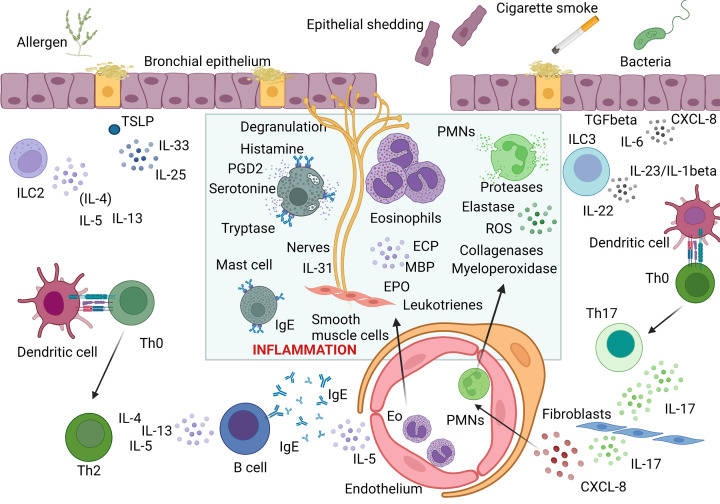
Figure 1. Cellular and cytokine interactions involved in allergic (Type 2) and non-allergic (non-Type 2) asthma.
Type 2 immune response is initiated when inhaled allergens trigger epithelial release of thymic stromal lymphopoietin (TSLP), IL-33 and IL-25 which induce type 2 responses via activation of type 2 innate lymphoid cells (ILC2), as well as activation and differentiation of Th2 cells. In this pathway, IL-4 and IL-13 regulate isotype switching in B cells to IgE production while IL-5 regulates eosinophil recruitment and activation. Effector phase of Type 2 immune response is dependent on allergen crosslinking of specific IgE on mast cells and basophils leading to their degranulation and release of histamine, serotonin and other mediators and proinflammatory cytokines. Furthermore, activated eosinophils recruited to the site of allergic inflammation release eosinophilic cationic protein (ECP), major basic protein (MBP) or eosinophilic peroxidase. The mixture of inflammatory mediators and cytokines including IL-4, IL-13, and IL-31 directly affect epithelial cells and induce their shedding, stimulate mucus overproduction, oedema, and bronchoconstriction. In non-type 2 immune response, environmental stimuli including cigarette smoke and microbes lead to a release of neutrophilic chemokine CXCL8, either directly from epithelial cells or fibroblasts via ILC3-mediated IL-17 pathway controlled by epithelial IL-6 and TGF beta. Recruited activated neutrophils release reactive oxygen species (ROS), myeloperoxidase, proteases, elastases and collagenases leading to epithelial cell damage and mucus hyperproduction. Created with BioRender Sofware (Ref.n.WV25BY7AMN).