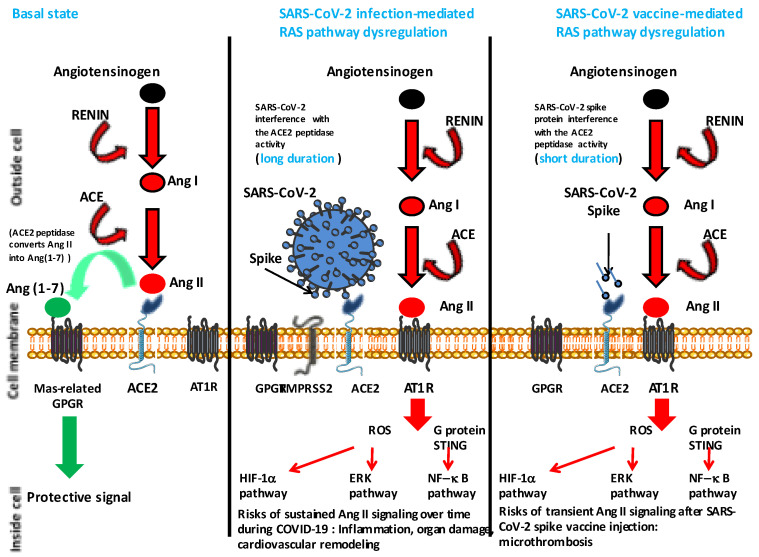
Figure 3.
Simplified diagram of the renin-angiotensin system (RAS) in normal conditions and under dysregulation mediated either by the SARS-CoV-2 or a SARS-CoV-2 spike based vaccine. The left panel simply indicates that ACE2 converts Ang II to Ang (1-7) leading to a protective signal (a balance between Ang I and Ang (1-7) is required for homeostasis). The middle panel illustrates the possible dysfunction of signals when SARS-CoV-2 is attached to its ACE2 receptor (this dysfunction has been experimentally and clinically proven). Under this condition the balance between Ang (1-7) and Ang II is in favor of Ang II. Ang II accumulates and binds to AT1R, leading to proinflammatory and hypoxia signals that can trigger tissue damage (in particular to the lung and heart). The right panel illustrates a hypothetical transient dysfunction of the RAS pathway when an excess of SARS-CoV-2 spike protein is present in tissues, as a consequence of recent vaccination, leading to a short period during which there is a risk of micro-thrombosis. The spike protein (vaccine) is likely to mimic the virus by interacting with the cellular ACE2; however in that case the process is expected to be of short duration in contrast to the process mediated by the virus that continues for as long as the virus replicates in a patient. Angiotensin I = Ang I; angiotensin II = Ang II; angiotensin (1-7) = Ang (1-7); angiotensin I converting enzyme = ACE; angiotensin I converting enzyme 2 = ACE2; angiotensin II type 1 receptor = AT1R; G protein-coupled receptor = GPGR; reactive oxygen species = ROS; hypoxia inducible factor 1 alpha = HIF-1α; extracellular signal regulated kinases = ERK; nuclear factor kappa B = NF-B.