Abstract
Objective:
Long-term care (LTC) homes (“nursing homes”) were challenged during the first year of the COVID-19 pandemic in Canada. The objective of this study was to measure the impact of the COVID-19 pandemic on resident admission and discharge rates, resident health attributes, treatments, and quality of care.
Design:
Synthesis analysis of “Quick Stats” standardized data table reports published yearly by the Canadian Institute for Health Information. These reports are a pan-Canadian scorecard of LTC services rendered, resident health characteristics, and quality indicator performance.
Setting and participants:
LTC home residents in Alberta, British Columbia, Manitoba, and Ontario, Canada that were assessed with the interRAI Minimum Data Set 2.0 comprehensive health assessment in fiscal years 2018/2019, 2019/2020 (pre-pandemic period), and 2020/2021 (pandemic period).
Methods:
Risk ratio statistics were calculated to compare admission and discharge rates, validated interRAI clinical summary scale scores, medication, therapy and treatment provision, and seventeen risk-adjusted quality indicator rates from the pandemic period relative to prior fiscal years.
Results:
Risk of dying in the LTC home was greater in all provinces (risk ratio [RR] range 1.06-1.18) during the pandemic. Quality of care worsened substantially on 6 of 17 quality indicators in British Columbia and Ontario, and 2 quality indicators in Manitoba and Alberta. The only quality indicator where performance worsened during the pandemic in all provinces was the percentage of residents that received antipsychotic medications without a diagnosis of psychosis (RR range 1.01-1.09)
Conclusions and implications:
The COVID-19 pandemic has unveiled numerous areas to strengthen LTC and ensure that resident’s physical, social, and psychological needs are addressed during public health emergencies. Except an increase in potentially inappropriate antipsychotic use, this provincial-level analysis indicates that most aspects of resident care were maintained during the first year of the COVID-19 pandemic.
Keywords: Long-term care, quality of care, COVID-19, clinical characteristics
Introduction
In Canada, long-term care (LTC) homes provide 24-hour facility-based nursing and personal support services to individuals with continuing care needs. LTC home residents were disproportionately affected during the initial waves of the COVID-19 pandemic in Canada. As of July 2021, 11 652 deaths among LTC home residents were recorded, accounting for more than 40% of all COVID-19 deaths across the country. Mortality rates have varied geographically and temporally, where risk of mortality was substantially greater in large provinces like Quebec and Ontario during the first 6 months of the pandemic. Provinces like Manitoba that were relatively unaffected in the first wave led the country in the second wave. 1 LTC home residents and staff were given priority access to vaccines in the winter of 2020/2021, 2 and with initial uptake exceeding 90% of residents and staff in several provinces, mortality rates fell dramatically across the country. 3
An abundance of media reports suggested that large numbers of LTC home residents experienced dire living conditions, poor quality of care, social isolation, and decline in health and well-being during the first year of the pandemic.4,5 In response to some of the more severe outbreaks, military support was provided to 5 LTC homes in Ontario. 6 The report from that deployment described many residents as having died from starvation and dehydration. 7 Further, more than half of the Ontario LTC home staff that responded to an online survey perceived that quality of care for residents with dementia had worsened during the pandemic. 8 Although there is no doubt that severe COVID-19 outbreaks negatively affected quality of care and resident health in some LTC homes, the impact of the pandemic on residents across the broader Canadian LTC sector has not yet been studied using objective quality measures.
Each year, the Canadian Institute for Health information (CIHI) publishes a standardized data table report in the public domain that describes services rendered, resident health characteristics, and quality indicator performance statistics for the LTC sector in Canada. 9 These “‘Quick Stats’ Profile of Residents in Residential and Hospital-Based Continuing Care” reports represent all LTC home residents in Canada that were assessed with the interRAI Minimum Data Set (MDS) 2.0 health assessments.10-12 Thus, they serve as a near pan-Canadian scorecard for LTC services in Canada and are the ideal way of measuring changes in resident clinical profile and quality of care that may have occurred during the pandemic.
This study synthesized 3 consecutive years of “Quick Stats” reports to measure changes to LTC home resident admission and discharges, resident health, treatments, and quality of care during the first year of the COVID-19 pandemic in Canada. By identifying the aspects of resident health and quality of care that were most severely affected during the pandemic, this study supports the development of targeted policy interventions to safeguard residents during future public health crises.
Methods
Study design
This study was a synthesis analysis of statistical reports produced by CIHI as part of its “‘Quick Stats’ Profile of Residents in Residential and Hospital-Based Continuing Care” repository from 2018/2019 to 2020/2021. Our analysis focused on Alberta, British Columbia, Manitoba, and Ontario because the incidence of COVID-19 among LTC home residents was greatest in these provinces during the initial waves of the pandemic. 1
Data sources
“Quick Stats” reports are based on data from CIHI’s Continuing Care Reporting System (CCRS). The information that is reported to CCRS is collected using the interRAI Minimum Data Set (MDS) 2.0 assessment. 10 This standardized comprehensive clinical health assessment is administered by trained assessors on a quarterly basis to persons residing in LTC homes for a period of 14 days or longer. It is used to assess numerous domains of health and well-being including functional and cognitive performance, mood and behavior, pain and other health conditions, and health service utilization. 10 “Quick Stats” reports are based on MDS 2.0 assessments pertaining to a given fiscal year, beginning April 1st and ending March 31st. When multiple MDS 2.0 assessments for a single resident are available during this accrual period, only the last assessment is used.
interRAI coding standards are employed in “Quick Stats” for the specification of all summary scales and algorithms used to report diverse aspects of health system performance, including clinical characteristics of residents, resource utilization, and risk adjusted quality of care. Information from the interRAI assessments is used for several purposes, including resident care planning,12-14 case-mix based funding, 15 and system performance monitoring using risk-adjusted quality indicators.16,17 These data are routinely used for system-level research and policy development,11,18-21 and have become 1 of the most important data sources for studying resident-level attributes associated with COVID-19 mortality among Canadians.22-24 The reliability and the validity of the assessment items and summary scales has been reported extensively in previous studies.25-29
Exposure: Pre-pandemic and pandemic periods
The earliest reported COVID-19 outbreak in Canada was on March 5th, 2020, 30 thus statistics reported for fiscal year 2020/2021 (most recent available) best represent care provided during the pandemic period. Prior fiscal years represent the pre-pandemic period.
Measures of interest
We compared several statistics reported in the “Quick Stats” data tables, including resident volumes, admission and discharge rates, discharge disposition, clinical summary scale scores (described in Supplemental Table 1), medication, therapy and treatment provision, and risk-adjusted quality indicator rates.
interRAI risk-adjusted quality indicators combine indirect standardization using outcome-associated covariates and stratification with direction standardization to allow fair comparison between entities—in this case pandemic and pre-pandemic periods—despite resident case-mix differences. 17 Each risk-adjusted quality indicator uses a different set of exclusion criteria, and some quality indicators require two consecutive assessments to measure resident-level change over time. 17 Seventeen quality indicators related to function (e.g., changes in independence in ADLs), safety (e.g., falls), and quality of life (e.g., changes in mood) are reported in the “Quick Stats” report. We focused on the nine quality indicators that are currently publicly reported on CIHI’s “Your Health System” national public reporting website. 31 The remaining quality indicators are presented as Supplemental Figures.
Statistical analysis
We compared resident volumes, admissions and discharges, and clinical summary scales, therapy and treatment provision, and risk-adjusted quality indicator rates by computing risk ratio (RR) statistics comparing fiscal years 2018/2019 and 2019/2020 (pre-pandemic periods) with 2020/2021 (pandemic period). Since year-to-year variance is expected, we focused on differences that were significantly different relative to both pre-pandemic years.
We computed admission and discharge rates as a percentage of all residents that received care during the fiscal year. Discharge disposition rates (e.g., death in facility, discharge to hospital) were also computed as a percentage of all residents that received care during the fiscal year. All other risk ratio comparisons were for measures collected using the MDS 2.0 assessment, thus the total number of assessed residents was used as the denominator.
All analyses were performed using R (version 4.1.0), primarily using the epitools package (version 0.5-10.1).
Results
Resident volume, admissions, and discharges
The total number of residents that received care in LTC homes during the pandemic period was lower in all provinces. The difference was largest in Ontario where the volume of residents decreased by 18%. This was primarily due to an unusually large decrease in the number of admissions during the pandemic period. Relative to before the pandemic, new admissions also accounted for a lower percentage of all residents that received care during the pandemic period in the other provinces—but nowhere near the magnitude seen for Ontario. Admissions from hospital increased twofold in Ontario during the pandemic year. They were also elevated in British Columbia and Manitoba (Figure 1).
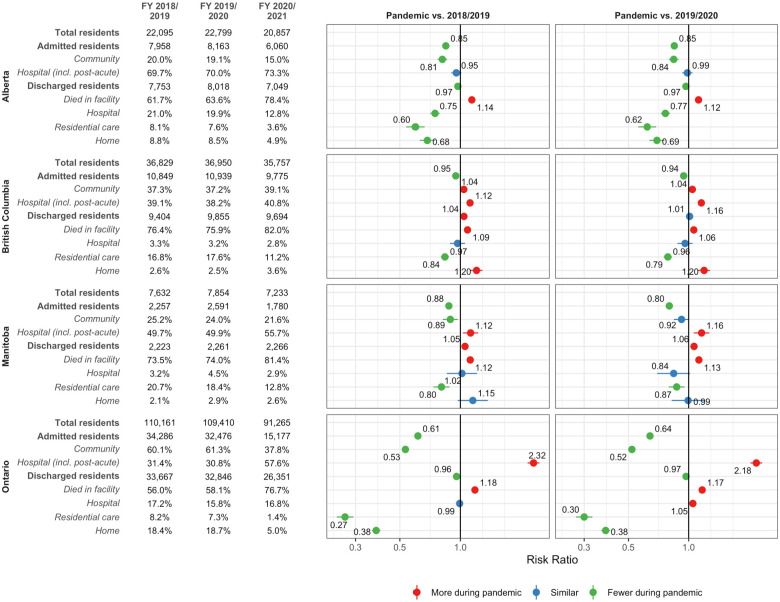
Figure 1.
Resident volumes, admission and discharge rates, and discharge destination during the COVID-19 pandemic relative to pre-pandemic periods.
Risk of discharge was greater in Manitoba (RR range 1.05-1.06) during the pandemic period, but slightly lower in Alberta (RR 0.97) and Ontario (RR range 0.96-0.97). Risk of death in the LTC homes was greater in all provinces during the pandemic. It was greatest in Ontario (RR range 1.17-1.18) and lowest in British Columbia (RR range 1.06-1.09). Risk of discharge to hospital during the pandemic period was lower in Alberta (RR range 0.60-0.62) and was similar to the pre-pandemic periods in the other provinces. Transfers to other residential care facilities were lower in all provinces during the pandemic period (Figure 1).
Resident health attributes
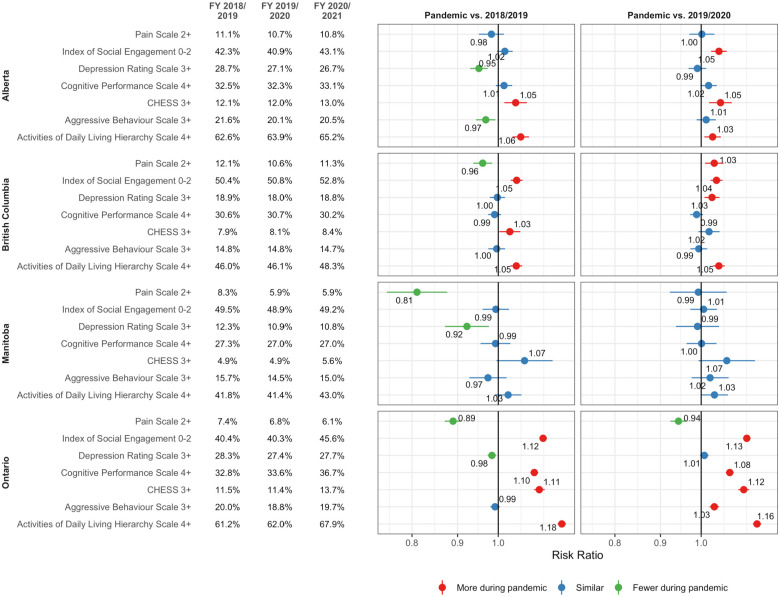
Figure 2 compares clinical scale scores by province during the pandemic period relative to the 2 previous years. In Alberta, there were small increases in the percentage of residents with at least extensive functional impairment (ADL-H 4+; RR range 1.03-1.06) and moderate or worse health instability (CHESS 3+; RR 1.05). In British Columbia, more residents experienced low social engagement (ISE 0-2; RR range 1.04-1.05) and extensive functional impairment (ADL-H 4+; RR 1.05). None of the differences in Manitoba were meaningful. In Ontario, there were greater negative shifts on several measures, including low social engagement (ISE 0-2; RR range 1.12-1.13), severe cognitive impairment (CPS 4+; RR range 1.08-1.10), moderate or worse health instability (CHESS 3+; RR range 1.11-1.12), and extensive functional impairment (ADL-H 4+; RR range 1.16-1.18). Fewer residents experienced daily pain (Pain scale 2+; RR range 0.89-0.94).
Figure 2.
Outcome scale scores during the COVID-19 pandemic relative to pre-pandemic periods.
Abbreviation: CHESS, Changes in Health, End-Stage Disease and Signs and Symptoms Scale.
Medications, therapies, and care programs
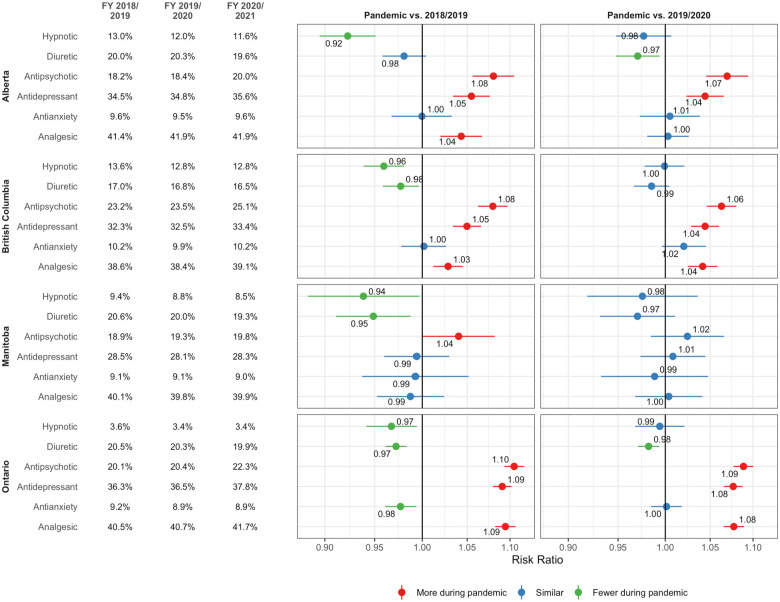
We observed an increase in antipsychotic (RR range 1.06-1.10) and antidepressant (RR range 1.04-1.09) use among residents during the pandemic period in Alberta, British Columbia, and Ontario. Analgesic use increased in British Columbia (RR range 1.03-1.04) and Ontario (RR range 1.08-1.09). Diuretic use decreased slightly in Ontario (RR range 0.97-0.98; Figure 3).
Figure 3.
Medication use during the COVID-19 pandemic relative to pre-pandemic periods.
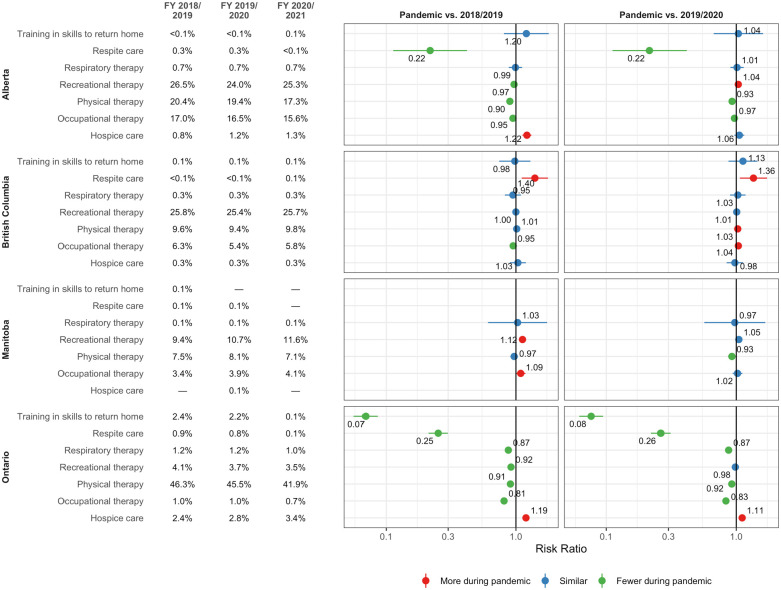
The percentage of residents that received physical therapy (RR range 0.90-0.93) and occupational therapy (RR range 0.81-0.97) decreased in Alberta and Ontario during the pandemic period. Although provided infrequently prior to the pandemic, we also observed a very large relative decrease in the provision of respite care (RR range 0.22-0.26) in these two provinces during the pandemic period. In the case of Ontario, almost no residents received training in skills to return to home during the pandemic period (RR range 0.07-0.08) (Figure 4).
Figure 4.
Therapies and treatments during the COVID-19 pandemic relative to pre-pandemic periods.
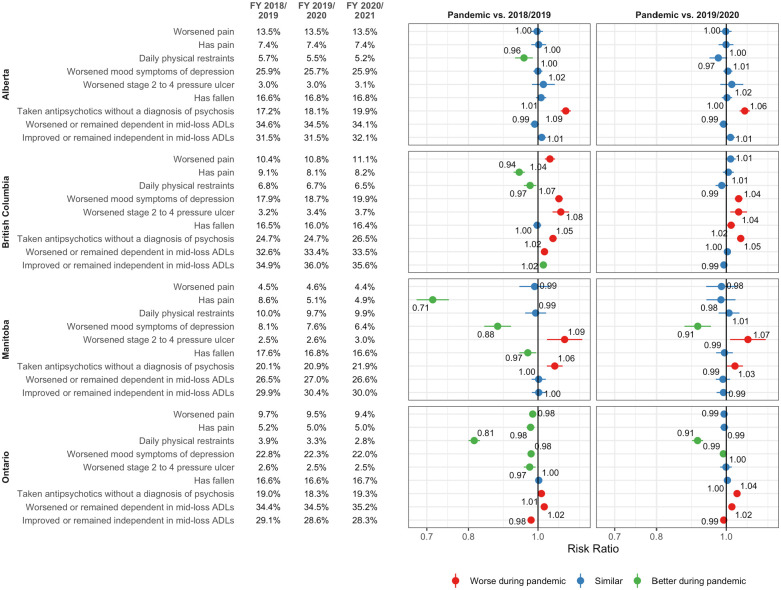
Quality indicator performance
Quality of care during the pandemic period was most severely affected in British Columbia and Ontario. Among all 17 quality indicators that are reported, worse performance was observed on 7 quality indicators in British Columbia and 6 quality indicators in Ontario. Quality of care worsened during the pandemic period on 2 indicators in Manitoba and Alberta. Improvement was observed on 4 quality indicators in Ontario, 2 quality indicators in British Columbia, and 1 quality indicator in Manitoba (Figure 5 and Supplemental Figures 1–4).
Figure 5.
Risk-adjusted quality indicator performance during the COVID-19 pandemic relative to pre-pandemic periods. Subset of quality indicators reported on Canadian Institute for Health Information’s “Your Health System” public reporting system. All quality indicators included in Supplemental Figures.
In all provinces there was an increase in the percentage of residents that received antipsychotic medications without a diagnosis of psychosis during the pandemic period. This increase was greatest in Alberta (RR range 1.06-1.09) and smallest in Ontario (RR range 1.01-1.04). The only other indicator that worsened in more than 1 province was the “worsened stage 2 to 4 pressure ulcer” indicator. Although the risk-adjusted rates for this indicator are low (range 2.5%-3.7% during pandemic), there were substantial relative increases in British Columbia (RR range 1.04-1.08) and Manitoba (RR range 1.07-1.09).
Two quality indicators improved in more than 1 province during the pandemic period. Fewer residents in Manitoba (RR range 0.88-0.91) and Ontario (RR range 0.98-0.99) experienced worsened mood symptoms of depression. Fewer residents experienced infections (excluding COVID-19) during the pandemic period in Ontario (RR range 0.93-0.99) and British Columbia (RR range 0.92-0.97).
Discussion
Our analysis is based on over half a million resident assessments in 4 Canadian provinces in the 2 years prior to and the first year of the COVID-19 pandemic. Despite high COVID-19 infection and mortality rates in Canadian LTC homes, we observed modest provincial-level changes in resident clinical characteristics and quality of care during the first year of the pandemic. Although COVID-19 was responsible for excess mortality among residents, 32 we postulate that large decreases in new admissions, particularly for convalescent and respite care, also explain some changes in measures of resident health. The areas in which pandemic exposure was associated with degraded quality of care were limited and inconsistent across provinces.
Off-label use of antipsychotic medications to address behavioral and psychological symptoms of dementia is a prevalent quality problem in LTC homes.16,33 As a result of national change initiatives in Canada, 16 rates of potentially inappropriate use decreased from 33.3% in 20112012 to 20.2% in 2019/2020. A significant increase in psychotropic medication prescribing, including antipsychotic medications, during the pandemic has previously been reported in LTC settings in Ontario,34,35 Michigan (United States), 36 the United Kingdom, 37 and Spain. 38 Our analysis indicates that increased psychotropic medication use also occurred in Alberta and British Columbia.
Degraded performance on CIHI’s risk-adjusted quality indicator in all provinces suggests that the increase in antipsychotic medication use was largely inappropriate in nature. When considered in the context of the progress that has been achieved over the past decade, this represents a step backwards for the LTC sector in Canada. Like in the United States, 36 we did not observe a significant increase in behavioral symptoms, which raises question about whether antipsychotic medications were provided preemptively, for example in anticipation of challenges related to outbreak management and staffing shortages. 39 CIHI’s publicly reported quality indicators should be used to monitor this issue at a facility-level and target LTC homes that would benefit from training and mentorship interventions focused on antipsychotic use within the context of the evolving LTC care environment. Previously successful interventions in Canada have focused on person-centered approaches to care, interdisciplinary collaboration, and use of routine medication review and deprescribing guidelines. 16
Our analysis is based on aggregated statistics and does not identify provincial-level factors, including staffing-related factors, that may be associated with a differential pandemic exposure impact on quality of care. Patterson et al 40 suggest that differences in LTC direct care staffing policies between Ontario and British Columbia might partially explain differences in COVID-19 response, and thus, differences in case and mortality rates between provinces. It is possible that pandemic period staffing difficulties are also related to Ontario's degraded performance on several quality indicators related to ADLs, particularly since direct care staff instability is associated with quality in this domain in United States nursing homes. 41 The challenge of ecological inferences of this type is reconciling other changes to quality of care that we observed. For example, despite their pandemic preparedness, 42 British Columbia was uniquely challenged in managing pressure ulcers and preventing worsening in mood symptoms of depression. Given that current evidence base suggests that the relationship between quality of care and staffing is mixed, 43 we believe that our findings are best used to guide future analysis using record-level CCRS data that are positioned to test this hypothesis directly.
Analysis of the initial waves of the pandemic indicates substantial variation in facility-level outbreak severity, with large outbreaks concentrated among a limited number of LTC homes.44-46 The denominators of the provincial-level quality indicators that we examined are large, ranging from nearly 20 000 residents in Manitoba to more than 200 000 residents in Ontario. Further, CIHI’s CCRS quality indicator methodology uses 4 consecutive fiscal quarters of MDS 2.0 assessment records, thereby buffering the impact of time-limited changes to quality of care during outbreaks periods. 47 Consequently, if changes to quality of care were predominantly among homes experiencing severe outbreaks, it is not surprising that differences were not detected in most of the broader provincial-level indicators that we examined. Conversely, this implies that the pandemic period differences in quality that we did observe likely to represent meaningful sector-wide changes that warrant careful monitoring. Future analyses should use record-level CCRS data to examine the pandemic impact on facility-level quality of care, particularly in proximity to outbreak periods among severely affected homes.
We observed an increase in the relative ratio of measures of clinical complexity (e.g., severe impairment in functional and cognitive abilities, high levels of health instability) during the pandemic period. We are unable to make inferences about resident-level increases in clinical complexity of existing residents using these cross-sectional data. However, given that changes to performance on quality indicators of longitudinal change were generally small, we expect that these differences are largely explained by fewer short-stay admissions during the pandemic period. This is because admissions for convalescence, respite, and interim care programs were suppressed, likely due to preference to avoid congregate care 4 and new resident isolation policies that would delay initiation of rehabilitation. 48 Residents that return to the community within 90 days of LTC admission are generally less impaired in physical and cognitive function49,50 and are excluded from CIHI national indicators of LTC appropriateness. 51 Health system administrators should be aware of this short-stay resident sample bias when comparing measures of resident complexity and resource intensity (e.g., case mix index) over time. 15
Limitations
Since we used standardized CIHI data tables, our analysis was limited to provincial-level measures of resident health status and quality of care. We expect that facility-level comparisons will identify LTC homes where the pandemic impact on resident health and quality of care was substantial, particularly among those that experienced severe outbreaks and critical staff shortages. “Quick Stats” data tables are produced as part of CIHI’s routine health system performance monitoring function and reflect MDS 2.0 assessments completed throughout the entire first year of the pandemic. Serial cross-sectional analysis using more granular time periods, which can be aligned with province-specific periods of heightened COVID-19 incidence (“waves”), would provide a better characterization of the pandemic impact on the LTC sector. We were also unable to examine resident sub-groups using these standardized data tables. Although we expect that fewer admissions among short-stay residents are responsible for most of the changes in resident health status that we observed, this question is best addressed through analysis of record-level data from CCRS.
Conclusions and Implications
Canada’s LTC sector experienced severe strain during the first year of the COVID-19 pandemic. While the pandemic has unveiled areas to be addressed in terms of infection practice and controls, emergency preparedness, and staffing supports, we should also recognize the system’s resilience. Except for the increased use of potentially inappropriate antipsychotic medications, our pan-Canadian synthesis analysis of CIHI data tables demonstrates that resident clinical complexity and quality of care are similar to pre-pandemic levels. Subsequent analyses should move beyond provincial-level comparisons to understand impact of COVID-19 outbreaks on facility-level changes in resident health and quality of care.
Supplemental Material
Supplemental material, sj-png-1-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-2-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-3-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-4-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study is supported by funding from the Canadian Institutes of Health Research (FRN—CIHR GA6-177780) and the Government of Canada’s New Frontiers in Research Fund (NFRFG-2020-00500) for collaboration in the EU Horizon 2020 research and innovation project Individualized CARE for Older Persons with Complex Chronic Conditions in Home Care and Nursing Homes (I-CARE4OLD, Grant Agreement No 965341).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Luke Andrew Turcotte  https://orcid.org/0000-0001-5678-7234
https://orcid.org/0000-0001-5678-7234
Supplemental material: Supplemental material for this article is available online.
References
- 1.Canadian Institute for Health Information. Impact of COVID-19 on Long-Term Care, March 2020 to June 2021 — Data Tables. Canadian Institute for Health Information; 2021. Accessed October 21, 2022. https://www.cihi.ca/sites/default/files/document/impact-covid-19-long-term-care-mar-2020-jun-2021-data-tables-en.xlsx [Google Scholar]
- 2.Brown KA, Stall NM, Vanniyasingam T, et al. Early Impact of Ontario’s COVID-19 Vaccine Rollout on Long-Term Care Home Residents and Health Care Workers. Ontario COVID-19 Science Advisory Table; 2021. [Google Scholar]
- 3.National Institute on Ageing. A Cautionary Tale: Canada’s Vaccine Rollout Among Older Adults. National Institute on Ageing; 2022. [Google Scholar]
- 4.Achou B, De Donder P, Glenzer F, Lee M, Leroux ML. Nursing home aversion post-pandemic: Implications for savings and long-term care policy. J Econ Behav Organ. 2022;201:1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller EA, Simpson E, Nadash P, Gusmano M. Thrust into the spotlight: COVID-19 focuses media attention on nursing homes. J Gerontol Ser B. 2021;76:e213-e218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Office of the Premier. Ontario taking action at high risk long-term care homes. news.ontario.ca. May 27, 2020. Accessed October 27, 2022. https://news.ontario.ca/en/release/57033/ontario-taking-action-at-high-risk-long-term-care-homes
- 7.Mialkowski C. Op LASER—JTFC observations in long-term care facilities in Ontario. 3350-Op LASER 20-01 (COS). Toronto (ON): Headquarters, 4th Canadian Division Joint Task Force (Central); 2020. Accessed October 21, 2022. https://www.macleans.ca/wp-content/uploads/2020/05/JTFC-Observations-in-LTCF-in-ON.pdf
- 8.Kirkham J, Shorey CL, Iaboni A, et al. Staff perceptions of the consequences of COVID-19 on quality of dementia care for residents in Ontario long-term care homes. Int J Geriat Psychiatry. 2022;37:gps.5725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canadian Institute for Health Information. Profile of Residents in Residential and Hospital-Based Continuing Care, 2020–2021. Canadian Institute for Health Information; 2020. [Google Scholar]
- 10.Bernabei R, Landi F, Onder G, Liperoti R, Gambassi G. Second and third generation assessment instruments: the birth of standardization in geriatric care. J Gerontol A Biol Sci Med Sci. 2008;63:308-313. [DOI] [PubMed] [Google Scholar]
- 11.Carpenter I, Hirdes JP. Using interRAI assessment systems to measure and maintain quality of long-term care. In: A Good Life in Old Age?. OECD Health Policy Studies. OECD Publishing; 2013:93-139. [Google Scholar]
- 12.Heckman GA, Gray Leonard C, Hirdes JP. Addressing Health Care Needs for Frail Seniors in Canada: The Role of interRAI Instruments. UWSpace. 2013. [Google Scholar]
- 13.Heckman GA, Hirdes JP, Hébert PC, et al. Predicting future health transitions among newly admitted nursing home residents with heart failure. J Am Med Dir Assoc. 2019;20:438-443. [DOI] [PubMed] [Google Scholar]
- 14.Hirdes JP, Mitchell L, Maxwell CJ, White N. Beyond the ‘iron lungs of gerontology’: using evidence to shape the future of nursing homes in Canada*. Can J Aging. 2011;30:371-390. [DOI] [PubMed] [Google Scholar]
- 15.Turcotte LA, Poss J, Fries B, Hirdes JP. An overview of international staff time measurement validation studies of the RUG-III case-mix system. Health Serv Insights. 2019;12:117863291982792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirdes JP, Major J, Didic S, et al. A Canadian cohort study to evaluate the outcomes associated with a multicenter initiative to reduce antipsychotic use in long-term care homes. J Am Med Dir Assoc. 2020;21:817-822. [DOI] [PubMed] [Google Scholar]
- 17.Jones RN, Hirdes JP, Poss JW, et al. Adjustment of nursing home quality indicators. BMC Health Serv Res. 2010;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fries BE, Morris JN, Bernabei R, Finne-Soveri H, Hirdes J, Consortium for the interRAI. Rethinking the resident assessment protocols. J Am Geriatr Soc. 2007;55:1139-1140. [DOI] [PubMed] [Google Scholar]
- 19.Hawes C, Phillips CD, Mor V, Fries BE, Morris JN. MDS data should be used for research. Gerontologist 1992;32:563-564. [DOI] [PubMed] [Google Scholar]
- 20.Mor V. Improving the quality of long-term care with better information. Milbank Q. 2005;83:333-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zimmerman DR, Karon SL, Arling G, et al. Development and testing of nursing home quality indicators. Health Care Financ Rev. 1995;16:107-127. [PMC free article] [PubMed] [Google Scholar]
- 22.Lee DS, Ma S, Chu A, et al. Predictors of mortality among long-term care residents with SARS-CoV-2 infection. J Am Geriatr Soc. 2021;69:3377-3388. [DOI] [PubMed] [Google Scholar]
- 23.McArthur C, Faller-Saunders A, Turcotte LA, et al. Examining the effect of the first wave of the COVID-19 pandemic on home care recipients’ instrumental activities of daily living capacity. J Am Med Dir Assoc. 2022;23:1609.e1-1609.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webber C, Myran DT, Milani C, et al. Cognitive decline in long-term care residents before and during the COVID-19 pandemic in Ontario, Canada. JAMA. 2022;328:1456-1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foebel AD, Hirdes JP, Heckman GA, Kergoat MJ, Patten S, Marrie R. Diagnostic data for neurological conditions in interRAI assessments in home care, nursing home and mental health care settings: a validity study. BMC Health Serv Res. 2013;13:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hirdes JP, Poss JW, Caldarelli H, et al. An evaluation of data quality in Canada’s Continuing Care Reporting System (CCRS): secondary analyses of Ontario data submitted between 1996 and 2011. BMC Medical Inform Decis Mak. 2013;13:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris JN, Nonemaker S, Murphy K, et al. A commitment to change: revision of HCFA’s RAI. J Am Geriatr Soc. 1997;45:1011-1016. [DOI] [PubMed] [Google Scholar]
- 28.Morris JN, Jones RN, Fries BE, Hirdes JP. Convergent validity of minimum data set-based performance quality indicators in postacute care settings. Am J Med Qual. 2004;19:242-247. [DOI] [PubMed] [Google Scholar]
- 29.Poss JW, Jutan NM, Hirdes JP, et al. A review of evidence on the reliability and validity of minimum data set data. Healthc Manage Forum. 2008;21:33-39. [DOI] [PubMed] [Google Scholar]
- 30.Hsu AT, Lane N, Sinha SK, et al. Understanding the Impact of COVID-19 on Residents of Canada’s Long-Term Care Homes – Ongoing Challenges and Policy Responses. International Long-Term Care Policy Network, CPEC-LSE; 2020:18. [Google Scholar]
- 31.Poldrugovac M, Amuah JE, Wei-Randall H, et al. Public Reporting of performance indicators in long-term care in Canada: does it make a difference? Can J Aging. 2022;41:565-576. [DOI] [PubMed] [Google Scholar]
- 32.Akhtar-Danesh N, Baumann A, Crea-Arsenio M, Antonipillai V. COVID-19 excess mortality among long-term care residents in Ontario, Canada. PLoS One. 2022;17:e0262807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rios S, Perlman CM, Costa A, Heckman G, Hirdes JP, Mitchell L. Antipsychotics and dementia in Canada: a retrospective cross-sectional study of four health sectors. BMC Geriatr. 2017;17:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campitelli MA, Bronskill SE, Maclagan LC, et al. Comparison of medication prescribing before and after the COVID-19 pandemic among nursing home residents in Ontario, Canada. JAMA Network Open. 2021;4:e2118441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stall NM, Zipursky JS, Rangrej J, et al. Assessment of psychotropic drug prescribing among nursing home residents in Ontario, Canada, during the COVID-19 pandemic. JAMA Intern Med. 2021;181:861-863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coe AB, Montoya A, Chang C, et al. Behavioral symptoms, depression symptoms, and medication use in Michigan nursing home residents with dementia during COVID -19. J Am Geriatr Soc. 2023;71:414-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McDermid J, Ballard C, Khan Z, et al. Impact of the Covid-19 pandemic on neuropsychiatric symptoms and antipsychotic prescribing for people with dementia in nursing home settings. Int J Geriatr Psychiatry. 2023;38:e5878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferro Uriguen A, Laso Lucas E, Sannino Menicucci C, et al. Psychotropic drug prescription in nursing homes during the COVID-19 pandemic. Drugs Aging. 2022;39:467-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ali MM, Oliveira I, Blanco M. Prescriptions of antipsychotics dispensed in long-term care facilities during the COVID-19 pandemic. Gen Hosp Psychiatry. 2022;78:141-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patterson PB, Weinberg T, McRae S, Pollack C, Dutton D. Long-term care staffing policies pre-COVID-19 and pandemic responses: a case comparison of Ontario and British Columbia. Can Public Policy. 2023;49:94-113. [Google Scholar]
- 41.Mukamel DB, Saliba D, Ladd H, Konetzka RT. Association of staffing instability with quality of nursing home care. JAMA Netw Open. 2023;6:e2250389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu M, Maxwell CJ, Armstrong P, et al. COVID-19 in long-term care homes in Ontario and British Columbia. CMAJ. 2020;192:E1540-E1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clemens S, Wodchis W, McGilton K, McGrail K, McMahon M. The relationship between quality and staffing in long-term care: a systematic review of the literature 2008–2020. Int J Nurs Stud. 2021;122:104036. [DOI] [PubMed] [Google Scholar]
- 44.Damiano N, Turcotte L. Factors Associated with COVID-19 Outbreaks, Transmission and Poor Outcomes in Ontario’s LTC Homes. Canadian Institute for Health Information; 2021. Accessed October 21, 2022.https://wayback.archive-it.org/17275/20210810150042/http://www.ltccommission-commissionsld.ca/presentations/index.html [Google Scholar]
- 45.Stall NM, Jones A, Brown KA, Rochon PA, Costa AP. For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. CMAJ. 2020;192:E946-E955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cox MB, McGregor MJ, Poss J, Harrington C. The association of facility ownership with COVID-19 outbreaks in long-term care homes in British Columbia, Canada: a retrospective cohort study. CMAJO. 2023;11:E267-E273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Canadian Institute for Health Information. CCRS Quality Indicators Risk Adjustment Methodology. Canadian Institute for Health Information; 2013. [Google Scholar]
- 48.Ontario Ministry of Health and Long Term Care. COVID-19 Directive #3 for Long-Term Care Homes under the Fixing Long-Term Care Act, 2021. 2020. [Google Scholar]
- 49.Fries BE, James ML. Beyond section Q: prioritizing nursing home residents for transition to the community. BMC Health Serv Res. 2012;12:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gassoumis ZD, Fike KT, Rahman AN, Enguidanos SM, Wilber KH. Who transitions to the community from nursing homes? Comparing patterns and predictors for short-stay and long-stay residents. Home Health Care Serv Q. 2013;32:75-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cho MZ, Frood J, Husak L, Lacroix J, Hall N, Turcotte LA. New data on access to mental health and addictions services and home and community care. Healthc Quart. 2021;23:9-11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-png-1-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-2-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-3-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights
Supplemental material, sj-png-4-his-10.1177_11786329231174745 for Long-Term Care Resident Health and Quality of Care During the COVID-19 Pandemic: A Synthesis Analysis of Canadian Institute for Health Information Data Tables by Luke Andrew Turcotte, Caitlin McArthur, Jeff W Poss, George Heckman, Lori Mitchell, John Morris, Andrea D Foebel and John P Hirdes in Health Services Insights