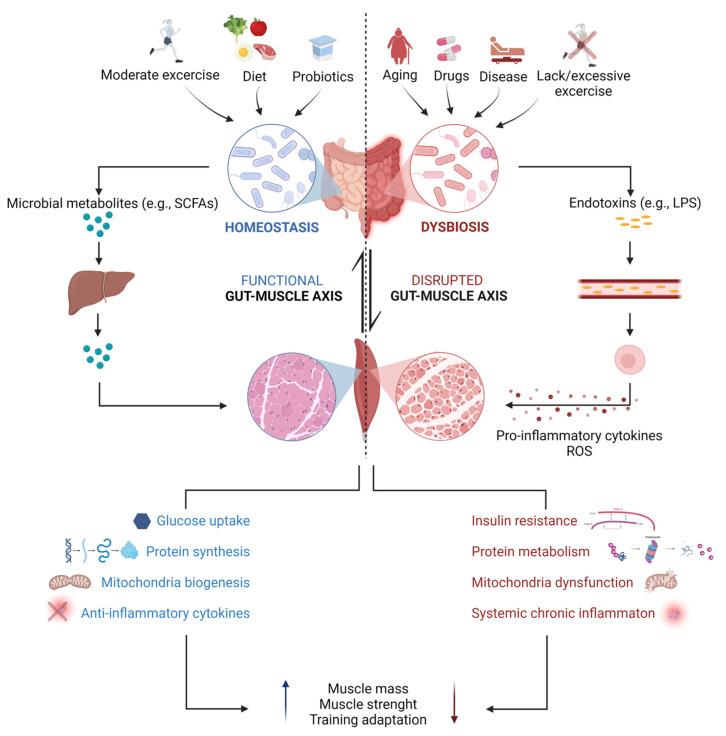
Figure 2.
Schematic diagram of gut microbiota-mediated regulation of skeletal muscle under physiological and pathological conditions. The shaping of the gut microbiota composition is driven by both genetic and environmental factors. Regular moderate physical activity, consumption of dietary fibers and supplementation with prebiotics/probiotics promote an increase in the relative abundance of potentially beneficial bacteria, involved in the production of metabolites, among which short chain fatty acids (SCFAs). Following absorption by intestinal cells, SCFAs (mostly propionate and acetate, while butyrate is mainly used as a source of energy for colonocytes) reach the liver, where most of the propionate serves as a substrate for hepatic gluconeogenesis, while part of the acetate is destined to undergo hepatic lipid synthesis. Eventually, just small amounts of SCFAs (primarily acetate) reach the systemic circulation and directly interact with skeletal muscles [77]. Thus, both direct and indirect mechanisms concur with SCFA-mediated regulation of skeletal muscle metabolism, including modulation of glucose and energy metabolism, protein balance, mitochondrial biogenesis and regulation of inflammation, overall improving skeletal muscle mass and function. On the contrary, dysbiosis, a state that can be caused by aging, insufficient/excessive physical activity, drug consumption or disease state, is associated with increased intestinal permeability and gut leaking, which facilitates the passage of endotoxins (e.g., lipopolysaccharide, LPS) and other microbial products (e.g., indoxyl sulfate) into the peripheral circulation, from where these molecules trigger the production of pro-inflammatory cytokines and reactive oxygen species (ROS) by macrophages and promote insulin resistance, muscle proteolysis, and mitochondrial dysfunction in skeletal muscles. This results in skeletal muscle changes that may manifest as decreases in muscle mass and function, ultimately affecting muscle physical performance. Created with Biorender.com.