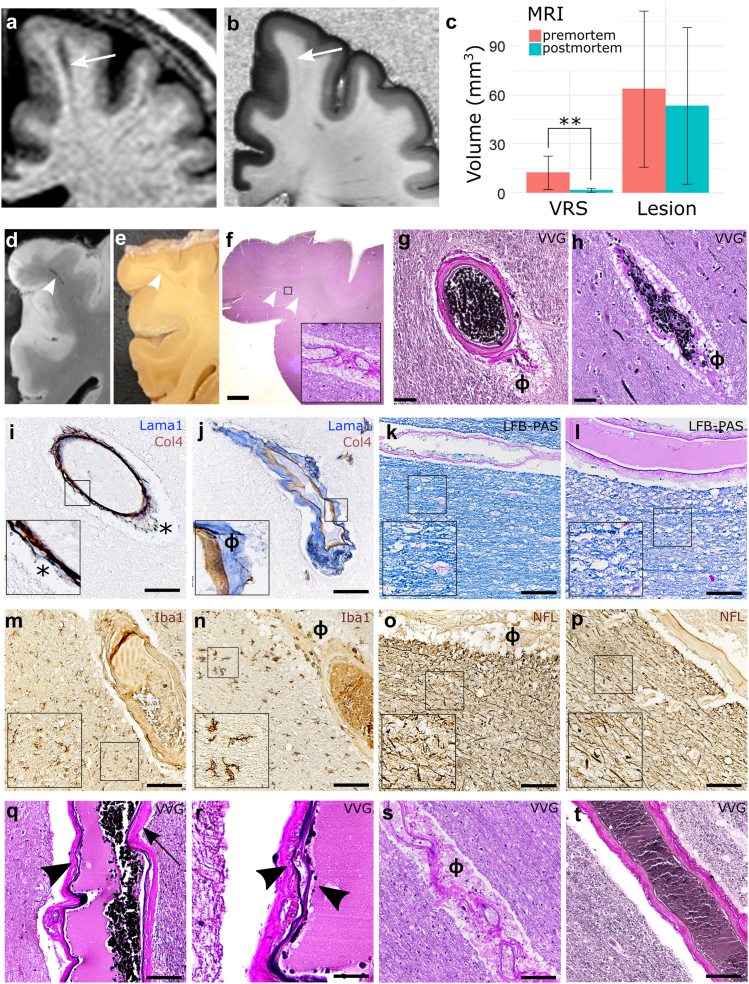
Fig. 5.
Histopathological validation of dilated and non-dilated VRS. (a–c): Dynamic changes of pre- (a) versus post-mortem VRS (b): VRS show a substantial drop in volume from pre- to post-mortem MRI (quantification: (c)). (d–f): VRS, as identified on postmortem T1w MRI scans (d), were correlated to corresponding brain tissue blocks I and paraffin tissue slices ((f), inlet with 200× magnification). VRS corresponded mostly to arteries ((g), ɸ = perivascular space) and to a lesser extent veins (h). (i and j): The perivascular compartments were identified with double staining for laminin α1 (labelling the parenchymal basement membrane, blue) and collagen IV α1 (labelling the vascular basement membrane, brown) (j) which was in contrast to artifacts caused by perimortem vascular collapse (asterisk, (i); inlets with 200× magnification). (k–p): Neither dilated (k, m, o, q, s) nor nondilated VRS (l, n, p, r, t) were associated with demyelination ((k and l), LFB-PAS), activation of microglia/macrophages ((m and n), Iba1), or axonal damage (o and p), neurofilament [NFL]; insets with 200× magnification]. (q–t): Dilated VRS of the arterial tree were more commonly associated with signs of small vessel disease, such as splitting of the internal elastic lamina (arrowhead in (q), 200× magnification, higher magnification in (r), vessel wall hyalinosis (arrow in (q)), or vascular tortuosity (s) compared to nondilated VRS (t). Scale bars = 50 μm, except in f = 1 mm and r = 10 μm. Abbreviations: ɸ, perivascular space; LFB-PAS, Luxol Fast Blue periodic acid-Schiff; MRI, magnetic resonance imaging; VVG, Verhoeff van Gieson; VRS, Virchow-Robin space.