Figure 3. A model of Apnea-induced Anxiety.
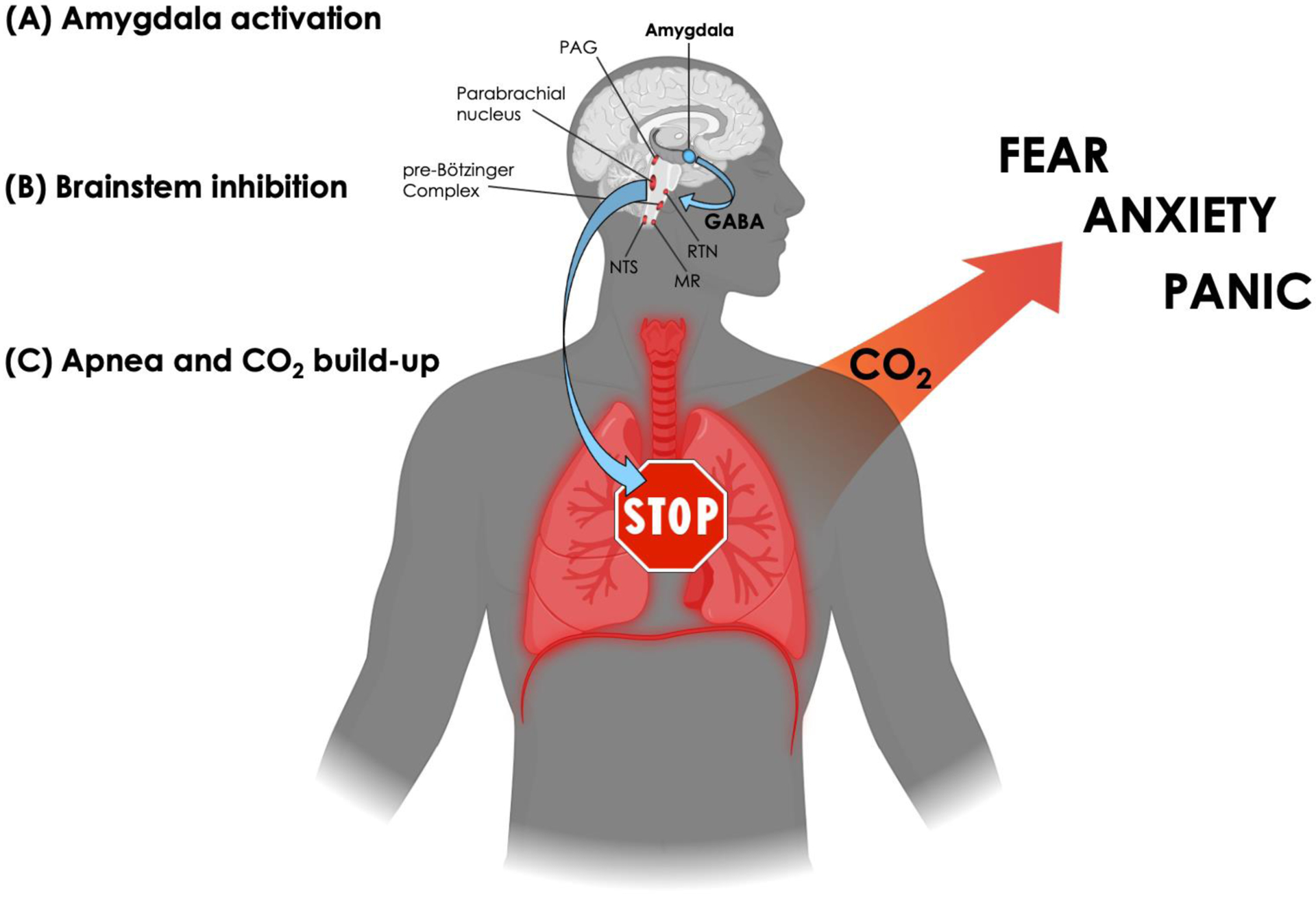
(A) Amygdala activation. The model applies to situations in which amygdala activation surpasses the necessary threshold to elicit apnea. Since a myriad of emotionally laden stimuli can activate the amygdala (Costafreda et al., 2008), the model allows for the possibility that any individual, healthy or anxious, could find themselves in a situation that triggers an episode of apnea.
(B) Brainstem inhibition. The central nucleus of the amygdala will flood downstream targets in the brainstem with GABA, leading to inhibition over respiratory-related nuclei that regulate the rate of breathing (including the periaqueductal gray (PAG) in the midbrain, the parabrachial nucleus in the pons, and the pre-Bötzinger complex in the medulla) as well as inhibition over chemoreceptive-related nuclei that sense changes in CO2 (both centrally in the retrotrapezoid nucleus (RTN) and medullary raphe (MR), and peripherally in the nucleus tractus solitarii (NTS) via projections from the carotid and aortic bodies).
(C) Apnea and CO2 build-up. As inhibition over brainstem respiratory centers accumulates, breathing eventually stops, leading to a transient state of apnea and rising levels of CO2. However, due to amygdalar inhibition over chemoreceptive centers in the brainstem, the individual remains unaware of the CO2 build-up and unaware that their breathing has stopped. Once amygdala activation subsides, and inhibition over the brainstem is lifted, chemoreceptive awareness and respiratory drive returns. The unforeseen build-up of CO2 generated during the episode of apnea rapidly activates suffocation alarms, triggering a state of anxiety characterized by varying degrees of fear and panic, hyperventilation, and avoidance/escape behavior. (Created with BioRender.com)
