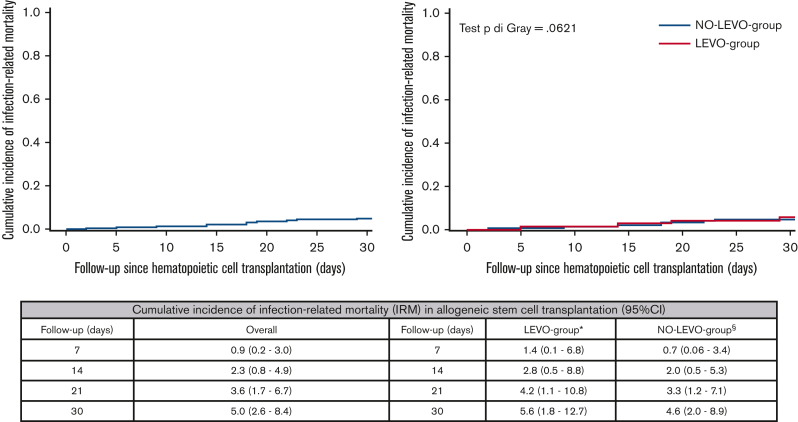
Figure 2.
Cumulative incidence of IRM at day +30 after transplant in the overall sample and according to prophylaxis use in allo-HSCT recipients. The cumulative incidence of IRM was estimated according to the Fine-Gray method, with relapse/progression, GVHD grade ≥2, and death from any other cause as competing events for IRM. In this analysis, the time to IRM was censored at the earliest of relapse/progression, GVHD grade ≥2, and death from any other cause, as appropriate. ∗Four patients died of IRM at day +30 after transplant: 2 CR-Kp carriers who experienced CR-Kp PE-BSI achieving BSI clearance with an appropriate empiric antibiotic therapy (cause of death: 1 pneumonia, 1 probable invasive aspergillosis and HHV6 encephalitis); 1 CR-Pa carrier who experienced CR-Pa PE-BSI with an inappropriate empiric antibiotic therapy (cause of death: CR-Pa septic shock and pneumonia); 1 patient who experienced vancomycin-susceptible E faecium PE-BSI developing systemic complications of sepsis (cause of death: cardiac decompensation, acute kidney injury, multiorgan failure). §Seven patients died of IRM at day +30 after transplant: 1 patient died of disseminated Scedosporium prolificans infection; 2 patients experienced P aeruginosa PE-BSI, 1 CR-Pa with inappropriate empiric antibiotic therapy (acquisition of CR-Pa rectal colonization after HSCT [cause of death: CR-Pa septic shock]) and 1 carbapenem-susceptible Pa with appropriate empiric antibiotic therapy achieving BSI clearance (cause of death: pneumonia, multiorgan failure); 1 patient experienced K pneumoniae likely amp-C producer PE-BSI with appropriate empiric antibiotic therapy achieving BSI clearance (cause of death: further PE-BSI sustained by S maltophilia with associated pneumonia); 2 patients experienced not ESBL-producing E coli PE-BSI with appropriate empiric antibiotic therapy achieving BSI clearance (cause of death: 1 septic shock and pneumonia, 1 bowel perforation); 1 patient died of septic shock and pneumonia without the occurrence of PE-BSI.