually for the each of the five follow-up timepoints. Latent growth curve modeling was used to estimate the course of change of BPD features over time.
Results:
Consistent with expectations, and controlling for quality of parent-child relationships and sociodemographic confounds, findings demonstrated that IPV exposure related to both cross-sectional association between interparental IPV and adolescents’ borderline features and change in borderline features over a 5-year period.
Conclusion:
Adolescents who had witnessed interparental IPV were more likely to have higher levels of BPD features at baseline and to deviate from the typically observed normative decline in BPD features over the 4-year follow-up period.
Keywords: Interparental violence, Adolescents, Borderline personality disorder
1. Introduction
Borderline personality disorder (BPD) is a serious mental disorder found in ~1.7 % of the general population and in 15–28 % of patients in psychiatric clinics or hospitals (Gunderson, Skodol, & Zanarini, 2018). BPD is characterized by significant interpersonal problems, problems in self and identity, affective and behavioral dysregulation (American Psychiatric Association, 2013). It is unique from other forms of psychopathology in that BPD is conceptualized primarily as a disorder of interpersonal function (American Psychiatric Association, 2013; Sharp et al., 2015). Whereas interpersonal dysfunction is an outcome of most psychiatric disorders, interpersonal dysfunction forms the core of BPD from which all other symptoms flow (Bender & Skodol, 2007).
Until about a decade ago, BPD was considered exclusively a disorder of adulthood. However, significant advances were made recently in research supporting the validity and reliability of the BPD diagnosis in adolescents (Chanen, 2015; Sharp & Fonagy, 2015). This research has shown that adolescent BPD mirrors adult BPD in phenomenology, prevalence, course and etiology (Kaess, Brunner, & Chanen, 2014; Sharp & Romero, 2007), and has led to consensus that adolescent BPD constitutes an important public health concern (Chanen, Sharp, Hoffman, & Global Alliance for Prevention and Early Intervention for Borderline Personality Disorder, 2017). Indeed, research has shown that adolescent BPD is associated with increased risk for suicide (Brent et al., 1993; Crumley, 1979; Pompili, Girardi, Ruberto, & Tatarelli, 2005; Turner, Jin, Anestis, Dixon-Gordon, & Gratz, 2018; Yen, Gagnon, & Spirito, 2013), academic problems (Winograd, Cohen, & Chen, 2008), other psychopathology (Ha, Balderas, Zanarini, Oldham, & Sharp, 2014), and poor social and occupational outcomes (Winograd et al., 2008). Moreover, community-based studies of BPD have demonstrated a normative increase in borderline symptoms in adolescence with a normative decline thereafter into adulthood (Bornovalova, Hicks, Iacono, & McGue, 2009). However, a subgroup of adolescents appear to deviate from the normative decline in maladaptive traits as they age into young adulthood by either maintaining or elevating high levels of borderline traits (Biskin, Paris, Renaud, Raz, & Zelkowitz, 2011; Cohen et al., 2008; De Clercq, Verbeke, De Caluwé, Vercruysse, & Hofmans, 2017). Identifying factors that contribute to the development or increase in borderline features in adolescence is therefore of great clinical significance.
Due to the interpersonal nature of BPD, developmental models of BPD highlight the role played by the family environment in the emergence of BPD (Crowell, Beauchaine, & Linehan, 2009; Fonagy & Bateman, 2008). In these models, BPD is understood to develop as a function of complex interactions between dispositional traits (sensitive and emotionally reactive temperament) and an invalidating family environment (Fruzzetti, Shenk, & Hoffman, 2005). These models describe an invalidating family environment as one in which family members’ feelings, thoughts, concerns, fears and worries are disqualified. Disqualification may happen through psychological or emotional abuse, but will naturally also happen in the case of physical violence. As such, exposure to any physical violence in the family, including exposure to intimate partner violence (IPV) may be seen as an example of extreme dysfunction in familial interactions, and may heighten risk for the development and increase of BPD features in adolescents. However, as yet, exposure to IPV has not been empirically validated as a predictor for the development of IPV.
Several definitions of IPV exposure have been put forward (Graham-Bermann, Lynch, Banyard, DeVoe, & Halabu, 2007; Samuelson, Krueger, & Wilson, 2012). However, most often, IPV exposure is defined as when children see, hear, are directly involved in (i.e. attempt to intervene), or experience the aftermath of physical, emotional or sexual assaults that occur between their caregivers (Evans, Davies, & DiLillo, 2008). Twenty-six percent of children are exposed to IPV during their lifetimes and an estimated 15.5 million children currently live in families where IPV has occurred (Hamby, Finkelhor, Turner, & Ormrod, 2011). Interparental IPV includes IPV between caregivers or any kind, e.g. two grandparents, a father and his girlfriend, a mother and a grandmother, and so forth.
Physical IPV is often operationalized as acts of physical aggression (slapped, pushed, choked, knifed) directed at one’s intimate partner (e.g., (Narayan, Hagan, Cohodes, Rivera, & Lieberman, 2019). It is sometimes motivated by a partner’s attempt to coerce or control the other (Johnson, 1995; Whitaker, 2013). Indeed, family environments marked by physical IPV are also often characterized by coercive and controlling interactions between partners, which include direct attempts at invalidating self-esteem (Black et al., 2013; McFarlane, Symes, Binder, Maddoux, & Paulson, 2014; Robertson & Murachver, 2011). These coercive and controlling interactions between partners often extend to parent-child dyads, and they are positively related to physically and psychologically abusive behavior toward children (Haselschwerdt et al., 2019) as well as to the children’s behavioral and emotional problems (Jouriles & McDonald, 2015). In short, family environments marked by interparental IPV appear to share some of the same damaging characteristics as those theorized to promote the development of BPD.
Reviews of the literature consistently conclude that children who are exposed to physical IPV are at heightened risk for immediate and future emotional and behavioral problems (e.g. Evans et al., 2008; Kitzmann, Gaylord, Holt, & Kenny, 2003; Vu, Jouriles, McDonald, & Rosenfield, 2016; Wolfe, Crooks, Lee, McIntyre-Smith, & Jaffe, 2003). Indeed, IPV exposure is now defined as a form of child maltreatment due to the trauma associated with witnessing, hearing, or trying to intervene in domestic violence between partners (Gilbert et al., 2009). However, there has yet to be a study examining links between childhood exposure to interparental IPV and BPD among adolescents. Given the distinctive nature of adolescent BPD as a disorder of maladaptive interpersonal function, coupled with its significance in predicting other types of problems, this is an important gap in the research literature. Thus, the goal of the current study was to evaluate relations between exposure to interparental IPV and the prospective development of borderline features in adolescents. The value of a longitudinal design lies in the fact that positive findings may be interpreted as potential evidence for causality. Our main study hypothesis was that adolescents’ reports of exposure to interparental IPV during childhood would predict higher levels of BPD features over time, and that exposure to IPV would disrupt the normative decline typically observed in adolescence in community samples (Bornovalova et al., 2009). In addition, developmental models of BPD have identified the quality of the parent-child relationships as a major factor in the development of BPD (Crowell et al., 2009; Fonagy & Bateman, 2008). In particular, developmental models of BPD have argued that the quality of interaction and relationship between caregiver and child constitute the most important environmental factor for the development of BPD. In this study, we furthermore aimed to expand these ideas by showing that exposure to IPV among caregivers contributes to the development of borderline features above and beyond the impact of the quality of the caregiver-child relationship.
2. Methods
2.1. Participants
Participants were recruited from mandated classes (e.g., English, History) from seven public high schools in a large and diverse metropolitan city in the southeastern United States as part of a larger longitudinal study which focused on adolescent dating violence (Temple, Shorey, Tortolero, Wolfe, & Stuart, 2013. All students in these classes were eligible. Study personnel visited each class prior to enrollment to describe the purpose of the study and answer any questions. A parental permission form was sent home with students to give to their parents to review and sign. In addition, students had to assent to participate prior to study onset. After completing these active consent/assent procedures, the final sample consisted of 1042 freshman and sophomore students response rate = 62 %). Assessments took place during school hours and were completed on paper-and-pencil surveys in a private classroom without teachers or school staff present. Upon entering the study, mean age was 15.09 (SD = .79; range 13–18), 56 % of the sample was female, and 31.4 % (n = 327) were Hispanic, 29.4 % (n = 306) were White/not Hispanic, 27.9 % (n = 291) were African American, 3.6 % (n = 38) were Asian or Pacific Islander, and 7.7 % (n = 80) were mixed or another race. At baseline, 45.5 % of participants were living with both parents, 20.4 % were living with one parent and one step-parent, 27.6 % lived with a single parent (24 % lived with their mother only, compared to 3.6 % living with their father only), 3 % of the sample lived with their grandparents, and 3.5 % reported “other” as their current living situation. Additionally, 19.4 % of the sample reported ever receiving mental health treatment (4 % were currently receiving mental health treatment at baseline). About 30 % of parents completed college (30.3 % of mothers and 31.3 % of fathers), whereas 20.4 % of mothers and 23.1 % of fathers did not graduate from high school.
2.2. Measures
2.2.1. Borderline personality features
The 24-item Borderline Personality Feature Scale for Children (BPFS-C; Crick, Murray–Close, & Woods, 2005) was administered in years two through five of the current study. The BPFS-C was developed for use in youth as young as nine years of age and includes indicators of borderline features such as affective instability, identity problems, negative relationships, and self-harm. Item responses are on a 5-point Likert scale ranging from “not true at all” to “always true”. Example items include “I get into trouble because I do things without thinking” and “I feel that there is something important missing about me, but I don’t know what it is.” All items are summed for a total score. Research supports the criterion and concurrent validity of the BPFS (Chang, Sharp, & Ha, 2011; Haltigan & Vaillancourt, 2016). Further, the BPFS-C has been shown to be partially invariant over time through adolescence (Haltigan & Vaillancourt, 2016), making it appropriate for use in longitudinal studies. In the current sample, Cronbach’s alpha was .88, .88, .89, and .91 in years 2–5, respectively.
2.2.2. Witnessing of IPV between parents/caregivers
In the first year of the study, adolescents responded to two items adapted from the Family of Origin Violence Questionnaire to measure exposure to interparental violence (Holtzworth-Munroe, Meehan, Herron, Rehman, & Stuart, 2000). The questions were introduced as such: “No matter how well parents get along, there are times when they argue, and feel angry towards each other. The following questions deal with things that your father (or male caregiver) and mother (or female caregiver) might have done to each other when they were angry.” followed by a list of physical forms of violence (e.g., slapped, slammed against wall, choked). Next, adolescents were asked to respond to the question: “In your life, how many times did your father (or male caregiver) do any of these behaviors towards your mother (or female caregiver)?” The response scale was: “Never,” “Once or twice,” “3–20 times,” or “More than 20 times”. The question was then repeated for mother-to-father violence. Because of the low base rate of physical violence between parents (see Results section), these variables were combined and dichotomized for a new variable indicating the presence of any IPV (in any direction) such that 0 indicated no instances of violence and 1 indicated at least one instance of violence between parents. Cronbach’s alpha for endorsement of IPV from each parent was .72.
2.2.3. Parent (caregiver)-child relationship quality
During the first year of the study we assessed quality and closeness of mother and father relationships with four items: “Do you feel close to your mother (female caregiver),” “Do you feel close to your father (male caregiver),” “Do you share your thoughts and feelings with your mother (female careiver),” and “Do you share your thoughts and feelings with your father (male careiver). These items were adapted from the Attachment to Parents scale (Arthur, Hawkins, Pollard, Catalano, & Baglioni, 2002), which in its original form was too long for use in a large scale 5-year longitudinal community-based study where participant burden had to be taken into account. Students rated answers on a 4-point Likert scale ranging from “very true” to “very false”. Responses for the two items were averaged for an index of relationship quality with each parent, with higher values indicating poorer relationship quality. Internal consistency was evaluated by calculating Cronbach’s alpha for these two items for each parent separately, which was .81 for the relationship with mother and .88 for the relationship with father. These items have been shown to predict adolescent externalizing outcomes among similar samples from the community (Fagan, Lee Van Horn, Antaramian, & Hawkins, 2011; Hill, Howell, Hawkins, & Battin-Pearson, 1999).
2.3. Procedures
The current study was approved by the appropriate institutional review board, and occurred over five years, with assessments occurring annually. Study recruitment took place during school hours in classes with mandatory attendance. Research staff presented the study to students and answered any questions, and take-home packets with study information and parental consent forms were sent home. Students who returned with parental consent provided assent and completed assessments during school hours. Annual assessments while students were still in school also took place in classes with mandatory attendance. After leaving high school, assessments were completed via a web-based platform. Adolescents were compensated with $10 (years 1–3) and $20 (year 4–5) gift cards for participating. There was some attrition within the sample over time. Specifically, 15.5 % did not participate in year 2, 20.0 % did not participate in year 3, 29.8 % did not participate in year 4, and 36.8 % did not participate in year 5. Those who did not participate in years 2–4 did not differ from the rest of the sample in regard to gender (χ2(1)’s = .064–3.37, p’s = .499–.066) and participation in years 3–5 was not related to year 2 BPD features (B’s = −.005 – .001, p’s = .544–.977); however, those who did not participate in year 5 were more likely to be male (χ2(1) = 40.69, p < .001). Those who did not participate in years 2 and 5 did not differ from the rest of the sample in terms of IPV; however, those who experienced IPV at baseline, were less likely to participate in years 3–4 (χ2(1)’s = 4.63–5.32, p = .021–.031). Lastly, those who did not participate in years 2–5 tended to be older (t’s(1040) = 1.94–8.05, p’s = .000–.053). In sum, older adolescents consistently did not respond to follow-up surveys and males and those exposed to IPV did not participate in either one or two waves of data collection, respectively. Attrition is typical in community-based samples over 5 years and while data was not missing completely at random as suggested in the these analyses, the assumption of data missing at random (MAR) was reasonable and drove our choice of method to handle missing data as explained below.
2.4. Data analytic strategy
Prior to conducting main study analysis, descriptive and bivariate statistics were computed using SPSS version 25.0 (IBM Corp, 2017). We evaluated the distribution of BPD features and examined the frequency at which adolescents reported witnessing violence between their parents. We also computed bivariate correlations between main study variables (IPV exposure and borderline features) with various sociodemographic indicators (gender, age, ethnicity/race, family composition/living situation, mental health treatment history, and parent education) that are related to borderline features and IPV exposure based on previous literature to determine whether they should be included as covariates in further models. Finally, we estimated effect sizes of change in BPD features from year two to each of the subsequent time points using the standardized mean gain (ESsg), which accounts for inter-individual stability (Becker, 1988) and provides an indication of the magnitude of change in BPD features over the course of the study.
Next, latent growth curve modeling was used to estimate the course of change of BPD features from years two through five of the study using MPlus version 7.0 (Muthén & Muthén, 2006). Full Information Maximum Likelihood (FIML) estimation was used to account for missing data due to attrition, which is based on the assumption of data missing at random (MAR), which is the case when missingness is not random, but can be fully accounted for by variables with complete information. While it is impossible to statistically test the assumption of MAR, authors have stated that this is a reasonable assumption to make (Little & Rubin, 2002) and that FIML provides unbiased estimates in this case. FIML uses all available information to estimate population parameters that would be most likely, given the available sample data. Goodness of fit of models were evaluated using the root-mean-square error of approximation (RMSEA; Steiger, 1980) and its 90 % confident interval (CI), the Tucker-Lewis index (TLI; Tucker & Lewis, 1973), the comparative fit index (CFI; Bentler, 1990), and the standardized root-mean-square residual (SRMR; Jöreskog & Sörbom, 1996). Acceptable model fit was defined in part by criteria (Hu & Bentler, 1999): RMSEA values close to 0.06 or below (with the lower value of the 90 % CI no higher than 0.05 and the upper value no higher than 0.08), CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. First, unconditional growth models were constructed that evaluated the relation between initial status (level of borderline features at year 2) and change in borderline features from years 2 through 5. Slope factors were identified by fixing the loading of borderline features at year two to 0 with the rest of the loadings increasing at a linear rate (up to a loading of 3 at year 5), based on previous research demonstrating linear decreases of borderline features across this age range (e.g., Wright et al., 2016). The associations between intercept and slope factors were freely estimated to determine the association between initial level of borderline features and the rate of change across the study. The mean of the slope and intercept factors in these models reflect the total rate of change across the study and average level of borderline features at year two, respectively. The variance of the slope and intercept factors reflects level of individual differences in rate of change and initial levels of borderline features. Next, we regressed both the intercept and slope factors on to the variable representing exposure to IPV while controlling for the effects of child gender, minority status, family composition/living situation, mental health treatment history, parent education, and relationship quality with each parent (based on bivariate analyses described below).
3. Results
The majority (60.2 %; n = 627) of adolescents reported that they had not been exposed to any violence between parents. 23.7 % (n = 247) reported that they had observed violence between parents “once or twice”, 10.7 % (n = 111) reported observing violence “3–20 times”, and 4.8 % (n = 50) reported observing violence more than 20 times. An exact McNemar’s test determined that there was not a significant difference in the porption of maternal IPV witnessed and paternal IPV witnessed, p = .13. Scores representing quality of the relationship with mother and father ranged from 1 to 5, with an average of 2.10 (SD = 1.02) for the relationship with mother and 2.85 (SD = 1.26) with father.
Table 1 includes bivariate correlates between study variables. IPV exposure was greater among those in a non-traditional living situation (a blended family, living with non-parents, or in a single parent household), with current or previous mental health treatment, whose parents did not receive a college education, and with lower parental relationship quality. Borderline features (at various time points) were higher among females, those in a non-traditional living situation, those with current or previous mental health treatment, and with lower parental relationship quality. Additionally, we found that there were small, but significant relations between borderline features and Hispanic and African American ethnicity/race. Specifically, only at year 4, borderline features were higher for those reporting to be non-Hispanic and African American. Based on this information, the variables of child gender, minority status, family composition/living situation, mental health treatment history, parent education, and relationship quality with each parent were included as covariates in the main analyses.
Table 1.
Correlations of main study variables.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Male | ||||||||||||||||
| Age | .02 | |||||||||||||||
| Minority Status | −.07* | .04 | ||||||||||||||
| Hispanic/White | −.02 | −.01 | .45** | |||||||||||||
| White/Not Hispanic | .07* | −.04 | −1.00** | −.45** | ||||||||||||
| African American | −.07* | .10** | .41** | −.41** | −.41** | |||||||||||
| Living Situation | −.06 | .13** | .08* | −.13** | −.08* | .27** | ||||||||||
| Lifetime MHT | −.06 | .03 | −.14** | −.07* | .14** | −.05 | .13** | |||||||||
| College Edu-Parent | .05 | −.06 | −.13** | −.24** | .13** | .06 | −.13** | .01 | ||||||||
| Mother Rel. Quality | .03 | −.02 | −.03 | −.03 | .03 | −.03 | .09** | .056 | −.03 | |||||||
| Father Rel. Quality | −.21** | .05 | .10** | .04 | −.10** | .09** | .34** | .08** | −.15** | .25** | ||||||
| Exposure to any IPV | −.04 | .05 | .02 | .06 | −.02 | −.02 | .12** | .15** | −.16** | .18** | .17** | |||||
| IPV Exposure - Severity | −.06 | .05 | .04 | .06 | −.04 | −.02 | .09** | .14** | −.16** | .14** | .13** | .91** | ||||
| BPD - Year 2 | −.17** | −.04 | .01 | −.05 | −.01 | .04 | .12** | .17** | −.03 | .15** | .21** | .22** | .23** | |||
| BPD - Year 3 | −.17** | −.01 | −.03 | −.05 | .03 | .02 | .13** | .13** | −.01 | .14** | .18** | .18** | .16** | .65** | ||
| BPD - Year 4 | −.14** | −.02 | .04 | −.08* | −.04 | .11** | .10** | .11** | −.04 | .14** | .17** | .14** | .12** | .58** | .65** | |
| BPD - Year 5 | −.07 | −.07 | −.02 | −.06 | .02 | −.00 | .06 | .10* | −.02 | .07 | .04 | .09* | .07 | .45** | .52** | .60** |
Note.
p<.05,
p<.01;
Living situation refers to the child living in a non-traditional family composition (values of 0 indicate that the child lives with both biological parents and values of 1 indicate a blended family or living with non-parents or in a single parent household); Lifetime MHT indicates if the child is currently or in their past has received mental health treatment; College Edu-Parent indicates if at least 1 parent graduated from college; Exposure to any IPV is a dichotomous variable indicating exposure to any interparental violence; IPV Exposure – Severity is a categorical variable indicating severity of exposure (0 = no exposure, 1 = 1 or 2 incidents of violence, 2 = 3 or more incidents of violence); BPD variables are total scores of BPFS-C in years 2–5 of the current study; All other variables are measured at baseline.
Table 2 includes descriptive statistics for the sample including the number of participants completing measures, % female, rate of IPV exposure, and borderline features as well as effect size for cumulative change in borderline features. Based on values of skew and kurtosis, distributions of scores of borderline features at each wave were approximately normal. The mean level of borderline features at Year 2 (57.62) was well below the clinical cut-off score of 65 which has been identified for this measure, consistent with the nature of the community sample in the current study. Yet, from years 2 through 5, between 31 to 27.5 % of the sample reported levels of borderline features above clinical cut-off on this scale. There was a slight downward trend of borderline features across each year with small effect sizes. Despite attrition, the overall proportion of IPV exposure remained stable across years. Additionally, between years 2–4, the gender proportion remains somewhat stable, although in the last year, the proportion of females increased.
Table 2.
Estimates of means and standard deviations of borderline features.
| n | % female | % IPV | Mean-BPD | SD-BPD | ESsg | 95 % CI | P | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Year 2 | 963 | 56.0% | 38.3 % | 57.62 | 14.34 | |||
| Year 3 | 890 | 55.6% | 38.0 % | 56.07 | 13.95 | −.10 | −.15: −.04 | .065 |
| Year 4 | 764 | 57.9% | 36.8 % | 55.76 | 13.99 | −.15 | −.10: −.02 | < .001 |
| Year 5 | 679 | 62.9% | 38.6 % | 54.30 | 15.46 | −.20 | −.26: −.13 | < .001 |
Note: ESsg refers to cumulative change (change from Year 2 of the study). %IPV is based on the exposure to IPV varaible measured at baseline with the percentage based on the total number of participants for each respective wave.
Model fit of the unconditional latent growth curve for reports of borderline features was excellent (χ2(5) = 4.91, p = .427; RMSEA=.000, 90 % CI: .000, .044; CFI=1.00; TLI=1.00; SRMR=.029). Mean level of slope for borderline features was −0.93 (SE = .19, p < .001; standardized estimate = −.29), mirroring the observed mean levels, which showed a decline in borderline features over the course of the study. There was a moderate negative association between intercept and slope of borderline features (r=−.39; p < .001) suggesting that adolescents with higher initial levels of borderline features had slower declines in borderline features over the course of the study.
The conditional growth model of borderline features also fit well to the data (χ2(21) = 16.09, p = .765; RMSEA=.000, 90 % CI: .000, .019; CFI=1.000; TLI=1.007; SRMR=.014). Parameters are listed in Table 3 and the estimate of R2 indicated that 18 % of variance in intercept and 9% of variance in slope were explained by the current predictor set.
Table 3.
Conditional latent growth curve model parameters.
| Parameter | B (SE) | 95 % CI | β | p |
|---|---|---|---|---|
|
| ||||
| Intercept-mean | 48.97 (1.61) | 45.82, 52.12 | 4.07 | < .001 |
| Slope-mean | 0.85 (0.69) | −0.50, 2.20 | 0.27 | .219 |
| Intercept-variance | 119.37 (8.82) | 102.07, 136.66 | 0.83 | < .001 |
| Slope-variance | 9.07 (1.84) | 5.46, 12.68 | 0.91 | < .001 |
| Intercept with Slope | −10.09 (3.33) | −16.61, −3.57 | −0.31 | .002 |
| Intercept on | ||||
| Child gender | −3.82 (.89) | −5.56, −2.09 | −0.16 | < .001 |
| Minority status | −0.12 (.93) | −1.95, 1.71 | −0.01 | .897 |
| Living situation | 1.44 (.91) | −0.34, 3.22 | 0.06 | .113 |
| Lifetime MHT | 4.38 (1.09 | 2.24, 6.52 | 0.15 | < .001 |
| Parent education | 0.76 (.95) | −1.11, 2.63 | 0.03 | .425 |
| QoR-Mother | 1.20 (.44) | 0.34, 2.06 | 0.10 | .006 |
| QoR-Father | 1.41 (.39) | 0.64, 2.17 | 0.15 | < .001 |
| IPV | 4.68 (.91) | 2.91, 6.46 | 0.19 | < .001 |
| Slope on | ||||
| Child gender | 0.43 (.38) | −0.32, 1.19 | 0.07 | .257 |
| Minority status | −0.08 (.40) | −0.87, 0.71 | −0.01 | .849 |
| Living situation | 0.10 (.39) | −0.67, 0.87 | 0.02 | .793 |
| Lifetime MHT | −0.67 (.47) | −1.59, 0.26 | −0.09 | .156 |
| Parent Education | −0.31 (.40) | −1.10, 0.47 | −0.05 | .435 |
| QoR-Mother | −0.05 (.19) | −0.43, 0.33 | −0.02 | .788 |
| QoR-Father | −0.42 (.17) | −0.76, −0.09 | −0.17 | .013 |
| IPV | −1.08 (.39) | −1.84, −0.31 | −0.17 | .006 |
Exposure to IPV had a significant and positive effect (coeff = 4.68, SE = 0.91, p < .001) on intercept and a negative effect (coeff = −1.08, SE = 0.39, p = .006) on slope, such that those who with IPV exposure had higher baseline levels of borderline features and slower decreases in features over time. Additionally, females, those with mental health treatment (currently or in the past), and lower relationship quality with both parents had higher baseline levels of borderline features. Those with poorer relationship quality with fathers, only, demonstrated slower decreases in borderline features over time. Once accounting for these predictors, as well as the intercept of borderline features, there was no longer a significant decline in borderline features across the course of the study (as evidenced by a nonsignificant slope parameter: coeff = 0.85, SE = 0.69, p = .219); however, there remained significant residual variance of both intercept (coeff = 119.37, SE = 8.82, p < .001) and slope factors (coeff = 9.07, SE = 1.84, p < .001), suggesting that other, unmeasured predictors (apart from exposure to IPV) may also associated with a slower normative decline in borderline features. These are discussed in the Discussion. Fig. 1 presents an illustration of this model: on the top half of the figure is a graph with individually linear-fitted curves for 15 randomly selected individuals, which demonstrate the hetereogeneity in the sample in terms of change of borderline features. The bottom half of the figure demonstrates the estimated means for those with and without IPV exposure, with a clear linear decrease for those who did not experience IPV compared to a relatively flat line for those who experienced any incidence of IPV.
Fig. 1.
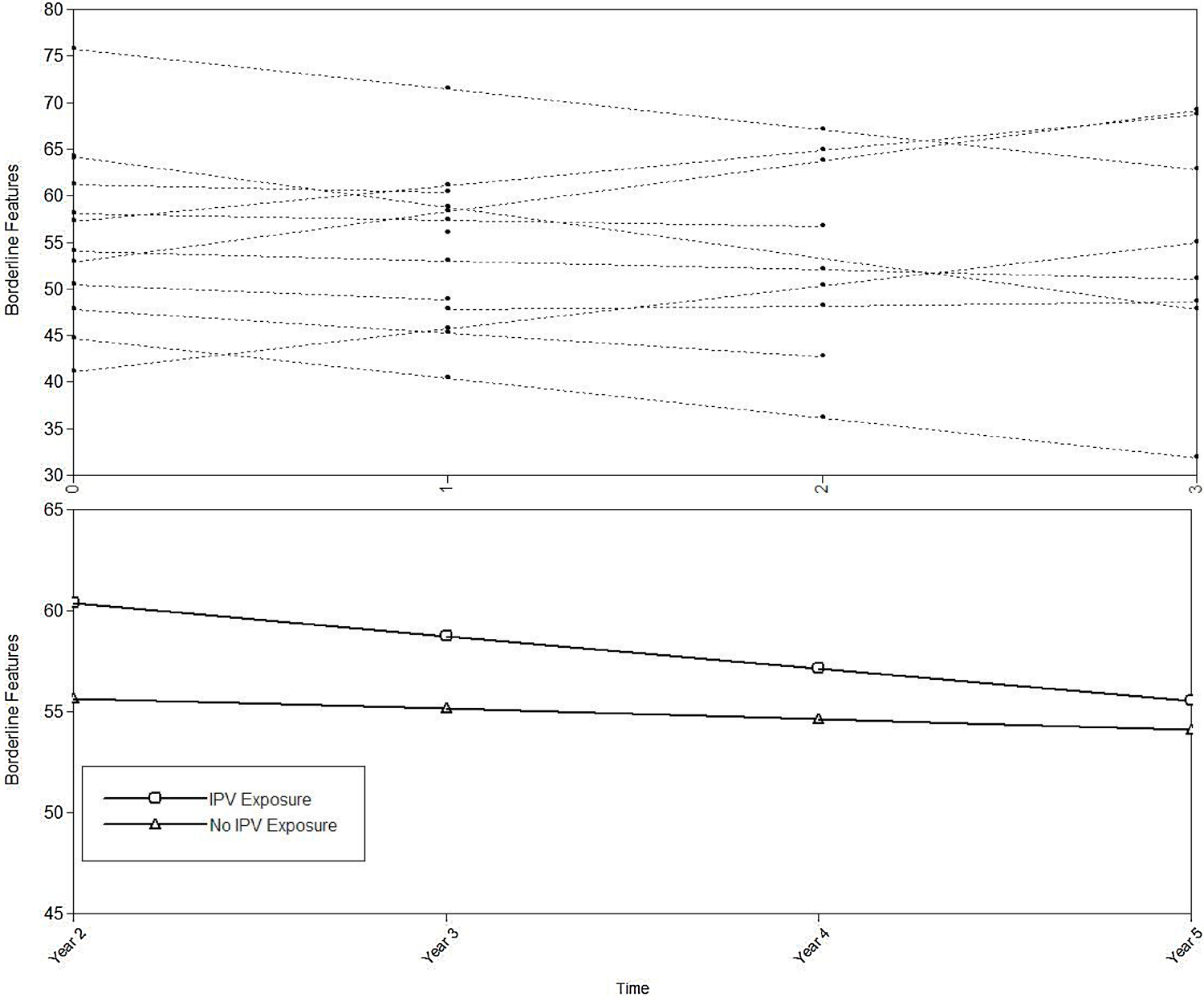
Individually fitted curves and estimated means for those with and without IPV exposure.
We conducted supplementary analyses based on suggestions made by reviewers to test whether severity of IPV exposure would have an effect on change in borderline features. For this model, we examined the subset of individuals (n = 408) who experienced IPV exposure and created a dichotomous variable of severity of IPV exposure (mild = 1–2 incidents of exposure or severe = 3+ incidents of exposure) as predictors of intercept and slope of borderline features. This model evidenced excellent fit to the data (χ2(21) = 23.99, p = .294; RMSEA=.019, 90 % CI: .000, .047; CFI=.992; TLI=.986; SRMR=.021). However, severity of IPV exposure did not significantly predict either intercept (coeff = 1.42, SE = 1.44, p = .325) or slope (coeff = 0.56, SE = 0.63, p = .374) of borderline features. These findings suggest that mere exposure to IPV is sufficient to predict change in the course of borderline features across late adolescence.
4. Discussion
Consistent with developmental models of BPD, which highlight the important role of early family environment, findings demonstrated that IPV related to both the intercept (cross-sectional association between interparental IPV and adolescents’ BPD) and the slope (change in borderline features over a 4-year period) parameters in our longitudinal model. Put simply, adolescents who had witnessed interparental/intercaregiver IPV were more likely to have higher levels of BPD features at baseline, and they were also more likely to deviate from the typically observed normative decline in BPD features over the 5-year follow-up period. The general downward trend in BPD features evidenced in the current study mirrors trends of BPD features observed in the years following mid-adolescence among other community samples (Bornovalova et al., 2009), but it is also clear that IPV may constitute one factor that can derail an adolescent from this normative decline. In sum, the current study adds to the empirical literature on interparental IPV and psychological problems among children and adolescents by documenting links between childhood exposure to interparental IPV and BPD features among adolescents.
The current findings also have implications for understanding the etiology of IPV among adults. Early experiences of child maltreatment, including the witnessing of interparental IPV, put individuals at risk for perpetrating IPV as adults (see Jouriles, Wolfe, Garrido, & McCarthy, 2006, for a review). It has been suggested that BPD features mediate the link between child maltreatment and IPV perpetration in adulthood (Hughes, Stuart, Gordon, & Moore, 2007; Jackson, Sippel, Mota, Whalen, & Schumacher, 2015), but this hypothesiss has not yet been tested with longitudinal data. However, prior longitudinal research indicates that BPD features predict later perpetration of IPV (Ehrensaft, Cohen, & Johnson, 2006), and the current research shows that childhood exposure to IPV relates to BPD features among adolescents. When considered together, the findings are consistent with the hypothesis that BPD features mediate the relation between childhood experiences of witnessing interparental IPV and the perpetration of IPV in adulthood.
As has been previously shown in community-based studies of adolescents (e.g. Crick et al., 2005), our study also showed a relation between female gender and higher levels of BPD features at baseline. However, this finding is likely the result of gender bias in diagnostic criteria for BPD - that is, criteria may assume unfairly that stereotypical female characteristics (e.g., emotionality) are pathological (Sharp et al., 2014). In addition, and consistent with developmental models of BPD, lower relationship quality with a caregiver, in this case the father, also predicted intercept and slope in the development of BPD features. Specifically, those who reported a higher relationship quality with their fathers had a faster decline of BPD features across the course of the study. The role of fathers has recently begun to receive more attention in the context of BPD, although there is still relatively little research on this topic. If we take into account that most IPV is perpertrated by men (Black et al., 2013), the fact that relationship quality with fathers appeared to either protect or put youngsters at risk for BPD seems to point to the importance of further considering the role of fathers not only in the development of BPD but in the effects of IPV on offspring more generally. In sum., these results add to a growing body of literature supporting the protective nature of paternal attachment security both against the development of BPD features (Kim, Sharp, & Carbone, 2014) and the negative impact of IPV, and in the development of positive emotion regulation strategies for adolescents with BPD (Fletcher, Parker, Bayes, Paterson, & McClure, 2014).
Our findings should be interpreted in the context of several limitations. First, although our findings suggest a temporal association between childhood exposure to interparental IPV and BPD features among adolescents, the findings are correlational, and variables not included in this study might help explain the findings. Variables that may be considered in future research include parental substance use, parental mental health, and other forms of child maltreatment. With regard to the latter, Ibrahim, Cosgrave, and Woolgar (2018) recently reviewed 10 studies of maltreatment related to BPD and showed that physical maltreatment and neglect by parents were in most cases related to BPD (emotional and sexual abuse related to BPD only in some studies). That our study demonstrated a link between physical abuse between parents and BPD in adolescents adds to a view that physical abuse in particular may be an important predictor of BPD in general. Second, our measurement of interparntal IPV was sub-optimal. Because of the relatively low frequency of exposure to interparental IPV we had to dichotomize the variable which gives the same weight to witnessing one instance of minor physical IPV as being exposed to multiple instances of minor to severe physical IPV. A more sophisticated assessment of IPV exposure that includes frequency, severity, timing of exposure, and type of IPV would yield richer data that might enable a more differentiated picture of different pathways and predictors of BPD. Moreover, exposure to IPV and quality of parental relationships were measured only at baseline which does not account for change over time and issues related to chronicity. Follow-up of all relevant variables would strengthen any future work in this regard. Findings regarding relationship quality with parents and IPV should also be interpreted against the background of the limitation that questions about relationship quality included mother and father, while questions about exposure to IPV included any caregiver. Concerns here are somewhat mitigated by the fact that we did not propose any interactional models that assumed that these questions covered the same caregivers. Other limitations in the current study include the fact that BPD is highly comorbid with other psychopathology (Cohen, 2008; Ha et al., 2014; Speranza et al., 2011), which was not controlled for in the current study. For instance, studies have shown that borderline symptoms are highly comorbid with symptoms of depression and anxiety, as well as trauma symptoms (Ha et al., 2014). While there is value in controlling for other psychopathology in order to increase specificity in defining unique trajectories for the development of BPD, doing so also creates an artificial and potentially non-generalizable picture of the development of BPD. In other words, important variance in the construct of BPD is lost if comorbidity is taken into account. Related to this limitation is the fact that we used a variable-centered approach to our analyses. Variable-centered approaches assume that all individuals from a sample are drawn from a single population for which a single set of “averaged” parameters can be estimated. In contrast, person-centered approaches consider the possibility that the sample might include multiple subpopulations characterized by different sets of parameters (Morin, Gagne, & Bujacz, 2016). While the former is most parsimonious, the latter has improved specificity. Neither approach is better or worse, but can provide complementary information about a problem and in this regard, future work in this area may benefit from taken a latent class approach to data of this sort. Another limitation that should be considered in interpreting our findings is that over-reliabnce on self-report, which may have inflated correlations.. An additional limitation relates to the fact that our study focused solely on physical IPV between caregivers, despite the fact that many forms of IPV have been defined. Future studies should include assessment of emotional and sexual IPV and verbal abuse between caregivers as these behaviors are as likely to contribute to the development of borderline features as physical IPV. A further limitation relates to attrition. While common for longitudinal studies in community samples, attrition does present the possibility for bias of parameter estimates. The value of conducting a longitudinal survey is that while certain individuals may fail to provide data for certain time points (as we found with males and those exposed to IPV), they resumed participation for later waves. However, we did find that older adolescents were consistently less likely to not complete follow-up surveys. We would expect our parameters to be biased if older adolescents didn’t complete the follow-up surveys because of their level of borderline pathology. While this assumption cannot be directly tested, it does temper the generalization of findings to older adolescents. Finally, our study neglected a thorough evaluation of exposure to same-sex/same-gender IPV which is an important emerging area in interparental IPV (e.g. McRae, Daire, Abel, & Lambie, 2017) and should be considered in the design of future studies. In sum, converging findings across different methods of measuring both childhood exposure to interparental IPV and BPD features among adolescents would provide stronger evidence for the documented links.
Despite these limitations, by demonstrating a predictive role for exposure to merely one instance of interparental IPV on the development of BPD features in adolescents, this longitudinal study is a novel contribution to the literature. Given that BPD appears to be more stable than internalizing and externalizing problems over time (see Sharp & Wall, 2018 for a review), and considering the very poor long-term outcomes documented for BPD (Gunderson et al., 2011; Skodol et al., 2002), it is important to identify variables that can be addressed with an eye on the prevention of BPD. The current findings suggest that exposure to interparental IPV may be one such variable. If replicated, our findings have implications for both developmental models of the pathogenesis of BPD, as well as for clinical practice. Regarding the former, developmental models of BPD fully acknowledge that the family environment may contribute to the development of BPD. However, the mechanisms by which this occur are usually framed solely in terms of the dyadic interaction and relations between caregiver and child. Here, we posit that exposure to physical violence should be considered an additional mechanism by which the family environment contributes to the development of BPD. An obvious pathway in this regard is through social learning and modeling. However, we also suggest that violence between parents is associated with (perhaps unintended) disregard for a child or adolescent’s perspective. Elsewhere, we have referred to the capacity to treat the child as a psychological agent with feelings, needs, perspectives and desires as parental mentalizing (Sharp & Fonagy, 2008; Sharp et al., n.d.). Parents who are deeply occupied and entangled in an emotionally or physically violent relationship will struggle to mentalize their child. Lack of parental mentalizing, in turn, have been suggested to be a critical factor in the development of BPD (Fonagy & Luyten, 2009).
Regarding clinical implications, the effects of interparental IPV on children can be targeted through a variety of parent-focused IPV programs (see Anderson & Van Ee, 2018; Austin, Shanahan, Barrios, & Macy, 2019 for reviews). These programs typically build resilence in children against the effects of IPVand they have shown good evidence of effectiveness. While untested, and following the argument above, an increase in mentalizing capacity in parents may be critical in protecting young people from developing BPD in particular. An alternative strategy to preventing BPD in young people is by addressing IPV between parents and caregivers more directly, which, in turn, should reduce any potential negative outcomes in children and adolescents, including BPD.
Funding
This study was made possible with funding by the Hogg Foundation for Mental Health (JRG-082) and the John Sealy Memorial Endowment Fund for Biomedical Research.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D.C: American Psychiatric Association. [Google Scholar]
- Anderson K, & Van Ee E (2018). Mothers and children exposed to intimate partner violence: A review of treatment interventions. International Journal of Environmental Research and Public Health, 15(9), 1955. 10.3390/ijerph15091955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur MW, Hawkins JD, Pollard JA, Catalano RF, & Baglioni AJ (2002). Measuring risk and protective factors for use, delinquency, and other adolescent problem behaviors: The communities that care youth survey. Evaluation Review, 26(6), 575–601. 10.1177/0193841X0202600601. [DOI] [PubMed] [Google Scholar]
- Austin AE, Shanahan ME, Barrios YV, & Macy RJ (2019). A systematic review of interventions for women parenting in the context of intimate partner violence. Trauma, Violence & Abuse, 20(4), 498–519. 10.1177/1524838017719233. [DOI] [PubMed] [Google Scholar]
- Becker BJ (1988). Synthesizing standardized mean-change measures. The British Journal of Mathematical and Statistical Psychology, 41(2), 257–278. 10.1111/j.2044-8317.1988.tb00901.x. [DOI] [Google Scholar]
- Bender DS, & Skodol AE (2007). Borderline personality as a self-other representational disturbance. Journal of Personality Disorders, 21(5), 500–517. 10.1521/pedi.2007.21.5.500. [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Biskin RS, Paris J, Renaud J, Raz A, & Zelkowitz P (2011). Outcomes in women diagnosed with borderline personality disorder in adolescence. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 20(3), 168–174. [PMC free article] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, … Stevens MR (2013). The national intimate partner and sexual violence survey (NISVS): 2010 summary report Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, & McGue M (2009). Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology, 21(4), 1335–1353. 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Johnson B, Bartle S, Bridge J, Rather C, Matta J, … Constantine D (1993). Personality disorder, tendency to impulsive violence, and suicidal behavior in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 32(1), 69–75. 10.1097/00004583-199301000-00010. [DOI] [PubMed] [Google Scholar]
- Chanen A (2015). Borderline personality disorder in young people: Are we there yet?: Borderline personality disorder. Journal of Clinical Psychology, 71(8), 778–791. 10.1002/jclp.22205. [DOI] [PubMed] [Google Scholar]
- Chanen A, Sharp C, Hoffman P, & Global Alliance for Prevention and Early Intervention for Borderline Personality Disorder (2017). Prevention and early intervention for borderline personality disorder: A novel public health priority. World Psychiatry, 16(2), 215–216. 10.1002/wps.20429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang B, Sharp C, & Ha C (2011). The criterion validity of the borderline personality features scale for children in an adolescent inpatient setting. Journal of Personality Disorders, 25(4), 492–503. 10.1521/pedi.2011.25.4.492. [DOI] [PubMed] [Google Scholar]
- Cohen P (2008). Child development and personality disorder. The Psychiatric Clinics of North America, 31(3), 477–493. 10.1016/j.psc.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Cohen P, Chen H, Gordon K, Johnson J, Brook J, & Kasen S (2008). Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Development and Psychopathology, 20(2), 10.1017/S095457940800031X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crick NR, Murray–Close D, & Woods K (2005). Borderline personality features in childhood: A short-term longitudinal study. Development and Psychopathology, null(04), 1051–1070. 10.1017/S0954579405050492. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan MM (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crumley FE (1979). Adolescent suicide attempts. JAMA, 241(22), 2404–2407. 10.1001/jama.1979.03290480038021. [DOI] [PubMed] [Google Scholar]
- De Clercq B, Verbeke L, De Caluwé E, Vercruysse T, & Hofmans J (2017). Understanding adolescent personality pathology from growth trajectories of childhood oddity. Development and Psychopathology, 29(4), 1403–1411. 10.1017/S0954579417000347. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, & Johnson JG (2006). Development of personality disorder symptoms and the risk for partner violence. Journal of Abnormal Psychology, 115(3), 474–483. 10.1037/0021-843X.115.3.474. [DOI] [PubMed] [Google Scholar]
- Evans SE, Davies C, & DiLillo D (2008). Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior, 13(2), 131–140. 10.1016/j.avb.2008.02.005. [DOI] [Google Scholar]
- Fagan AA, Lee Van Horn M, Antaramian S, & Hawkins JD (2011). How do families matter? Age and gender differences in family influences on delinquency and drug use. Youth Violence and Juvenile Justice, 9(2), 150–170. 10.1177/1541204010377748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher K, Parker G, Bayes A, Paterson A, & McClure G (2014). Emotion regulation strategies in bipolar II disorder and borderline personality disorder: Differences and relationships with perceived parental style. Journal of Affective Disorders, 157, 52–59. 10.1016/j.jad.2014.01.001. [DOI] [PubMed] [Google Scholar]
- Fonagy P, & Bateman A (2008). The development of borderline personality disorder—A mentalizing model. Journal of Personality Disorders, 22(1), 4–21. 10.1521/pedi.2008.22.1.4. [DOI] [PubMed] [Google Scholar]
- Fonagy P, & Luyten P (2009). A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Development and Psychopathology, 21(4), 1355–1381. 10.1017/S0954579409990198. [DOI] [PubMed] [Google Scholar]
- Fruzzetti AE, Shenk C, & Hoffman PD (2005). Family interaction and the development of borderline personality disorder: A transactional model. Development and Psychopathology, 17(4), 1007–1030. 10.1017/S0954579405050479. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, & Janson S (2009). Burden and consequences of child maltreatment in high-income countries. Lancet, 373(9657), 68–81. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann SA, Lynch S, Banyard V, DeVoe ER, & Halabu H (2007). Community-based intervention for children exposed to intimate partner violence: An efficacy trial. Journal of Consulting and Clinical Psychology, 75(2), 199–209. 10.1037/0022-006X.75.2.199. [DOI] [PubMed] [Google Scholar]
- Gunderson H, Skodol T, & Zanarini (2018). Borderline personality disorder. Nature Reviews, 24(4), 10829. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, … Skodol AE (2011). Ten-year course of borderline personality disorder: Psychopathology and function from the collaborative longitudinal personality disorders study. Archives of General Psychiatry, 68(8), 827–837. 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha C, Balderas JC, Zanarini MC, Oldham J, & Sharp C (2014). Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. The Journal of Clinical Psychiatry, 75(5), e457–464. 10.4088/JCP.13m08696. [DOI] [PubMed] [Google Scholar]
- Haltigan JD, & Vaillancourt T (2016). The Borderline Personality Features Scale for Children (BPFS-C): Factor structure and measurement invariance across time and sex in a community-based sample. Journal of Psychopathology and Behavioral Assessment, 38(4), 600–614. 10.1007/s10862-016-9550-1. [DOI] [Google Scholar]
- Hamby S, Finkelhor D, Turner H, & Ormrod R (2011). Children’s exposure to intimate partner violence and other family violence. Washington, DC: U.S. Department of Justice; 10.1037/e725322011-001. [DOI] [Google Scholar]
- Haselschwerdt ML, Hlavaty K, Carlson C, Schneider M, Maddox L, & Skipper M (2019). Heterogeneity within domestic violence exposure: Young adults’ retrospective experiences. Journal of Interpersonal Violence, 34(7), 1512–1538. 10.1177/0886260516651625. [DOI] [PubMed] [Google Scholar]
- Hill KG, Howell JC, Hawkins JD, & Battin-Pearson SR (1999). Childhood risk factors for adolescent gang membership: Results from the seattle social development project. The Journal of Research in Crime and Delinquency, 36(3), 300–322. [Google Scholar]
- Holtzworth-Munroe A, Meehan J, Herron K, Rehman U, & Stuart G (2000). Testing the Holtzworth-Munroe and Stuart (1994) batterer typology. Journal of consulting and clinical psychology, 68(6), 1000–1019. 10.1037/0022-006X.68.6.1000. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hughes FM, Stuart GL, Gordon KC, & Moore TM (2007). Predicting the use of aggressive conflict tactics in a sample of women arrested for domestic violence. Journal of Social and Personal Relationships, 24(2), 155–176. 10.1177/0265407507075406. [DOI] [Google Scholar]
- IBM Corp (2017). IBM SPSS statistics for windows (Version 25.0). Armonk, NY: IBM Corp. [Google Scholar]
- Ibrahim J, Cosgrave N, & Woolgar M (2018). Childhood maltreatment and its link to borderline personality disorder features in children: A systematic review approach. Clinical Child Psychology and Psychiatry, 23(1), 57–76. 10.1177/1359104517712778. [DOI] [PubMed] [Google Scholar]
- Jackson MA, Sippel LM, Mota N, Whalen D, & Schumacher JA (2015). Borderline personality disorder and related constructs as risk factors for intimate partner violence perpetration. Aggression and Violent Behavior, 24, 95–106. 10.1016/j.avb.2015.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MP (1995). Patriarchal terrorism and common couple violence: Two forms of violence against women. Journal of Marriage and the Family, 57, 283–294. [Google Scholar]
- Jöreskog KG, & Sörbom D (1996). LISREL 8: User’s reference guide. Retrieved fromhttps://books.google.com/books?hl=en&lr=&id=9AC-s50RjacC&oi=fnd&pg=PR1&dq=joreskog+sorbom+1996&ots=lV4BzWr72K&sig=5_tYjO1HnzLY6846Ayaz576fUqY.
- Jouriles EN, & McDonald R (2015). Intimate partner violence, coercive control, and child adjustment problems. Journal of Interpersonal Violence, 30(3), 459–474. 10.1177/0886260514535099. [DOI] [PubMed] [Google Scholar]
- Jouriles EN, Wolfe DA, Garrido E, & McCarthy A (2006). Relationship violence. Behavioral and emotional disorders in adolescents: Nature, assessment, and treatment. Guilford Press621–641. [Google Scholar]
- Kaess M, Brunner R, & Chanen A (2014). Borderline personality disorder in adolescence. Pediatrics, 134(4), 782–793. 10.1542/peds.2013-3677. [DOI] [PubMed] [Google Scholar]
- Kim S, Sharp C, & Carbone C (2014). The protective role of attachment security for adolescent borderline personality disorder features via enhanced positive emotion regulation strategies. Personality Disorders Theory Research and Treatment, 5(2), 125–136. 10.1037/per0000038. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Gaylord NK, Holt AR, & Kenny ED (2003). Child witnesses to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology, 71(2), 339–352. 10.1037/0022-006X.71.2.339. [DOI] [PubMed] [Google Scholar]
- Little R, & Rubin D (2002). Statistical analysis with missing data. New York: John Wiley & Sons. [Google Scholar]
- McFarlane J, Symes L, Binder B, Maddoux J, & Paulson R (2014). Maternal-child dyads of functioning: The intergenerational impact of violence against women on children. Maternal and Child Health Journal, 18(4), 2236–2243. [DOI] [PubMed] [Google Scholar]
- McRae L, Daire AP, Abel EM, & Lambie GW (2017). A social learning perspective on childhood trauma and same-sex intimate partner violence. Journal of Counseling & Development, 95(3), 332–338. [Google Scholar]
- Morin A, Gagne M, & Bujacz A (2016). Feature topic: Person-centered methodologies in the organizational sciences. Organizational Research Methods, 19(1), 8–9. 10.1177/1094428115617592. [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2006). Mplus version 7 user’s guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Narayan A, Hagan M, Cohodes E, Rivera L, & Lieberman A (2019). Early childhood victimization and physical intimate partner violence during pregnancy: A developmental and person-oriented approach. Journal of interpersonal violence, 31(1), 3–26. [DOI] [PubMed] [Google Scholar]
- Pompili M, Girardi P, Ruberto A, & Tatarelli R (2005). Suicide in borderline personality disorder: A meta-analysis. Nordic Journal of Psychiatry, 59(5), 319–324. 10.1080/08039480500320025. [DOI] [PubMed] [Google Scholar]
- Robertson K, & Murachver T (2011). Women and men’s use of coercive control in intimate partner violence. Violence and Victims, 26(2), 208–217. [DOI] [PubMed] [Google Scholar]
- Samuelson KW, Krueger CE, & Wilson C (2012). Relationships between maternal emotion regulation, parenting, and children’s executive functioning in families exposed to intimate partner violence. Journal of Interpersonal Violence, 27(17), 3532–3550. 10.1177/0886260512445385. [DOI] [PubMed] [Google Scholar]
- Sharp C, & Fonagy P (2008). The parent’s capacity to treat the child as a psychological agent: Constructs, measures and implications for developmental psychopathology. Social Development, 17(3), 737–754. 10.1111/j.1467-9507.2007.00457.x. [DOI] [Google Scholar]
- Sharp C, & Fonagy P (2015). Practitioner review: Borderline personality disorder in adolescence—recent conceptualization, intervention, and implications for clinical practice. Journal of Child Psychology and Psychiatry, 56(12), 1266–1288. 10.1111/jcpp.12449. [DOI] [PubMed] [Google Scholar]
- Sharp C, & Romero C (2007). Borderline personality disorder: A comparison between children and adults. Bulletin of the Menninger Clinic, 71(2), 85–114. 10.1521/bumc.2007.71.2.85. [DOI] [PubMed] [Google Scholar]
- Sharp C, Shohet C, Givon D, Penner F, Marais L, & Fonagy P (n.d.). Learning to mentalize: A mediational approach for caregivers and therapists. Clinical Psychology Science and Practice (in press). [Google Scholar]
- Sharp C, & Wall K (2018). Personality pathology grows up: Adolescence as a sensitive period. Current Opinion in Psychology, 21, 111–116. 10.1016/j.copsyc.2017.11.010. [DOI] [PubMed] [Google Scholar]
- Sharp C, Michonski JD, Steinberg L, Fowler JC, Frueh BC, & Oldham JM (2014). An investigation of differential item functioning across gender of BPD criteria. Journal of Abnormal Psychology, 123(1), 231–236. 10.1037/a0035637. [DOI] [PubMed] [Google Scholar]
- Sharp C, Wright AGC, Fowler JC, Frueh BC, Allen JG, Oldham J, ... Clark LA (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 124(2), 387–398. 10.1037/abn0000033. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, & Siever LJ (2002). The borderline diagnosis I: Psychopathology, comorbidity, and personaltity structure. Biological Psychiatry, 51(12), 936–950. 10.1016/S0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- Speranza M, Revah-Levy A, Cortese S, Falissard B, Pham-Scottez A, & Corcos M (2011). ADHD in adolescents with borderline personality disorder. BMC Psychiatry, 11(1), 10.1186/1471-244X-11-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH (1980). Tests for comparing elements of a correlation matrix. Psychological Bulletin, 87(2), 245–251. 10.1037/0033-2909.87.2.245. [DOI] [Google Scholar]
- Temple JR, Shorey RC, Tortolero SR, Wolfe DA, & Stuart GL (2013). Importance of gender and attitudes about violence in the relationship between exposure to interparental violence and the perpetration of teen dating violence. Child Abuse & Neglect, 37(5), 343–352. 10.1016/j.chiabu.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. 10.1007/BF02291170. [DOI] [Google Scholar]
- Turner BJ, Jin HM, Anestis MD, Dixon-Gordon KL, & Gratz KL (2018). Personality pathology and intentional self-harm: Cross-cutting insights from categorical and dimensional models. Current Opinion in Psychology, 21, 55–59. 10.1016/j.copsyc.2017.09.009. [DOI] [PubMed] [Google Scholar]
- Vu NL, Jouriles EN, McDonald R, & Rosenfield D (2016). Children’s exposure to intimate partner violence: A meta-analysis of longitudinal associations with child adjustment problems. Clinical Psychology Review, 46, 25–33. 10.1016/j.cpr.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Whitaker MP (2013). Centrality of control-seeking in men’s intimate partner violence perpetration. Prevention Science, 14(5), 513–523. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, & Chen H (2008). Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry, 49(9), 933–941. 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, & Jaffe PG (2003). The effects of children’s exposure to domestic violence: A meta-analysis and critique. Clinical Child and Family Psychology Review, 17. [DOI] [PubMed] [Google Scholar]
- Yen S, Gagnon K, & Spirito A (2013). Borderline personality disorder in suicidal adolescents. Personality and Mental Health, 7(2), 89–101. 10.1002/pmh.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]


