Figure 3. The anti-inflammatory functions of HDL.
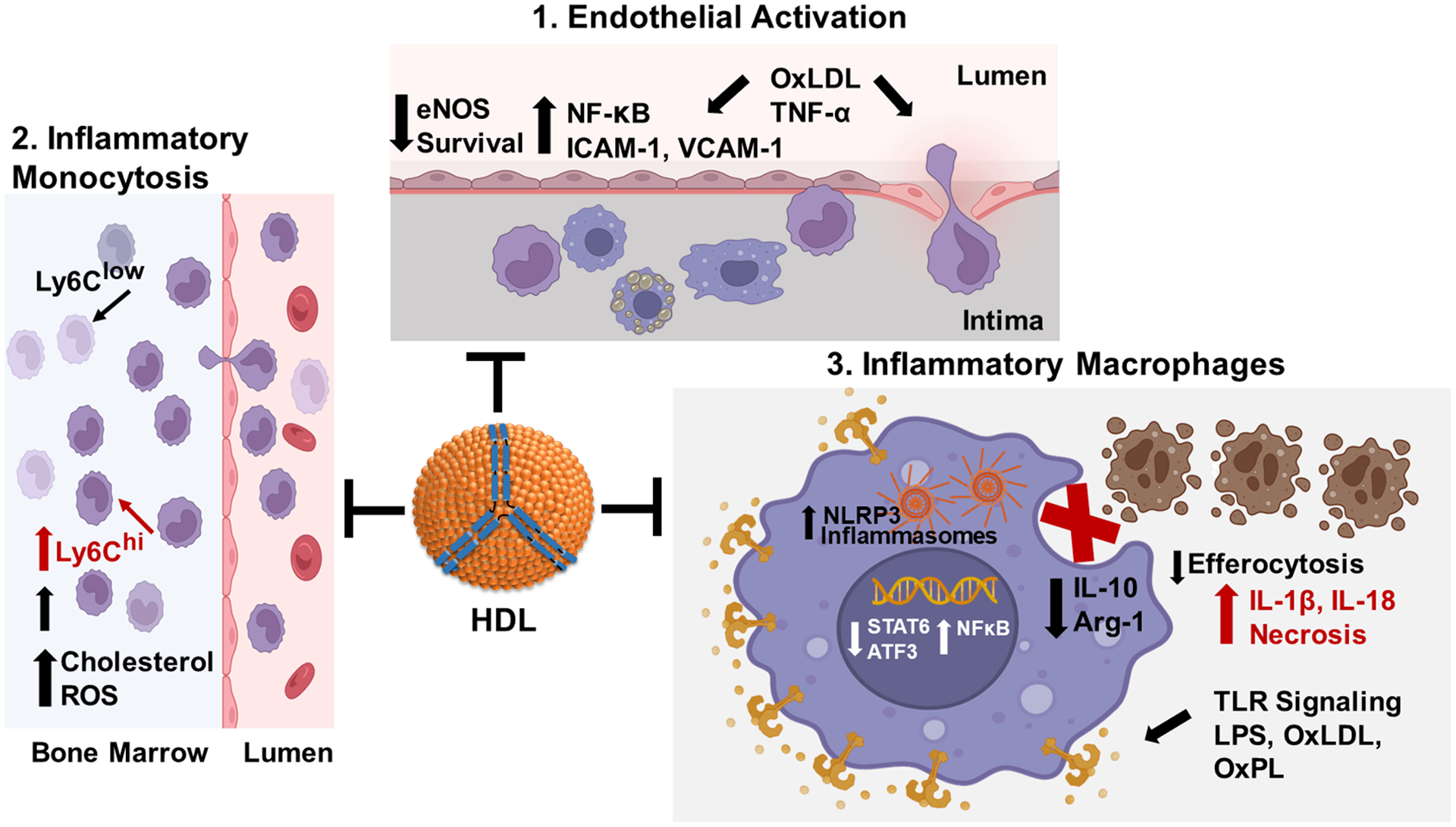
1. HDL suppresses endothelial activation in response to proinflammatory stimuli such as TNF-α and oxLDL. Proinflammatory stimuli activate NF‐κB (nuclear factor kappa B), which increases expression of monocyte adhesion proteins and chemotactic/inflammatory cytokines, thereby increasing monocyte recruitment and endothelial cell death. HDL signaling pathways stimulate nitric oxide production to decrease NF‐κB activation and maintain endothelial barrier integrity. 2. HDL prevents inflammatory monocytosis. Increased LDL and oxLDL, resulting from hypercholesterolemia, induce inflammatory signaling and ROS (reactive oxygen species) leading to expansion of bone marrow granulocyte monocyte progenitors that give rise to inflammatory Ly6Chigh monocytes. HDL signaling pathways suppress ROS production and inflammatory signaling and expansion of Ly6Chigh monocytes. 3. HDL prevents the macrophage proinflammatory phenotype. LPS, oxLDL, and other TLR (toll-like receptor) ligands activate NF‐κB leading to increased expression of inflammatory cytokines and NLRP3 (nucleotide oligomerization domain-like receptor protein with pyrin domain containing 3) inflammasome components resulting in decreased efferocytosis of apoptotic cells and necrotic death. HDL suppresses TLR signaling and NF‐κB activation via cholesterol efflux dependent and independent pathways to promote activation of Atf3 (activating transcription factor 3) and STAT6 (signal transducer and activator of transcription 6), thereby reducing activation of inflammasomes and enhancing efferocytosis of apoptotic cells by promoting expression of Arg-1 (arginase-1) and IL-10. Created with BioRender.com.
