Abstract
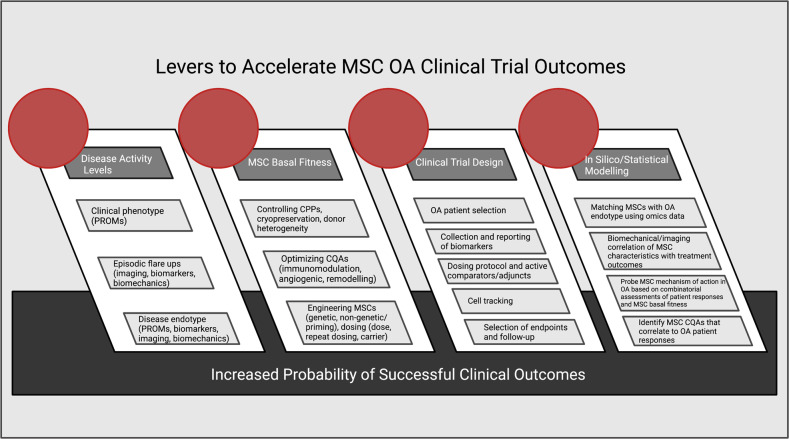
Osteoarthritis (OA) is a degenerative multifactorial disease with concomitant structural, inflammatory, and metabolic changes that fluctuate in a temporal and patient-specific manner. This complexity has contributed to refractory responses to various treatments. MSCs have shown promise as multimodal therapeutics in mitigating OA symptoms and disease progression. Here, we evaluated 15 randomized controlled clinical trials (RCTs) and 11 nonrandomized RCTs using culture-expanded MSCs in the treatment of knee OA, and we found net positive effects of MSCs on mitigating pain and symptoms (improving function in 12/15 RCTs relative to baseline and in 11/15 RCTs relative to control groups at study endpoints) and on cartilage protection and/or repair (18/21 clinical studies). We examined MSC dose, tissue of origin, and autologous vs. allogeneic origins as well as patient clinical phenotype, endotype, age, sex and level of OA severity as key parameters in parsing MSC clinical effectiveness. The relatively small sample size of 610 patients limited the drawing of definitive conclusions. Nonetheless, we noted trends toward moderate to higher doses of MSCs in select OA patient clinical phenotypes mitigating pain and leading to structural improvements or cartilage preservation. Evidence from preclinical studies is supportive of MSC anti-inflammatory and immunomodulatory effects, but additional investigations on immunomodulatory, chondroprotective and other clinical mechanisms of action are needed. We hypothesize that MSC basal immunomodulatory “fitness” correlates with OA treatment efficacy, but this hypothesis needs to be validated in future studies. We conclude with a roadmap articulating the need to match an OA patient subset defined by molecular endotype and clinical phenotype with basally immunomodulatory “fit” or engineered-to-be-fit-for-OA MSCs in well-designed, data-intensive clinical trials to advance the field.
Keywords: MSC, Osteoarthritis, Cell therapy, mesenchymal stromal cell, RCT
Subject terms: Immunology, Inflammation
Introduction
Overview of osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, affecting an estimated 650 million people (654.1 [95% CI, 565.6–745.6]) aged 40 and older worldwide as of 2020, with an incidence of 203 per 10,000 person-years [95% CI, 206–331] [1]. The global age-standardized prevalence of knee OA is estimated to be 3.8%, with a higher prevalence in females than in males [2]. Globally, among the total OA cases in 2019, the knee was the leading anatomic site, accounting for 60.6% of all OA cases [3], and knee OA will be the focus of this review.
OA imposes socioeconomic burdens due to its morbidity, which results in reduced daily activity and productivity. Currently, arthritis costs an estimated US$ 24 billion annually in Canada, with projected increases to US$ 49 billion annually by 2031 [4], and US$ 140 billion annually in the United States of America [5]. Patients with OA experience a significant reduction in their quality of life, yet there are no disease-modifying treatments for this disease. Current treatments include lifestyle changes (exercise, weight loss, and quitting smoking); symptom-modifying injectables [6], including corticosteroids, hyaluronic acid (HA), platelet-rich plasma (PRP); and recently, autologous patient serum containing activated monocyte/macrophages (a mixed population termed as MΦs) [7] that are injected with short- to medium-term analgesic effects. OA is managed with these symptom-modifying approaches until surgical joint replacement can be performed—which is reserved for patients with end-stage OA—leaving a typical 10–20-year gap with limited clinical management of OA morbidity. Joint replacement for OA has a large effect size but is appropriate only at advanced disease stages [8]. With the paucity of effective treatments, there is an urgent need for clinical studies of new and existing therapies.
OA is a multifactorial disease affecting articular cartilage, subchondral bone, menisci (in the knee), synovial tissue (a membrane lining the joint and heterogeneously composed of fibroblasts, MΦs, and endothelial and stromal cells), tendon/ligaments and muscle [9]. While historically OA has been considered a disease of mechanical “wear-and-tear” that leads to the degradation of articular cartilage, more recently, this view has shifted to recognize the important roles of inflammation, metabolic dysregulation, and fibrosis in the complex disease pathophysiology and symptomology. Notably, these pathophysiological mechanisms are interrelated, and while in this review we emphasize the importance of modulating inflammation, we also include a discussion of other disease factors due to this complex interplay.
OA is highly heterogeneous in terms of clinical features and responses to available treatments, as well as through the contribution of different biochemical factors that contribute to the progressive and gradual loss of articular cartilage [9, 10] and bone changes and inflammation that cause joint pain and swelling, which impair patient mobility and quality of life [11]. As such, OA is now better understood not as a single disease but as a collection of different clinical phenotypes [12] with different and/or overlapping molecular endotypes that drive the disease; patients thus present with different combinations of pain, symptoms and dysfunction [13]. Mechanical instability [14, 15], trauma [16], sex [17, 18], age [19–21], obesity [22, 23] and metabolic syndrome [24–26] are major risk factors for knee OA. Within articular cartilage, biomechanical and chemical cues prompt a shift toward a proinflammatory and catabolic (“activated”) chondrocyte phenotype associated with chondrocyte hypertrophy and apoptosis that contribute to cartilage degradation [27–29]. The subchondral bone in OA is characterized by microcracks, bone marrow lesions, neovascularization, and osteophyte formation; this facilitates crosstalk between osteocytes and chondrocytes at the bone-cartilage interface, which is thought to play an important role in regulating the activated chondrocyte phenotype [30–32]. Synovial tissue, consisting primarily of synovial fibroblasts and MΦs [33, 34], is a key source of proinflammatory, catabolic, and profibrotic factors [35–37]. These factors contribute to inflammation, cartilage degradation, and fibrocartilage formation in articular cartilage and joint menisci, leading to joint swelling, stiffness, and pain [35–37]. The synovium becomes increasingly vascularized in OA, allowing increased immune cell infiltration into the joint that further propagates the inflammatory and degradative process [38, 39].
Inflammation plays a critical role in OA, and proinflammatory cytokines such as interleukin-1-beta (IL-1β), IL-6 and tumor necrosis factor alpha (TNF-α) are implicated in OA pathogenesis [40] and are elevated in OA joint tissues and synovial fluid [41, 42]. The joint-specific presence of these proinflammatory mediators drives cartilage catabolism and degradation, resulting in the recruitment of more immune cell infiltrates and perpetuating a negative cascade of increasing inflammation and patient pain and symptoms [43]. Targeting inflammatory mediators in OA is thus key to modifying disease progression [13]. Nonetheless, several single anti-inflammatory therapies, including anti-TNF [10] and anti-IL-1 [11, 12], have failed in clinical trials, although both TNF-α and IL-1β indisputably play key roles in OA pathogenesis. Tellingly, in a systematic review to classify patients based on clinical phenotypes, only 12% of patients fell into the inflammatory phenotype category [12], but this is likely reflective of the temporal nature of OA rather than the limited importance of proinflammatory cytokines in driving molecular endotypes [42]. The temporal, overlapping and heterogeneous complexity of this multi-tissue disease emphasizes the challenges of targeting single pathways for overall treatment effects. Multimodal disease-mitigating agents or combinations of agents are needed and should be matched appropriately to the temporal stage and patient endotype, representing significant headwinds in developing effective OA therapeutics.
Mesenchymal stromal cells (MSCs) for the treatment of OA
MSCs are attractive therapeutic candidates for OA due to their multimodal mechanisms of action, including their immunomodulatory properties. MSCs modulate the inflammatory cytokine milieu and immune cell responses in the joint via the release of secreted paracrine factors and extracellular vesicles (EVs) and through host macrophage-mediated efferocytosis [44–47]. In addition to their immunomodulatory functions, MSCs exert regenerative effects through the release of growth factors, cytokines, organelle transfer, and other molecules that can mediate endogenous repair responses in the host microenvironment. MSCs derived from multiple sources, such as bone marrow, adipose tissue and the umbilical cord, have demonstrated unambiguous preclinical therapeutic efficacy in a wide variety of disease indications on account of these immunomodulatory and reparative properties. MSCs have been investigated in over 5000 patients with a demonstrable safety profile [46–48]. Currently, 10 MSC-based therapies, including Stempeucel®, CARTISTEM®, Prochymal®, Stemirac®, Alofisel®, and others, are approved in certain countries, and more than 1050 clinical trials are registered at clinicaltrials.gov for MSCs targeting multiple disease indications [49–51]. Notably, this includes CARTISTEM®, an allogeneic umbilical cord blood (CB) MSC product by MEDIPOST, approved in S. Korea for the treatment of degenerative arthritis and cartilage defects [52]. Importantly, there are no approved MSC products in the United States of America [53]. Thus, despite the existence of examples of successful global commercial MSC products, including the approval of StemOne®, an allogeneic cell therapy treatment for knee OA approved by the Drug Controller General of India in September 2022 [54], there is also evidence of mixed clinical effectiveness, which has limited commercial success in major markets. With respect to OA, MSC treatment, as assessed in several randomized clinical trials and meta-analyses, improves pain, function, quality of life scores and cartilage volume [46–50, 55], but data are based on limited sample sizes, and larger, high-powered trials are needed to reach definitive conclusions.
In this review, we will examine a curated set of peer-reviewed RCTs and discuss clinical evidence of efficacy from these controlled trials, focusing only on culture-expanded MSCs in treating OA [56–71]. Next, we will deconstruct the mechanisms of action of MSCs in OA and the role of MSC basal immunomodulatory fitness on therapeutic efficacy, highlighting the immunomodulatory role of MSCs and interplay with cartilage-reparative, antifibrotic and angiogenic effects. There are several reviews discussing preclinical MSC mechanisms of action in the treatment of OA [72–75], and we therefore focus our analysis primarily on clinical evidence. We will conclude with a roadmap that incorporates a discussion on stratifying inflammatory OA patients on the basis of baseline clinical phenotypes and disease endotypes, selecting and designing fit and fit-for-purpose MSCs, and incorporating appropriate clinical trial designs as critical next steps in advancing successful MSC clinical trials and enabling commercial MSC therapeutics for knee OA.
Culture-expanded MSCs and randomized, controlled OA clinical trial results
Selection criteria for the inclusion of randomized controlled trials (RCTs)
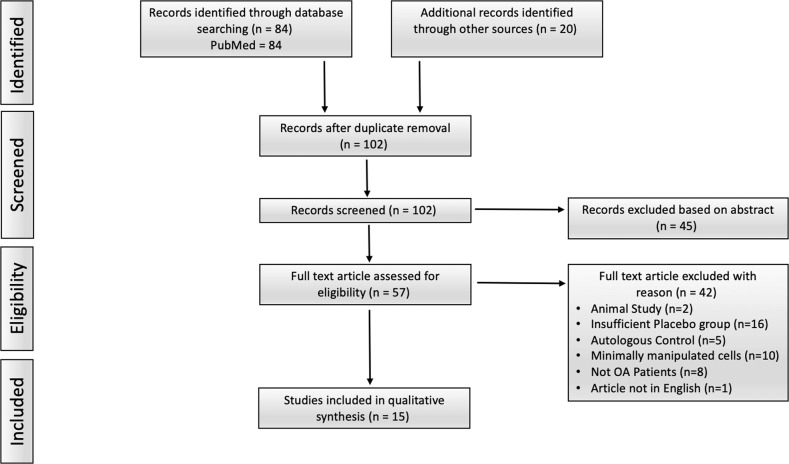
To stringently probe the clinical efficacy of MSC therapies from a larger collection of reported data, we collected published data on RCTs for MSC effects in OA. We reviewed clinical trials from the PubMed database using the following search string: “mesenchymal stromal cell” or “mesenchymal stem cell” or “MSC” or “ASC” (adipose stromal/stem cells) or “MPC” (multipotent precursor/progenitor cell) and “osteoarthritis”. The results were further filtered by “Clinical Trial” and “Randomized Controlled Trial”, resulting in 84 clinical trials. Additionally, recently published meta-analyses [76–80] were cross-referenced to ensure the inclusion of all relevant clinical studies, bringing the total to 102 clinical trials once duplicates were removed. Next, abstracts were screened, and 45 trials were discarded for reasons including trial inclusion of non-OA patients or non-MSC products or lack of randomization. The full articles of the remaining trials were assessed, and the trials were refiltered for eligibility, including only English language articles. Trials with insufficient control groups (16 trials) and of minimally manipulated cells (10 trials), or those meeting other criteria specified in Fig. 1, were excluded. It is important to note that we did not include trials of bone marrow aspirate concentrates, stromal vascular fractions or other minimally manipulated cellular sources, focusing only culture-expanded MSCs to consistently analyze the available clinical evidence, which represents a departure from previous systematic reviews [81–85].
Fig. 1.
PRISMA flow diagram of the literature selection process. PubMed search string “((((((MPC) OR (Mesenchymal stem cell)) OR (MSC)) OR (ASC)) OR (Mesenchymal stromal cell)) AND (Osteoarthritis) + Clinical Trial + RCT”
Our approach resulted in 15 peer reviewed RCTs that we compared based on dosing, tissue source, MSC therapeutic product volume and carrier, clinical trial duration, and outcomes assessed by primary and secondary endpoints [56–71]. Overall, the 15 RCTs discussed in this section included patients who were treated with various doses of MSCs, ranging from 3.9 × 106 to 150 × 106 cells, or control treatments, including saline, PRP, HA, and others (Table 1). Of the RCTs analyzed in this section, 60% investigated MSCs from autologous sources, while the remaining 40% used allogeneic MSCs. Nearly half (7/15) of the RCTs involved bone marrow-derived MSCs (denoted MSC(M)); 6 of 15 used adipose tissue-derived MSCs (denoted MSC(AT)), and one study each used placenta tissue or Wharton’s jelly MSCs (MSC(WJ)). Although 15 RCTs were included, the total number of MSC-treated and control patients was small (610), making it difficult to render definitive conclusions regarding effect sizes, as has been noted in previous meta-analyses [76–80].
Table 1.
Randomized control trials of culture-expanded mesenchymal stromal cells
| Author | MSC Tissue Source | Cells/Dose (x106) | Treatment Group Intervention | Control Group Intervention | Sample Size (Treatment/Control) | Male/Female | Baseline Pain Scores (VAS/WOMAC/KOOS) | Follow-up Duration (months) | Follow-up Evaluation |
|---|---|---|---|---|---|---|---|---|---|
| Autologous | |||||||||
| Lee et al. [57] | AT | 100 | sIA injection of MSCs in 3 mL of saline | sIA injection of 3 mL saline |
24 12/12 |
6/18 |
MSC: 60/NA/NA Control: 56.4/NA/NA |
0, 3, 6 |
WOMAC, VAS, KOOS, ROM, MRI (0, 6 months) |
| Freitag et al. [58] | AT | 100 | sIA injection of MSCs or 2 IA injections of MSCs at 0 and 6 months each suspended in 3 mL of saline | Ongoing conventional conservative management only |
30 20/10 |
16/14 |
sIA MSC: NA/59.6/53 dIA MSC: NA/54.4/52.1 Control: NA/58.8/52.8 |
0, 1, 3, 6, 12 |
NPRS, KOOS, WOMAC, MOAKS (0, 12 months) |
| Lamo-Espinosa et al. [59] | M | 100 | sIA injection of MSCs suspended in 3 mL of Ringers Lactate solution followed by weekly injections of PRP (PRGF®), weekly, for 3 weeks (final volume of 8 mL) | sIA injection of PRP (PRGF®), weekly, for 3 weeks (final volume of 8 mL) |
56 28/28 |
33/18 |
MSC: 5.3/33.4/NA Control: 5/31.9/NA |
0, 3, 6, 12 |
VAS, WOMAC, WORMS (0, 12 months) |
| Lamo-Espinosa et al. [56, 60] | M | 10, 100 | sIA injection of low dose or high dose MSCs suspended in 1.5 or 3.0 mL of Ringers Lactate solution, respectively. Both followed by a sIA injection of 4 mL HA (Hyalone®) | sIA injection of 60 mg HA (Hyalone®) in a final volume of 4 mL |
30 20/10 |
17/8 |
10-MSC: 7/37/NA 100-MSC: 6/28/NA Control: 5/29/NA |
0, 3, 6, 12, 48 |
VAS, WOMAC, OARSI, WORMS (0, 6, 12 months) |
| Lu et al. [61] | AT | 50 | 2 IA injections of MSCs at 0 and 3 weeks, SHAM injections at week 1 and 2, suspended in 2.5 mL | 4 IA injections of 2.5 mL HA (week 0, 1, 2, and 3) |
52 26/26 |
6/46 |
MSC: R 5.50, L 5.27/33.77/NA Control: R 4.96, L 4.92/32.15/NA |
0, 6, 12 |
WOMAC, VAS, SF-36, MRI (0, 6, 12 months) |
| Emadedin et al. [63] | M | 40 | sIA injection of MSCs in 5 mL of saline | sIA injection of 5 mL saline |
47 31/39 |
27/16 |
MSC: NA/NA/NA Control: NA/NA/NA |
0, 3, 6 | VAS, WOMAC, MCII, PASS |
| Bastos et al. [62] | M | 40 | sIA injection of MSCs in either 10 mL of PRP or PBS | sIA injection of corticosteroid (4 mg dexamethasone) |
47 30/17 |
24/23 |
MSC: NA/NA/30.3 MSC-PRP: NA/NA/37.3 Control: NA/NA/36.9 |
0, 1, 2, 3, 6, 9, 12 | KOOS, ROM |
| Wong et al. [64] | AT | 14.6 | HTO + Microfracture + sIA injection of MSC suspended in 2 mL of HA | HTO + Microfracture + sIA injection of 2 mL HA |
56 28/28 |
29/27 |
MSC: NA/NA/NA Control: NA/NA/NA |
0, 6, 12, 24 | IKDC, Lysholm, Tegner, MOCART (0, 12 months) |
| Koh et al. [71] | AT | 4.11 | HTO + sIA injection of MSCs suspended in 3 mL of PRP | HTO + sIA injection of 3 mL PRP |
52 26/26 |
11/33 |
Control: 45.4/NA/NA MSC: 44.3/NA/NA |
0, 3, 12, 14–24 |
KOOS, Lysholm, VAS, Radiograph (0, 24 months) |
| Allogeneic | |||||||||
| Gupta et al. [65] | M | 25, 50, 75, 150 | sIA injection of MSCs suspended in 2 mL (25 & 50) or 4 mL (75 and 150) of PLASMA-LYTE A + 20 mg (2 mL) HA | sIA injection of either 2 or 4 mL PLASMA-LYTE A |
60 40/20 |
15/45 |
25-MSC: 60.9/1315.8/NA 50-MSC:73.7/1498.4/NA Control-2: 61.0/1239.6/NA 75-MSC: 57.4/1470.6/NA 150-MSC: 46.6/1388.1/NA Control-4: 65.3/1382.0/NA |
0, 1, 3, 6, 12 |
VAS, ICOAP, WOMAC Index MRI (0, 6, 12 months) |
| Chen & Hu et al. [66] | AT | 16, 32, 64 | sIA injection of MSCs suspended in 8 × 106 cells/mL with cryoprotectant CryoStor® CS10 | sIA injection of Hya Joint Plus 3 mL synovial fluid supplement |
57 49/8 |
11/46 |
MSC: NA/NA/NA Control: NA/NA/NA |
0, 1, 3, 6, 9, 12 | WOMAC, VAS, KSCRS |
| Soltani et al. [67] | Placenta | 50–60 | sIA injection of MSCs suspended in 10 mL of culture media | sIA injection of 10 mL saline |
20 10/10 |
2/18 |
MSC: NA/NA/NA Control: NA/NA/NA |
0, 2, 6 |
VAS, KOOS, ROM, MRA (0, 6 months) |
| Vega et al. [68] | M | 40 | sIA injection of MSCs suspended in 8 mL of Ringer-lactate | sIA injection of 60 mg HA |
30 15/15 |
11/19 |
MSC: 54/41/NA Control: 64/45/NA |
0, 6, 12 |
VAS, WOMAC, Lequesne SF-12, MRI (0, 6, 12 months) |
| Matas et al. [69] | WJ | 20 | 2 IA injection of MSCs at 0 and 6 months or 1 IA injections of MSCs at 0 months and IA injection of saline at 6 months | 2 IA injection of HA at 0 and 6 months |
29 21/8 |
11/18 |
sIA MSC: 44.8/37.4/NA dIA MSC: 39.4/35.6/NA Control: 38.7/28.9/NA |
0, 1, 2, 3, 6, 9, 12 |
WOMAC, VAS, SF-36, WORMS (0, 6, 12 months) |
| Kuah et al. [70] | AT | 3.9, 6.7 | sIA injection of MSCs suspended in 2 mL | sIA injection of cell supernatant |
20 16/4 |
12/8 |
3.9-MSC: 57/6.6/NA 6.7-MSC: 60.8/7.9/NA Control: 43.8/6.3/NA |
0, 1, 3, 6, 9, 12 |
VAS, WOMAC, AQoL-4D, MRI (0, 12 months) |
M bone marrow, AT adipose tissue, WJ Wharton’s jelly, sIA single intra-articular injection, dIA double intra-articular injection, HA hyaluronic acid, PRP platelet-rich plasma, KOOS knee injury and osteoarthritis outcome score, VAS visual analog scale, ROM range of motion, MOAKS MRI osteoarthritis knee score, IKDC International Knee Documentation Committee, MRI magnetic resonance imaging, WOMAC Western Ontario McMaster Universities Arthritis Index, MOCART magnetic resonance observation cartilage repair tissue, MCII minimally clinically important improvement, PASS patient acceptable symptom state, KSCRS new Knee Society Clinical Rating System, WORMS whole-organ magnetic resonance imaging score, HTO high tibial osteotomy, PBS phosphate-buffered saline, MSC mesenchymal stromal cell, ICOAP intermittent and constant pain score, SF-36 36-Item Short Form Survey, SF-12 12-Item Short Form Health Survey, AQoL-4D assessment of quality of life 4D questionnaire, NPRS numeric pain rating scale
Demographically, of the 610 treated patients, 356 patients (59%) were female, and 231 (38%) were male, while sex was not specified for 22 patients (3%). The average ages of patients per treatment group were generally between 50 and 60 years, with few outliers. Patients with knee OA as diagnosed by radiological and clinical evidence of OA [86] with Kellgren-Lawrence (KL) grades ranging from 1–4 were included in 13 of the 15 RCTs. Multiple clinically relevant endpoints, including the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Visual Analog Scale (VAS) score, International Knee Documentation Committee (IKDC) score, Knee Injury and Osteoarthritis Outcome Score (KOOS), Numeric Pain Rating Scale (NPRS) score, and others, were used as patient-reported outcome measures (PROMs) and varied by study.
Overall, we observed a net positive treatment effect of MSCs, with clinical trials demonstrating improvement in VAS (9/12 trials), KOOS pain (4/5), WOMAC pain and total (9/11) or NPRS (1/1) scores relative to within-group baselines at their respective endpoints. There was considerable variation in the timing of endpoint collection among trials, including endpoint collection at 6 months (14/15 or 93%), 12 months (12/15 or 80%), and 24 months (3/15 or 20%). Overall, 12/15 RCTs showed improvements in most of their respective endpoints at final follow-up relative to baseline values, while relative to control groups, 11/15 trials found significantly better clinical outcomes. Our observations align with those of several meta-analyses that have reported positive effects of MSC treatments in OA [76–80].
RCT patient populations
To further understand the differential responses to MSC treatments, we further investigated the heterogeneous OA patient populations enrolled in these trials. Some trials, including those of Freitag et al. [58] and Koh et al. [71], had a minimum age of 18 years, while Kuah et al. [70] and Matas et al. [69] restricted enrollment to patients aged 40–65 years old. Despite this variation and the limited sample sizes (average MSC treatment group N = 24.8), the mean ages for MSC treatment groups ranged from only 50.7 to 65.9 years across 14/15 studies, representative of an age range with a higher prevalence of OA [56–71]. Due to the higher prevalence of females with OA, we expected and observed a higher proportion of females (357, 59%) relative to males (231, 38%) treated. Furthermore, none of the studies, due to sample size limitations, included analyses based on sex or gender, which represent important variables that may influence treatment responses [87].
Fourteen out of fifteen RCTs reviewed in this section classified patients by KL grade, typically enrolling patients with KL grade 2–3 knee OA. However, within this classification, there is considerable heterogeneity in clinical phenotype (and disease endotype). We tried to parse differences in clinical phenotype looking at baseline pain scores (Table 1); 6/15 and 5/15 studies reported VAS and WOMAC scores, respectively. Other studies used the KOOS, Lysholm, Tegner, NPRS, IKDC and whole-organ magnetic resonance imaging score (WORMS). There were two studies that did not provide baseline values at all [63, 67] and one that provided values only as changes from baseline, which limits comparison between studies. Although most studies reported similar baseline scores, there was some variability that confounded the analysis of effective MSC dosing, as discussed below. Notably, two studies reported baseline VAS scores that varied by at least 10 mm between the treatment and control groups. Kuah et al. reported a baseline control VAS score of 43.8, much lower than the baselines for MSC groups of 57.0 and 60.8 for the 3.9 and 6.7 × 106 dose groups, respectively [70]. The baseline VAS score in the Vega et al. study was 54 in the MSC group and 64 in the control group [70]. Clinical baseline phenotyping is clearly an important variable, and targeting patients with the right clinical phenotype and disease endotype will be key to successful future MSC clinical trials and outcomes in OA.
MSC dose comparisons in RCTs
The studies included in RCT analyses used a range of doses from 3.9 × 106 to 150 × 106 cells. Dose optimization is not fully understood, with only 4/15 studies performing a dose escalation evaluation. Three of the four dose escalation groups received cells that were cryopreserved and subsequently thawed immediately prior to injection, while Lamo-Espinosa et al. used freshly cultured MSCs. Most of the studies showed positive effects of MSCs at moderate to high doses (>40 × 106 MSCs), although as we discuss throughout this section, baseline patient phenotype and endotype, as well as other factors distinct among studies, may be confounding variables. Lamo-Espinosa et al. showed that only the higher dose of 100 × 106 MSC(M), suspended in a 3 mL volume of Ringer’s lactate and coadministered with 4 mL of HA, was able to provide a significant improvement in the overall WOMAC score at 12 months. The moderate dose of 10 × 106 MSC(M) suspended in 1.5 mL of Ringer’s lactate and coadministered with 4 mL of HA did not result in significant improvements in the WOMAC pain and function subscale scores. However, there was a significant improvement in the WOMAC stiffness subscale score at both 6 and 12 months. They also reported nonsignificant reductions in cartilage volume changes by magnetic resonance imaging (MRI) for the high-dose group at 12 months, while no changes were observed in the low-dose or HA groups, suggestive of possible chondroprotective effects of the higher doses of MSC(M), as discussed further in the next section [60].
Differential median baseline WOMAC total scores for the 10 × 106 vs. 100 × 106 dose reflective of variations in patient clinical phenotype and endotype might have contributed to the differential efficacy of the MSC doses [60]. This concept is supported by the findings of the study by Kuah et al. [70], in which patients with lower (albeit not statistically significant) baseline VAS scores were randomized to the group receiving a lower dose (3.9 × 106) of MSC(AT), which showed good efficacy, while patients with lower baseline pain scores in the Lamo-Espinosa et al. trial were randomized to the group receiving a high dose (100 × 106) of MSC(M), which showed better efficacy than the moderate dose (10 × 106) at the 12-month endpoint [60].
Lamo-Espinosa et al. conducted a subsequent 4-year follow-up study with 27 of the 30 patients [56]. Both the high (100 × 106) and moderate (10 × 106) MSC(M) dose groups continued to show significant differences according to VAS scores relative to the control group. Strikingly, overall WOMAC scores were significantly improved in the moderate- but not high-dose MSC(M) group relative to the control group at 48 months. The control group treated with HA alone showed short-term improvements in WOMAC pain, function, and overall scores at 3 and 6 months, but not at longer follow-up timepoints of 12 or 48 months. The observed differences in WOMAC scores at 48 months between the high- and moderate-dose groups suggest the need for longer follow-ups and additional baseline patient clinical phenotyping and endotyping (discussed in the Roadmap section) to understand the differences in personalized disease trajectories in the high- vs. moderate-dose groups. Interestingly, the moderate-dose group with more baseline pain (higher WOMAC scores) showed better WOMAC scores than the control group at the 48-month timepoint.
Similarly, Chen and Hu et al. demonstrated improvements in overall WOMAC scores at 48 weeks posttreatment in the group receiving the highest dose (64 × 106) of allogeneic MSC(AT) relative to HA controls; all dose groups (16 × 106, 32 × 106, and 64 × 106) showed improvements in WOMAC total scores and stiffness, pain, and function subscores from baseline to 48 weeks posttreatment [66]. The Knee Society Clinical Rating System (KSCRS) symptom score was significantly different at week 48 in the 64 × 106 high-dose group vs. the HA control group. Interestingly, the moderate dose group (16 × 106) had significantly higher (less severe) baseline KSCRS patient satisfaction scores, suggestive again of baseline clinical phenotype effects of patient selection on observed treatment outcomes.
Conversely, two studies, Gupta et al. [65] and Kuah et al. [70] showed more efficacious outcomes at lower MSC doses. Gupta et al. included 25 × 106, 50 × 106, 75 × 106, and 150 × 106 pooled bone marrow allogeneic MSCs (Stempeucel®) combined with HA injections. Although the study was not adequately powered for definitive dose comparisons (N = 10 patients/dose group, N = 20 for control group), the authors observed a trend toward pain reduction measured by VAS, WOMAC and Intermittent and Constant Pain Score (ICOAP) scoring criteria in the low-dose group (25 × 106 cells); this was not statistically significant when compared to control (Plasma-Lyte A) [45]. Importantly, Gupta et al. included MSC(M) derived from pooled allogeneic donors (N = 3), and there is clinical evidence in patients with graft-versus-host disease (GVHD) that pooled bone marrow MSCs have greater efficacy than single-donor bone marrow MSCs [88].
Kuah et al. [70], similar to Gupta et al. [65], showed that cryopreserved allogeneic MSC(AT) delivered with cell supernatant were efficacious at lower doses of 3.9 × 106 and 6.7 × 106 in significantly improving WOMAC pain subscale scores at 6 months, but this effect was sustained at 12 months only in the low-dose (3.9 × 106) group [70]. However, none of the WOMAC subscale scores were significantly different between the control (culture supernatant) and MSC(AT) groups at the 12-month timepoint. Kuah et al. used MSC(AT) from individual, nonpooled healthy donors, different from the Gupta et al. studies with pooled MSC(M). Furthermore, the tissue sources differed between the two studies. Additionally, relative to all the MSC(M) treatment groups in the study by Gupta et al. (except their 150 × 106 MSC(M) group), the patients in the Kuah et al. study in the 3.9 × 106 and 6.7 × 106 dose groups had lower mean baseline VAS pain scores of 57.0 and 60.8, respectively. The 25 × 106, 50 × 106, 75 × 106 and 150 × 106 dose groups in the Gupta et al. study had mean baseline VAS scores of 67.0, 78.8, 71.3, and 62.0, respectively. Thus, MSC dosing needs to be viewed in the context of baseline patient clinical phenotype and, as we discuss later, disease endotype. Interestingly, Kuah et al. randomized patients with lower (albeit not statistically significant) baseline VAS scores to the lower dose (3.9 × 106) MSC(AT) group, while Lamo-Espinosa et al. randomized patients with lower baseline pain scores (based on the WOMAC) to the high dose (100 × 106) MSC(M) group [60]. In both cases, the patients with the lower baseline clinical phenotype responded more efficaciously to MSCs, irrespective of dosing.
Taken together, the limited RCT data on dose escalations provide no evidence of a clear winner in terms of patient-reported outcomes. While both the Gupta et al. [65] and Kuah et al. [70] groups showed that lower doses of allogeneic MSCs were better (although neither were statistically significant vs. controls at 12 months), Lamo-Espinosa et al. [60], Chen and Hu et al. [66] concluded that higher allogeneic MSC(M) or MSC(AT) doses were better, showing statistically significant differences in WOMAC scores at 12 months. However, the longer 48-month follow-up by Lamo-Espinosa et al. [56] did not show sustained improvements in PROMs in the higher 100 × 106 MSC(M) group. Furthermore, cartilage volume losses at 12 months (discussed in detail below) did not change at the higher doses but were reduced at the lower dose and in the control HA group [60], suggestive of greater chondroprotective effects at higher MSC doses. Two meta-analyses on the use of MSCs in OA (albeit including a group receiving a mixture of culture-expanded MSCs and minimally manipulated cells) found that medium to higher doses were more effective and cited 40 × 106 cells [89] or 50 × 106 cells [81] as the cell threshold for significant patient-reported benefits. Our nonstatistical analyses are supportive of moderate to higher MSC doses, but we note that the effects of baseline patient pain scores, differences between pooled versus single allogeneic donors, differences in MSC tissue sources, the use of MSC therapies in combination with other bioactive agents, and other variables confound the effects of MSC dosing. Matching the clinical phenotype (and disease endotype of OA patients) to MSC basal fitness seems to be key to achieving successful clinical outcomes.
Repeat MSC injection RCTs
There are only three published RCTs in which repeat MSC intra-articular injections were administered. Freitag et al. used cryopreserved autologous MSC(AT) at doses of 100 × 106 cells suspended in 3 mL saline [58]; Matas et al. opted for cryopreserved 20 × 106 allogeneic MSC(WJ) [69]; and Lu et al. used cryopreserved 50 × 106 autologous MSC(AT). Matas et al. and Freitag et al. designed their trials to be run with three treatment groups receiving either a single or double intra-articular MSC injections (6 months apart) vs. a control group. Lu et al. injected 50 × 106 MSC(AT) at 0 and 3 weeks along with sham injections at weeks 1 and 2, which were compared to 2.5 mL HA injections at weeks 0, 1, 2, and 3.
Interestingly, Freitag’s group initially included a fourth arm of 40 × 106 MSC(AT) injected at higher monthly frequencies (1, 2, 3 and 6 months) that was scrubbed due to emerging data showing injection-site pain with frequent monthly injections [75]. Although there were significant improvements for both treatment groups (single injection; N = 10, double injection; N = 10) compared with the control group (conservative management; N = 10), there was no significant difference between the single- and double-injection groups at least in KOOS and WOMAC scores at the 12-month completion of the study. A combined metric of KOOS, WOMAC, and NPRS scores was used to calculate the percentage of participants achieving a minimal clinically important difference at 12 months relative to baseline values, and values of 25.7%, 84.1%, and 87.1% were found for the control, single, and double injection groups, respectively. Notably, while there were no differences in KOOS and WOMAC scores at 12 months between the single- and double-injection groups, there was a reduction in cartilage volume losses in the double- vs. single-injection groups. Interestingly, as in this example, we have noticed a pattern in which structural changes and PROMs tend to occur independently, with improvements in only one or the other occurring at a time.
Conversely, the design of the Matas et al. trial included a control group (N = 8) that also received repeat dosing of intra-articular HA, while the single injection MSC(WJ) group (N = 9) received a control second injection at 6 months. The double injection MSC(WJ) group (N = 9) received 20 × 106 cells in 3 mL of saline at both baseline and 6 months postinjection. Using both the WOMAC total and pain scores, significant improvements were observed in the double injection MSC(WJ)-treated vs. HA groups. This is especially consequential because the HA control group also received a second injection at 6 months that boosted the previously waning WOMAC pain and function subscale score improvements [69]. The single injection MSC(WJ)-treated group showed continued improvements up to 9 months, but WOMAC scores reverted toward the levels of the HA control group (after the second HA injection) at the 12-month follow-up. Longer follow-up times would have afforded a better evaluation of the synergistic or additive effects of the double MSC(WJ) injections. Interestingly, Matas et al. did not report changes in cartilage volume with single vs. dual injections.
The Lu et al. trial employed a unique dosing method in which four injections were given a week apart for both the MSC and control groups. The control group received four 2.5 mL injections of HA, while the treatment group received 50 × 106 MSC(AT) during the first and third injections and 2.5 mL of HA in the second and final weeks. During both the 6- and 12-month follow-ups, there were significant improvements in VAS pain scores relative to the HA control group and significantly increased cartilage volumes relative to baseline in terms of modified WORMS, while the HA control group showed cartilage volume losses at 12 months [61].
Taken together, all three trials reported benefits of dual injections, although only the Matas and Lu trials showed differences in PROMs at 12 months, while the Freitag and Lu trials showed gains in cartilage volume or a lack of cartilage volume losses at 12 months with dual injections.
Autologous vs. allogeneic MSCs in RCTs
RCTs investigating autologous MSCs made up the majority (9/15) of the studies reviewed, while the remaining (6/15) studies investigated MSCs of allogeneic origin. The autologous tissue of origin was split between bone marrow (5/9) and adipose tissue (4/9), while allogeneic sources were split between adipose tissue (2/6) and bone marrow (2/6). The remaining allogeneic trials used MSCs from Wharton’s jelly (1/6) or the placenta (1/6). Most of the dose escalation trials (3/4) used allogeneic MSC sources, while the three repeat injection trials were divided two-to-one between autologous and allogeneic MSCs [60, 65, 66, 68–70, 75].
In 5/6 of the MSC allogeneic trials, there was a significant improvement in PROMs (WOMAC, KOOS, and KSCRS scores) relative to the control groups. This was true regardless of doses ranging as low as 3.9 × 106 MSC(AT) [70] and as high as 64 × 106 MSC(M) [70]. The exception was the Gupta et al. [65] trial using cryopreserved pooled MSC(M) doses combined with HA injection, which were unable to achieve a significant difference from the control treatments at 12 months in terms of VAS or WOMAC scores [65]. However, the lowest dose was most efficacious in reducing pain scores. Taken together, 5/6 allogeneic MSC trials reported positive patient outcome effects at low to moderate doses (3.9–40 × 106 MSCs) [66–70].
Similarly, in 8/9 RCTs using autologous MSCs, there was significant improvement in PROMs [56–62, 71]. Typically, the autologous studies used doses from 10–100 × 106 MSCs, including the studies of Bastos et al. [62], Wong et al. [64], and Lamo-Espinosa et al. [56, 60]. The exception was the trial of Koh et al., who performed high tibial osteotomy in addition to administering low-dose (4 × 106) MSC(AT) and 3 mL of PRP, which resulted in significant improvement in VAS pain scores relative to the high tibial osteotomy and PRP alone control group [71]. Two studies used saline as a control [57, 63]. The use of saline as a control necessitated an earlier 6-month endpoint. Emadedin et al. showed a mean change in overall WOMAC scores of >10 points in the MSC(M) vs. saline groups at 6 months [63]. Lee et al. showed significant improvements in WOMAC scores at 6 months in the MSC(AT) group but not the saline control group [57]. Freitag et al. showed that repeat moderate-dose (40 × 106) autologous MSC(AT) injections improved WOMAC total scores relative to conservative management [58]. Taken together, from the limited dataset on RCTs, moderate to higher doses (10–100 × 106) of autologous MSCs (except for in the study of Koh et al., who used 4 × 106 autologous MSC(AT) in combination with PRP and surgical intervention) resulted in positive PROMs at the study endpoints. These findings suggest that although the efficacy of MSCs has been demonstrated relative to the current standard of care at various cell doses, there is no definitive dose range that has been reproducibly and consistently shown to be efficacious; multiple factors, including OA patient clinical phenotype, molecular endotype, and MSC basal fitness, need to be considered, matched and optimized.
In summary, the 15 RCTs with 610 treated patients showed positive effects of MSCs relative to control treatments at 12-month timepoints in terms of PROMs. However, clear distinctions are not apparent in regard to dose dependencies, MSC tissue of origin, and autologous or allogeneic MSC sources. We did note that in 7/9 autologous MSC trials, moderate to high (10 × 106—100 × 106) MSC doses were used, while 5/6 allogeneic MSC trials used low to moderate doses (4 × 106—40 × 106), suggesting possible augmented basal fitness of allogeneic-, nonpatient-derived MSCs. However, culture parameters to expand MSCs and cryopreservation/thawing can further affect basal fitness, as previously reported [90, 91]. Additionally, we noted variations in baseline VAS or WOMAC scores across the 15 RCTs and between treatment groups within a given trial that were suggestive of differences in the clinical phenotype of patients that further confound MSC dosing effects. All clinical trials reported PROMs, while 10/15 reported effects on cartilage repair, and a few reported changes in local and systemic biomarkers (3/15) [62, 66, 70]. The mechanisms through which MSCs may exert these observed changes are discussed in the next section.
MSC mechanisms of action in knee OA
Despite the completion of 15 peer-reviewed RCTs, there is limited evidence on the clinical mechanism of action of MSCs in OA. An improved understanding of the mechanism of action would be beneficial in the following ways: (i) it would facilitate the design of improved MSC therapies with properties tailored to achieve the desired effects in OA; (ii) it would facilitate the selection of critical quality attributes (CQAs) for MSC investigational products that are relevant to the mechanism of action and could be used as potential release criteria; (iii) in patient stratification or precision medicine-based approaches, it could facilitate the selection of patients with a higher response likelihood to MSC interventions based on disease status biomarkers relevant to the therapeutic mechanism of action; and (iv) it would facilitate the selection of relevant readouts or biomarkers that inform clinical responses based on the expected clinical effects of an MSC intervention.
To underscore the importance of understanding the mechanism of action, a previous biologic license application for Remestemcel-L™, an allogeneic MSC(M) product for the treatment of steroid-refractory acute GVHD, was rejected by the United States Food and Drug Administration (FDA), partially due to the inadequacy of the CQAs employed by the sponsor; the researchers did not demonstrate a clear relationship of the MSC CQAs to the clinical potency of the product [92]. The FDA statement also noted that while the assays used as CQAs—MSC(M) expression of TNF receptor 1 protein and MSC(M)-mediated inhibition of IL-2Rα expression in activated lymphocytes—were aligned with the hypothesized immunomodulatory mechanism of action for the MSC(M) product, there was a lack of clinical evidence submitted to support this mechanism [92]. The FDA recommended using a multivariate matrix of CQAs, as we have recently proposed [92]. Altogether, while the mechanisms may be complex and multimodal for MSC therapy, particularly in the context of OA, understanding these mechanisms is key for obtaining regulatory authorization and for eventual refinement of MSC therapies.
The following subsections provide an overview of current insights into MSC mechanisms of action in OA, with emphasis on immunomodulatory mechanisms. We provide an overview of in vitro and preclinical studies that provide insights into MSC-mediated immunomodulation as an important mechanism of action in OA. We further detail the clinical evidence (beyond the 15 RCTs in the previous section) where available, discussing immunomodulatory, chondroprotective, regenerative and other effects of MSCs in the treatment of knee OA.
MSC anti-inflammatory and immunomodulatory effects on OA
MSC-mediated anti-inflammatory and immunomodulatory effects on OA inflammation are also known to play a central role in OA, with both innate and adaptive mediators involved in the pathophysiology [93]. In particular, the synovium, consisting primarily of fibroblast-like synoviocytes and MΦs, becomes inflamed in OA; neovascularization as well as a leaky endothelium within the subintimal layer allows increased cellular and molecular infiltration within the synovium and synovial fluid [94]. Lineage-tracing experiments in a rheumatoid arthritis mouse model have also indicated the presence of a self-renewing population of resident synovial MΦs that may represent a source of additional immune cells in the synovium [95]. The infrapatellar fat pad within the knee joint is also highly vascularized and contributes to increased levels of inflammatory cells and mediators [96]. MΦs produce inflammatory and catabolic mediators in OA, and our group has shown that MΦs represent the most abundant leukocyte population within the synovial fluid of OA patients [97]. Indeed, CD14+CD16- (classical) and CD14+CD16+ (intermediate) MΦ subpopulations were found to be positively and negatively correlated with more severe PROMs in a cohort of knee OA patients [97]. The synovial membrane in OA contains several other immune populations, including T and B cells, natural killer cells, neutrophils, dendritic cells, mast cells, and granulocytes, that play roles in OA pathology [97]. In particular, T cells are relatively abundant within the OA synovium and synovial fluid, and altered profiles of T-cell subsets, including Th1, Th17, and Treg cells, have been documented [98]. We have further shown that activated T-cell subsets correlate with different MΦ subsets [97]. Anti-inflammatory and immunosuppressive effects of MSCs on MΦs and T cells have been widely documented [99, 100] and thus represent plausible cellular effectors of intra-articular injections of MSCs in OA.
Evidence of the anti-inflammatory and immunomodulatory functionality of MSCs has been extensively reviewed in various preclinical studies [72, 101]; nonetheless, we highlight some of the key findings here to provide context for immunomodulation as a primary MSC mechanism of action. Notably, work by Fahy et al. demonstrated that conditioned medium derived from human OA synovial macrophage cultures inhibited chondrogenic differentiation of MSC(M) [102]. In vitro polarization of human peripheral blood-derived monocytes to proinflammatory subtypes had similar effects on inhibiting MSC(M) chondrogenic differentiation, suggestive of a potential proinflammatory blockade of chondrogenic differentiation in an OA joint. The presence of IL-6, CCL18 and other proinflammatory factors in synovial macrophage conditioned medium was thought to inhibit MSC(M) chondrogenic differentiation. Thus, addressing proinflammatory imbalance in the joint may be a prerequisite to enabling endogenous chondroprogenitor differentiation and proliferation repair mechanisms. In vitro, MSC(AT) showed anti-inflammatory effects on OA chondrocytes and synoviocytes harvested from the femoral condyle of OA patients undergoing total knee replacement [103]. Indirect cocultures of MSC(AT) with OA chondrocytes demonstrated reduced hypertrophy and promoted a mature differentiated chondrocyte phenotype, while more modest anti-inflammatory effects were observed with MSC(AT)-conditioned medium, suggesting the importance of cross-talk between MSC(AT) and chondrocytes in mediating these effects. These data support the hypothesis that MSCs enable chondrocyte repair and tissue remodeling in part by alleviating anti-inflammatory cues that inhibit chondrocyte proliferation and appropriate differentiation.
The hypothesis that immunomodulation and inflammation play a central role in MSC-mediated OA repair and tissue remodeling is further supported by data from our laboratory showing that iron nanoparticle-labeled syngeneic murine MSC(M) injected into immunocompetent C57Bl/6 mice with surgically induced OA were retained within the synovium up to 4 weeks postsurgery; importantly, the presence of the iron-labeled MSC(M) was confirmed with dual Prussian Blue and SCA-1+ (a murine MSC marker) cell staining by immunohistochemistry [104]. We additionally showed that these MSC(M) were apoptotic and phagocytosed by CD206+ MΦs, which resulted in an increase in the CD206:iNOS-positive MΦ ratio in the MSC(M)- vs. saline-treated mice [104]. Our data are highly supportive of an anti-inflammatory effect of MSC(M) and interactions with local MΦs in the articular joint to modulate them to more pro-resolving subtypes. Interestingly, Schelbergen et al. showed in mouse models that the reparative effects of MSC(AT) were limited to inflammatory models of OA, namely, collagenase-induced OA (CIOA), but not in the post-traumatic surgical injury and destabilization of the medial meniscus (DMM) model [105]. Additionally, they found that MSC(AT) were most effective in mice with high synovitis scores and systemic inflammation, as evidenced by serum levels of S100A8/9. A follow-up study by van Dalen et al. showed that polymorphonuclear cells (PMNs) form clusters around MSC(AT) injected in the CIOA mouse joint and that this may be mediated by IL-1β priming, which upregulates MSC(AT) expression of chemotactic factors and enhances PMN phagocytic activity in coculture experiments [106]. These observations challenge the utility of the well-accepted DMM model for measuring MSC-mediated cartilage reparative effects and support the important role of the immunomodulatory mechanisms of MSCs in OA models.
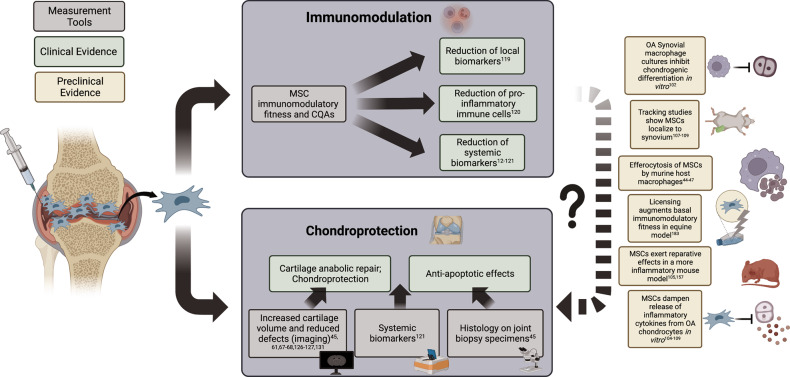
Cell tracking studies in equine [107] and ovine [108, 109] OA models demonstrate that autologous and allogeneic MSCs can persist within the joint for the duration of study periods ranging from 8–14 weeks postinjection. Notably, these studies have shown that injected MSCs home to the synovium rather than to cartilage [107–109], supporting MSC modulation of synovial inflammation as a primary therapeutic target in OA. Feng et al. [109] used allogeneic MSC(AT) labeled with superparamagnetic iron oxide (SPIO) combined with HA to observe MSC localization primarily to the synovium, particularly around synovial CD68+ macrophages. In this ovine OA model, the levels of the inflammatory factors TNF-α and IL-6 in the synovial fluid of the MSC(AT) + HA-treated group were significantly lower than those in the control groups; concomitantly, these groups also showed significantly thicker cartilage of the tibial plateau relative to controls [109]. Barrachina et al. [110] used an equine model to show that MSC(M) in chemically (amphotericin)-induced OA significantly reduced inflammatory markers via histopathological analysis of the synovium at both 2 and 6 months. Subsequently, both unprimed MSC(M) and MSC(M) primed with IFNy and TNF-α (to enhance the basal immunomodulatory fitness of the cells) resulted in delayed cartilage degeneration. However, the MSC(M)-primed group showed an anabolic response via an upregulation of collagen type II (COL2), aggrecan (ACAN) and cartilage oligomeric matrix protein (COMP) gene expression. Although both MSC(M) treatment groups showed similar macroscopic cartilage appearances, the differential gene expression suggests higher quality tissue remodeling due to MSC priming with proinflammatory cytokines, supportive of primary MSC immunomodulatory functionality. Moreover, canine MSC(AT) genetically modified to overexpress the pleiotropic growth factor platelet-derived growth factor (PDGF) or antioxidant factor heme-oxygenase 1 (HO-1) showed improvements in pain and lameness scores in PDGF-MSC(AT)-treated but not HO-1 MSC(AT)-treated beagles with cranial cruciate ligament transection, which mimics posttraumatic OA [111]. Notably, the expression of tissue inhibitor of metalloproteinases was significantly upregulated, effectively reducing catabolic MMP-13 and nerve growth factor. Furthermore, an increase in collagen type 2 was observed in canine chondrocytes [112]. Taken together, the in vitro and preclinical data support the chondroprotective and tissue remodeling effects mediated by MSCs in parallel to or secondary to primary immunomodulatory and anti-inflammatory effects, visualized in Fig. 2.
Fig. 2.
Clinical and preclinical evidence of mesenchymal stromal cell mechanisms of action on immunomodulation and chondroprotection in knee osteoarthritis. Solid arrows are used to demonstrate mechanisms for which there is supporting clinical evidence: dashed arrows indicate the relationship between immunomodulatory and chondroprotective mechanisms supported by preclinical evidence. MSC mesenchymal stromal cell, CQAs critical quality attributes, OA osteoarthritis
Now, it should be noted that the role of inflammation in OA is not fully understood, and it is unclear whether inflammation represents a primary etiology of the disease or whether it arises secondary to other processes, such as joint damage and altered mechanical signaling within the cartilage [113]. Moreover, the inflammatory landscape of OA appears to be distinct from that of other arthritides, and the levels of classical Th1 cytokines such as TNF-α and IL-1, which are prevalent in RA, are present at very low levels in the synovial fluid of OA patients [114]. Indeed, the level of inflammation in OA may vary temporally, and it has been posited as a distinguishing feature for OA patient endotype, as discussed below [115]. In the context of MSC therapies, an improved understanding of inflammatory features and their temporal kinetics may be crucial given that inflammatory priming is critical to induce immunomodulatory functions in MSCs [116]. Thus, for MSCs to achieve therapeutic benefit in OA via immunomodulation, it may be important to better delineate inflammatory patient endotypes and/or inflammatory flares using sensitive imaging and/or biomarker evaluations that would enable improved patient selection based on responder likelihood to MSC therapy.
Clinical evidence of MSC immunomodulation in OA
While the findings of preclinical studies (extensively reviewed [117, 118]) support MSC-mediated immunomodulation in OA as an important mechanism of action, clinical evidence has thus far been limited. In a twelve-patient Phase I/IIa knee OA clinical trial with autologous MSC(M) injections, our group provided the first clinical evidence to demonstrate that MSCs modulate inflammation within the OA joint [119]. We observed a significant reduction in synovial fluid levels of the proinflammatory cytokine IL12p40 at 3 months relative to baseline along with a trend toward reduced levels of the intermediate CD14+CD16+ MΦs [119]. In parallel, we noted significant improvements in KOOS pain, symptom, and quality of life and WOMAC stiffness subscale scores relative to baseline [119].
Systemic and local levels of inflammatory biomarkers after intra-articular MSC injections have also been investigated in recent knee OA trials. A study by Li et al. demonstrated systemic anti-inflammatory effects of MSC(M) injections and platelet lysate (three monthly injections with MSCs and platelet lysate injected three days apart) relative to arthroscopic debridement and HA injections in knee OA patients (KL grade 0–2, N = 40–46/group); significant reductions in serum TNF-α and IL-6 were noted within the MSC(M)-treated group at 6 and 12 months relative to baseline and to the HA controls [120]. In a three-patient study, Sadri et al. also reported a trend toward decreased serum IL-6 and transiently increased IL-10 in knee OA patients (KL grade 2–3) receiving allogeneic MSC(AT), albeit with a limited sample size and no statistical testing [121].
In contrast to the above, Bastos et al. have shown that there were no significant differences in synovial fluid levels of various inflammatory cytokines (IL-17A, IFN-γ, TNF -α, IL-10, IL-6, IL-4, and IL-2) between knee OA (KL grade 1–4) patient groups treated with autologous MSC(M) (40 × 106 fresh cells), autologous MSC(M) plus autologous PRP, or corticosteroids at 6 and 12 months after treatment (N = 10–13/group) [62]. Notably, the authors detected significant reductions in the levels of the anti-inflammatory cytokine IL-10 at 12 months relative to baseline in all three groups, which the authors postulated may be related to a resolution of inflammation across groups due to a potential compensatory role of IL-10 in the inflammatory context of OA [62]. Nonetheless, the MSC injections may have effected immunomodulatory changes at earlier timepoints that were missed upon synovial fluid collection at 6 months. Indeed, in our previous knee OA clinical trial with autologous MSC(M), we probed inflammatory changes within the synovial fluid at baseline and 3 months to detect earlier changes in joint inflammation that coincided with maximal improvements in patient pain, symptoms and function [119].
Clinical evidence of chondroprotection and cartilage repair
To date, most OA clinical trials investigating disease modification by MSC therapeutics have focused on cartilage changes, given that cartilage degradation is a hallmark of OA, as well as a history of regulatory bodies emphasizing the need for structural changes to achieve therapeutic effects in OA [122]. Altogether, we identified 21 clinical studies (Table 2) that provided evidence of chondroprotective or cartilage regenerative effects of intra-articular MSC injections in knee OA, including through imaging modalities, second-look arthroscopy, analysis of cartilage tissue biopsies, and the measurement of biomarkers for cartilage breakdown in serum, plasma and urine. While these effects are promising, it should be noted that these observations provide little insight into the true mechanisms of action given that MSCs can modulate the joint microenvironment through interactions with a variety of cell types within the joint, including chondrocytes and other cells. As noted above, these effects may occur downstream of MSC-mediated immunomodulation in the OA joint, as demonstrated by Fahy et al. and others in vitro [110, 117, 118]; further research is needed to delineate the interrelationships among these mechanisms of action. While most published studies investigating cartilage repair have suggested regenerative (14/21 or 66%) or chondroprotective (4/21 or 20%) effects of MSC injections, several others (3/21 or 14%) have not detected improvements in cartilage volume or integrity. Moreover, a meta-analysis of five published clinical studies reported that the quality of evidence for MSC-mediated chondroprotection or regeneration was limited, pointing to the need for additional higher powered and well-controlled studies [83]. Insights into chondroprotection and regeneration have primarily relied on MRI measurements, which are associated with several limitations, including a lack of sensitivity and a standardized methodology for MRI measurements and analyses. Importantly, previous work has shown that the relationship between cartilage structural changes and patient pain or other symptoms is complex and not necessarily correlative (reviewed in [123–125]), suggesting that chondroprotection and regenerative effects may not map onto patient clinical responses. Nonetheless, we review clinical studies evaluating the regenerative and chondroprotective effects of intra-articular MSC injections, as these provide useful evidence for the potential disease-modifying effects of MSCs within the OA joint.
Table 2.
Clinical effects of culture-expanded mesenchymal stromal cell injections on knee OA cartilage
| Author | MSC tissue source | Cell dose (x106 cells) | Treatment group intervention | Comparison (baseline or control) | Number treated | Cartilage outcome measures | Time points | Cartilage outcomes |
|---|---|---|---|---|---|---|---|---|
| Autologous | ||||||||
| Jo et al. [45] | AT | 10, 50, 100 | sIA injection of MSC | Baseline |
12 (100 × 106 dose); 3 (50 × 106 dose); 3 (10 × 106 dose) |
MRI (volume, defect size), Arthroscopy, Histology (Col I, Col II, SafO), X-ray (KL, JSW) |
0, 3, 6 months (MRI, X-ray); 0, 6 months (arthroscopy, histology) |
Regeneration favouring high-dose group by MRI, arthroscopy, histology |
| Lamo-Espinosa et al. [60] | M | 10, 100 | sIA injection of MSC + 60 mg HA | Baseline, 60 mg HA control |
10 (100 × 106 dose); 10 (10 × 106 dose); 10 (control) |
MRI (WORMS), X-ray (JSW) | 0, 6, 12 months | Possible regeneration favouring high-dose group by X-ray and MRI |
| Freitag et al. [58] | AT | 100 | sIA injection of MSC ± second injection at 6 months | Baseline, conservative management control, and dose groups |
10 (single dose); 10 (two doses); 10 (control) |
MRI (MOAKS) | 0, 12 months | Chondroprotection favouring two-dose group |
| Lamo-Espinosa et al. [59] | M | 100 | IA injections of MSC at 0, 1, and 2 weeks + 8 mL PRP | Baseline, PRP only control |
30 (MSC+PRP); 30 (control) |
MRI (WORMS), X-ray (JSW) | 0, 12 months | No significant effects |
| Lee et al. [57] | AT | 100 | sIA injection of MSC | Baseline, 3 mL saline (vehicle) control |
12 (MSC group); 12 (control) |
MRI (volume, defect size), X-ray (KL, JSW, HKA) | 0, 6 months | Chondroprotection; significant increase in defect size observed in saline- but not MSC-treated group by MRI |
| Song et al. [126] | AT | 10, 20, 50 | Bilateral IA injections of MSC at 0, 3 weeks ± third injection at 48 weeks | Baseline | 6/dose group | MRI (volume) | 0, 12, 24, 48, 72, 96 weeks | Regeneration favouring high-dose group with subsequent reduction in cartilage volume at 96 weeks |
| Chahal et al. [119] | M | 1, 10, 50 | sIA injection of MSC | Baseline |
4 (50 × 106 dose); 4 (10 × 106 dose); 4 (1 × 106 dose) |
MRI (T2, WORMS), ELISA (HA, COMP, C1–2C, C2C, CTXII) |
0, 6, 12 months (MRI); 2, 6, 12, 24, and 48 week (ELISA) |
Possible chondroprotection; no changes by MRI but catabolic biomarkers were significantly reduced and favoured high-dose group |
| Chen et al. [127] | AT | 50 | sIA injection of MSC | Baseline | 12 | MRI (MOAKS), X-ray (KL, JSW) | 0, 48 weeks | Regeneration indicated by reduced MOAKs articular cartilage pathology scores |
| Lu et al. [61] | AT | 50 | Bilateral IA injections at 0 and 3 weeks | Baseline, 25 mg HA control | 26/group | MRI (volume) | 0, 24, 48 weeks | Regeneration in MSC group with degeneration in HA group |
| Orozco et al. [128] | M | 40 | sIA injection of MSC | Baseline | 12 | MRI (T2, PCI) | 0, 6, 12 months | Regeneration indicated by significant reduction in PCI scores at 6 and 12 months |
| Rich et al. [129] | M | 40 | sIA injection of MSC | Baseline | 50 | MRI (T2, PCI) | 0, 12 months | Regeneration indicated by significant reduction in T2 values |
| Soler et al. [130] | M | 40 | sIA injection of MSC | Baseline | 15 | MRI (T2, PCI) | 0, 6, 12 months | Regeneration indicated by significant reduction in T2 values at 6 and 12 months |
| Al-Najar et al. [131] | M | 30.5 | IA injection of MSC at 0 and 1 month | Baseline | 13 | MRI (thickness) | 0, 6, 12 months | Regeneration indicated by increased cartilage thickness at 12 months |
| Allogeneic | ||||||||
| Gupta et al. [65] | M | 25, 50, 75, 150 | sIA injection of MSC + 20 mg HA | Baseline, vehicle + HA control |
10 (for each MSC dose); 20 (control) |
MRI (WORMS), X-ray (unspecified parameters) |
0, 6, 12 months (MRI); 0, 3, 6 months (X-ray) |
No significant effects |
| Sadri et al. [121] | AT | 100 | sIA injection of MSC | Baseline | 3 | MRI (thickness, volume), ELISA (COMP, HA, CTX-II, MMP-3) |
0, 6 months (MRI); 0, 1 week, 1, 3, 6 months |
Possible chondroprotection and regeneration by MRI and ELISA but small sample size |
| Soltani et al. [67] | Placenta | 50–60 | sIA injection of MSC | Baseline, saline control |
10 (MSC); 10 (control) |
MRA (thickness) | 0, 24 weeks | Regeneration indicated by increased cartilage thickness relative to baseline in MSC but not control group |
| Zhao et al. [132] and Lu et al. [133] | AT | 10, 20, 50 | Bilateral IA injections at 0 and 3 weeks | Baseline |
7 (10 × 106 group); 8 (20 × 106 group); 7 (50 × 106 group) |
MRI (volume, WORMS, T1rho, T2, T2star, R2 star, ADC, FA) | 0, 48 weeks | Regeneration favouring high-dose group |
| Vega et al. [68] | M | 40 | sIA injection of MSC | Baseline, 60 mg HA control |
15 (MSC group); 15 (control) |
MRI (T2, PCI) | 0, 6, 12 months | Regeneration indicated by improved PCI in MSC(M)-treated patients relative to HA at 12 months |
| Matas et al. [69] | WJ | 20 | sIA injection of MSC ± second injection at 6 months | Baseline, 60 mg HA control |
10 (single dose); 10 (two doses); 8 (control) |
MRI (WORMS) | 0, 6, 12 months | No significant effects |
| Park et al. [134] | CB | 11.5–20 | Implantation of HA hydrogel containing MSC(WJ) | Baseline | 6 | MRI (dGEMRIC ΔR1), Arthroscopy, Histology (Col II, SafO) |
0, 3 years (MRI); 0, 12 weeks, 12 months (arthroscopy, histology) |
Possible regeneration but small sample sizes |
| Kuah et al. [70] | AT | 3.9, 6.7 | sIA injection of MSC + cell supernatant | Baseline, control group treated with cell supernatant and vehicle only |
8 (3.9 × 106 dose); 8 (6.7 × 106 dose); 4 (control) |
MRI (volume, MOAKS), ELISA (C2C, CTXII, HA, CTX-I) | 0, 12 months | Chondroprotection within the low-dose group relative to high-dose and control group by MRI but not biomarkers |
M bone marrow, AT adipose tissue, WJ Wharton’s jelly, CB cord blood, sIA single intra-articular injection, HA hyaluronic acid, PRP platelet-rich plasma, MRI magnetic resonance imaging, MOAKS MRI Osteoarthritis Knee Score, MOCART magnetic resonance observation cartilage repair tissue, WORMS whole-organ magnetic resonance imaging score, ADC apparent diffusion coefficient, FA fractional anisotropy, KL Kellgren-Lawrence classification of osteoarthritis, JSW joint space width, HKA hip-knee angle, SafO safranin O, MSC mesenchymal stromal cell, MRA Magnetic resonance arthrogram, dGEMRIC delayed gadolinium-enhanced MRI of cartilage, COL1 collagen type I, COL2 collagen type II, COMP cartilage oligomeric matrix protein, C1-2C C1-2C collagen type I and II cleavage, C2C collagen type II cleavage, CTX-I C‐telopeptide of type II collagen, CTX-II C‐telopeptide of type II collagen, MMP-3 matrix metalloproteinase 3
The findings of studies involving the use of autologous MSCs have generally supported the cartilage reparative effects of MSCs, and these studies have included MSCs derived from either adipose tissue or bone marrow. For studies investigating autologous MSC(AT), doses range from 10 × 106 to 100 × 106 cells with single or multiple injections. A dose comparison study by Jo et al. using intra‐articular injections of autologous MSC(AT) reported a significantly increased cartilage volume and reduced size of cartilage defects in the medial femoral and tibial condyles of knee OA (KL grade 2–4) patients at 6 months after injection within their high-dose (100 × 106 cells, N = 12 patients) but not lower-dose (10 × 106 cells, N = 3) or moderate-dose (50 × 106 cells, N = 3) groups [45]. The authors also showed through arthroscopic and histological assessment at baseline and 6 months the presence of regenerated cartilage and reduced cartilage defects [45]. However, in a follow-up Phase IIb RCT from the same investigators, more modest effects on cartilage were reported when comparing only the high-dose (100 × 106 fresh cells) group vs. saline-treated controls (N = 12/group, KL grade 2–4); autologous MSC(AT) injections had no significant effect on the change in the size of cartilage defects at 6 months relative to baseline by MRI, while patients in the saline control group displayed significant exacerbations of cartilage defects, suggesting a chondroprotective but not a regenerative effect of the MSC(AT) [57]. Using the same dose of 100 × 106 autologous MSC(AT) but with cryopreserved cells, Freitag et al. compared single versus two injections of autologous MSC(AT) (doses 6 months apart, KL grades 2–3) to conservative management control treatment (N = 10/group), reporting improved chondroprotection for the two-dose group relative to the single-dose and control groups at 12 months after injection as measured using the semiquantitative MRI Osteoarthritis Knee Score (MOAKS; a semiquantitative and subregional scoring system) method [58].
Regenerative effects of autologous MSC(AT) have also been reported at moderate doses. A dose comparison study investigating bilateral repeat injections of autologous MSC(AT) within both knee joints (10, 20 or 50 × 106 cells/dose at 0, 3 and 48 weeks, KL grade 2–3; N = 4–5/group) showed increases in cartilage volume up to 72 weeks relative to baseline that favored the 50 × 106 dose [126]. Interestingly, a subsequent decrease in cartilage volume was observed at 96 weeks (approx. 22 months) after injection [126], suggesting that regenerative effects may have been transient and emphasizing the importance of long-term follow-ups. A similar approach was used to evaluate bilateral repeat injections of autologous MSC(AT) (50 × 106 cells/dose at 0 and 3 weeks; KL grade 2–3) relative to an HA control treatment (N = 26/group), reporting significantly increased cartilage volume at 48 weeks within the MSC(AT)-treated group, while cartilage degeneration was observed within the HA-treated group [61]. At the same dose level, Chen et al. showed that intra-articular injections (50 × 106 cryopreserved cells) in knee OA (KL grade 2–3, N = 12) significantly improved articular cartilage pathology and several other MOAKS metrics at 48 weeks relative to baseline, including improvements in the overall MOAKS and bone marrow lesions, while no significant changes in the joint space height as measured by X-ray were detected [127]. Taken together, these data suggest that moderate to higher doses (≥50 × 106 cells) of autologous MSC(AT) delivered through single or repeat injections can effect measurable cartilage repair changes, at least over shorter durations of 6–12 months. Longer studies are rare, but their findings suggest the absence of sustained cartilage reparative effects, which merits further investigation.
Dose ranges for studies investigating autologous MSC(M) are similar to those for studies on MSC(AT) but with a slightly wider range of 1 × 106—100 × 106 cells with single or repeat injections, as well as the use of combination strategies involving surgical interventions or delivery of HA or PRP. As detailed in the RCT section above, Lamo-Espinosa et al. compared single-dose intra-articular injection of MSC(M) combined with HA injection (10 × 106 and 100 × 106 fresh cell dosage groups) relative to HA injection alone (N = 10 patients/group) in knee OA patients (KL grade 2–4) and reported modest chondroprotective effects that favored a high dose, as evidenced by X-ray at 6 and 12 months showing a reduction in the knee articular interline within the HA group that was significant at 12 months, while no degenerative changes were observed in the MSC(M) treatment groups [60]. However, the same group administered three weekly doses of a combination product including autologous PRP with or without autologous MSC(M) (100 × 106 fresh cells/dose, N = 30/group, KL grade 2–4) in a RCT and showed no significant effects on cartilage volume changes as evaluated by X-ray and the MRI WORMS protocol at 12 months after injection [60]. Other clinical trials conducted by this group in Spain have reported regenerative effects of single injections of autologous MSC(M) at moderate doses (40 × 106 fresh cells) with significant improvements in cartilage quality for knee OA patients (KL grade 2–4) by T2 relaxation times (an MRI metric used to evaluate cartilage quality that is sensitive to water content and collagen fibril organization) and the poor cartilage index (PCI, an estimate of the percentage of T2 values above 50 ms) at 12 months relative to baseline [128–130]. Regenerative effects have also been reported by Al-Najar et al. using two intra-articular injections of autologous MSC(M) (at comparable doses of 30.5 × 106 fresh cells/dose, 1 month apart, N = 13) in knee OA patients (KL grade 2–3), showing significant increases in cartilage thickness by T2 mapping at 12 but not 6 months after the first injection relative to baseline [131]. Work from our group has shown more modest effects of autologous MSC(M) on knee cartilage. In knee OA patients (KL grade 3–4) administered a single intra-articular injection of autologous MSC(M) (1 × 106, 10 × 106, 50 × 106 cells, N = 4/group), we observed no changes in WORMS or T2 relaxation times at 6 and 12 months after injection relative to baseline for any cell dosage groups [119], including the high-dose group, which was comparable in magnitude to that in the Spanish studies. However, an analysis of cartilage breakdown byproducts by general estimating equations (GEEs) showed a significant decrease in the levels of serum C1‐2C in the 50 × 106 cell dose group relative to the 1 × 106 and 10 × 106 cell dose groups [119]. Overall, the findings of clinical trials involving autologous MSC(M) indicate possible chondroprotective and regenerative effects and suggest that moderate-to-higher dose (≥40 × 106 cells) single-injection autologous MSC(M), speaking to the basal fitness of autologous MSCs from OA patients or lower doses that are repeated or combined with other interventions, have measurable effects on cartilage. The evaluation of serum and urine biomarkers of cartilage breakdown products may be more sensitive than MRI evaluations of cartilage integrity, but a combinatorial approach is likely needed to understand all effects.
Using allogeneic MSCs, mixed effects of intra-articular injections on OA cartilage have been reported, and this may be related to greater use of cryopreserved cells, the use of other MSC tissue sources that have been less studied in the context of OA clinical trials, the use of combined interventions and an overall fewer number of allogeneic trials, all of which complicate interpretations. In a RCT, Soltani et al. showed regenerative effects of allogeneic placenta-derived MSCs (50–60 × 106 fresh cells), as evidenced by significantly increased cartilage thickness at 24 weeks relative to baseline in knee OA patients (KL grade 2–4), while no changes were observed with saline vehicle control (N = 10/group) [67]. A RCT by Vega et al. comparing a single-dose intra-articular injection of allogeneic MSC(M) (40 × 106 fresh cells) to HA injection (N = 15/group) in patients with knee OA (KL grade 2–4) also reported regenerative effects on cartilage with significant improvements in cartilage quality by the PCI in the MSC(M) group at 12 months relative to baseline that was not apparent in the HA group [68]. Another trial in which patients with knee OA (KL grade 2–3) received bilateral repeat doses of allogeneic MSC(AT) (10 × 106, 20 × 106, or 50 × 106 cryopreserved cells/dose in both knees at 0 and 3 weeks, N = 7–8/group) also showed improvements in cartilage volume and integrity by MRI across dosage groups at 48 weeks relative to baseline [132, 133]. Using multiparametric MRI measurements (including WORMS, T2, and other metrics), the authors reported that T1rho measurements (estimating glycosaminoglycan (GAG) and proteoglycan content) were the most sensitive for detecting differences between dose groups, with the high-dose group showing significantly greater increases in T1rho values [132]. In contrast to these studies, a RCT by Matas et al. comparing single and two doses of MSC(WJ) (20 × 106 fresh cells/dose, with a second dose at 6 months for the two-dose group) to HA injection (N = 8–10/group) in knee OA patients (KL grade 1–3) showed no detectable changes in MRI WORMS measured at 6 and 12 months after injection [69].
Allogeneic MSCs have also been investigated in combination with other injectables. Using cryopreserved allogeneic MSC(AT) and cell culture supernatant containing MSC-secreted factors and EVs, Kuah et al. reported evidence of chondroprotection in a RCT with knee OA patients (KL grade 1–3); patients receiving the low-dose cell product (3.9 × 106 cryopreserved cells, N = 8) showed no reduction in cartilage volume, while significant reductions were observed in both the high-dose (6.7 × 106 cryopreserved cells, N = 8) and control (cell culture media and cryopreserved cells, N = 4) groups at 12 months relative to baseline [70]. Notably, the authors reported no changes in serum or urine levels of cartilage catabolic biomarkers (C2C, CTX-II, HA, and CTX-I) [70], which contrasts with findings from our previous study showing reductions in catabolic biomarkers but no detectable cartilage volume changes by MRI [119]. A RCT by Gupta et al. in which knee OA patients (KL grade 2–3) were administered cryopreserved allogeneic MSC(M) from pooled donors (25 × 106, 50 × 106, 75 × 106, or 150 × 106 cells/dose in separate cohorts, N = 10/cohort) or vehicle (N = 5/cohort) followed by HA injection demonstrated no effect of the MSC injections on cartilage volumes as assessed by X-ray and MRI WORMS scores relative to baseline or control at 6 and 12 months follow-up [65]. Using an in situ tissue engineering strategy, Park et al. implanted a composite consisting of a HA hydrogel with allogeneic MSC(CB) (0.5 × 107 cells/mL and 500 µl/cm2 of the defect area, N = 6) into cartilage defects for patients with knee OA (KL grade 3) and ICRS grade 4 cartilage lesions [134]. Arthroscopic evaluation of the defects at 12 weeks postimplantation revealed maturing cartilage, and ICRS grades were reduced in 4 out of 6 patients. A subset of two consenting patients at the 1-year follow-up showed hyaline-like cartilage that integrated with the surrounding tissue, along with positive staining with the proteoglycan-binding dye safranin O and cartilage-specific collagen II by biopsy. MRI measurements at the 3-year follow-up (N = 5) also showed increased GAG content at the defect sites relative to baseline using delayed gadolinium‐enhanced MRI of cartilage (dGEMRIC). Notably, the authors reported significant improvements in VAS pain scores and IKDC scores at 6 months relative to baseline that were maintained through 7 years of follow-up in an analysis of a subset of patients without additional knee surgery or replacements [134]. This tissue-engineered product has been commercialized in S. Korea as CARTISTEM™; it is currently in clinical evaluations in the USA (NCT01733186) and Japan.
Taken together, recent data support the regenerative and/or chondroprotective effects of intra-articular MSC injections, especially when injected at moderate to higher doses (≥40 × 106 cells), in repeat doses or when combined with surgical interventions. However, differences in the baseline clinical phenotype of patients, MSC tissue sources, the use of fresh versus cryopreserved cells, and the use of combination strategies involving coinjections with HA or PRP and surgical interventions confound these analyses. Additional high-quality evidence is required with higher powered and well-controlled clinical trials coupled with longer durations of follow-up for evaluating cartilage changes by MRI. Measurements of biomarkers for cartilage degradation in synovial fluid, urine, serum and plasma along with patient clinical phenotyping and endotyping will also provide useful insights into this potential mechanism of action of MSCs in effecting cartilage regeneration and repair in knee OA. Importantly, the reported clinical chondroprotective and regenerative effects of MSCs are observational and may be achieved through several mechanisms. Donor MSCs may directly regulate the endogenous chondrocyte phenotype by modulating their ECM production and promoting cell survival and autophagy via growth factors, microRNAs (miRs), EVs and organelle transfer [135–138]. MSCs may also recruit endogenous progenitors [139] and regulate their differentiation into chondrocytes [140]. Alternatively, MSCs can modulate the joint microenvironment to indirectly promote cartilage repair through interactions with immune cells and other joint tissues, as discussed in the previous subsections. Thus, further study is needed on the multimodal mechanisms of action of MSCs, but these mechanisms are likely to include both direct and indirect effects on cartilage, as previously reviewed [74, 141].
Other potential mechanisms
In addition to having immunomodulatory and chondroprotective effects in OA, MSCs may act through a variety of other mechanisms that target multiple tissues within the joint. These mechanisms include antifibrotic and angiogenic effects, which are interrelated with immunomodulation. In particular, the pro-angiogenic mechanisms of MSCs have been widely documented and are of clinical relevance to a variety of conditions, such as critical limb ischemia [142]. The potential pro-angiogenic effects of MSCs are understudied in OA, but angiogenesis is generally associated with increased inflammation, synovitis, and pain [143]. However, our previous clinical study in knee OA demonstrated a significant increase in levels of the pro-angiogenic factor VEGF in the synovial fluid of OA patients at 3 months relative to baseline after autologous MSC(M) injections, and this was observed in parallel to significant improvements in patient pain and other PROMs, as well as reduced joint inflammation [119]. VEGF has been shown to be associated with catabolic processes in synovial cells and chondrocytes in a mouse surgically induced OA model [144]; however, other pro-angiogenic factors, such as FGF2, which can also be produced by MSCs, may have pleiotropic functions in OA, with FGF2 having dichotomous effects on articular chondrocytes dependent on relative chondrocyte expression of FGFR1 and FGFR3 receptors [145]. Moreover, platelet-rich plasma (PRP), an often used analgesic for joint pain and inflammation, is known to be rich in pro-angiogenic factors, including PDGF isoforms, TGF- a/TGF- b, VEGF, EGF, FGF-a/b, connective tissue growth factor (CTGF), IGF-1, hepatocyte growth factor (HGF), keratinocyte growth factor (KGF) and Ang-1, and yet symptom and pain-relieving effects of PRP injections have been reported in RCTs and in several meta-analyses in knee OA patients [146–148].
There is a complex interplay between inflammatory and angiogenic processes, with immune cells playing a critical role in the temporal regulation of vessel remodeling through both pro- and anti-angiogenic mechanisms [149]. Previous work by Boregowda et al. indicated that the in vitro immunomodulatory and pro-angiogenic properties of human MSC(M) may be inversely correlated and mediated by levels of the transcription factor TWIST1 [150]. The stimulation of MSC(M) with proinflammatory factors increased the immunosuppressive functions of MSC(M) and reduced the levels of TWIST1, while the stimulation of MSC(M) with pro-angiogenic factors had the opposite effect [150]. In support of this, we have separately shown that lower levels of several angiogenic factors inversely correlated with the immunomodulatory fitness of human MSC(AT), as evaluated by in vitro monocyte/macrophage polarization toward inflammation-resolving phenotypes [91]. Thus, it is possible that the immunomodulatory properties of MSCs may predominate over the angiogenic properties, and this could be mediated by proinflammatory cues within the joint microenvironment in knee OA; however, this is speculative, and there is likely a complex interplay between inflammatory and angiogenic processes mediated by MSCs for which further study in an OA context is needed.
Antifibrotic effects of MSC therapies have been documented in several clinical indications for which fibrosis is a disease hallmark, including for idiopathic pulmonary fibrosis [151] and ischemic cardiomyopathy [152]; thus, antifibrotic functions represent a possible mechanism of action for MSCs in OA. Fibrotic tissue in the synovium and cartilage is marked by synovial hyperplasia and fibrocartilage formation, respectively, which modulate the disease tissue microenvironment and cellular phenotypes within the OA joint [153]. Importantly, a complex interplay exists among tissue fibrosis, inflammation, and angiogenesis, and MSCs can modulate immune cells and augment neovascularization to remodel fibrotic tissue, as we discussed in a previous review [154]. While reduced synovial hyperplasia has been shown in preclinical OA studies evaluating MSC treatment [105, 155], more research is needed to understand whether MSCs may exert direct antifibrotic effects on OA or whether this is achieved indirectly through MSC-mediated immunomodulation or angiogenesis.
In addition to the immunomodulatory, angiogenic, and antifibrotic properties of MSCs that may impact multiple tissues within the joint, MSCs may have tissue-specific effects on the subchondral bone, menisci, and ligaments. MRI data on these tissues from clinical studies involving MSCs in OA are sparse and limited by the sensitivity of the technique. However, Chen et al. have shown that autologous MSC(AT) injection significantly reduced the MOAKS for bone marrow lesions and cysts, meniscus pathology, and periarticular features at 48 weeks relative to baseline, while no significant differences were observed for osteophyte, synovitis, ligament tears or tendon abnormality scores [127]. In terms of subchondral bone, MSCs can interact with osteoclasts in OA through direct cell‒cell contact and indirectly through secreted factors and EVs to inhibit osteoclastogenesis and subchondral bone resorption, as recently reviewed [156]. Osteoblasts are also known to modulate cartilage metabolism and subchondral bone remodeling in OA, and a previous in vitro study demonstrated that EVs derived from human MSC(AT) reduced OA osteoblast senescence and the release of inflammatory mediators such as IL-6 [157].
The menisci and ligaments of the joint play important roles in mechanical support, and damage to these tissues can precede radiographic OA; however, their roles in OA progression and pathophysiology are poorly understood [158]. A recent study by Ramos-Mucci et al. demonstrated that the ligaments and menisci undergo structural changes, including increased mineralization and chondrogenesis, in both a spontaneous and surgically induced OA model [159]. MSCs are being investigated for meniscal and ligament repair due to their chondroprotective and immunomodulatory properties [160, 161], and thus, the joint menisci and ligaments represent possible additional target tissues for MSC mechanisms of action in OA that merit further study.
Influence of MSC immunomodulatory basal fitness on their mechanisms of action
Several factors can influence the fitness and overall phenotype of MSCs that may in turn influence their mechanisms of action, as discussed here with emphasis on effects mediating immunomodulatory fitness. Donor heterogeneity represents a major variable and includes a multitude of factors, such as donor health status, age, BMI and sex, that can influence the in vitro clonogenic potential, paracrine functions, and proclivity toward senescence of MSCs [162–165]. We have been investigating the interactions between donor heterogeneity and the optimization of culture variables to culture-expand MSC(M) while maintaining their immunomodulatory functionality and have shown that donor heterogeneity is an important variable for a subset of donors; surrogate gene readouts are also being developed to prospectively identify these donors (Kolade et al., manuscript in preparation). Tissue procurement, isolation and manufacturing strategies for MSCs are also factors that modulate MSC behavior [166, 167]. MSC donor fitness is typically minimally investigated by evaluating cell viability, proliferation and trilineage differentiation; these parameters are often separate from the actual clinical mechanisms of action in OA and thus provide limited insights into the true fitness of MSCs prior to intra-articular injection. More rigorous assessments, as we have recently proposed [91], are needed to better understand and evaluate basal MSC donor fitness [168]. The level of expansion for MSCs should also be carefully monitored, as transcriptome drift has been reported to precede changes in growth kinetics and other hallmarks of senescence for human MSC(WJ) [169].
In support of the immunomodulatory mechanism of action of MSCs in OA, we and others have investigated the relationships between the baseline immunomodulatory fitness of donor MSCs in vitro and their clinical efficacy. In our clinical trial, we measured the levels of IFN‐γ-induced expression of immunomodulatory genes (prostaglandin-endoperoxide synthase 2, PTGS2; cluster of differentiation 274, CD274; indoleamine 2,3-dioxygenase 1 IDO1; interleukin-10, IL10; hepatocyte growth factor, HGF; and transforming growth factor beta 1, TGFB1) and TNF-α-induced TSG6 protein expression by MSC(M) in vitro and found correlations with changes in WOMAC and KOOS scores [69]. These data suggest that MSC(M) with higher baseline immunomodulatory fitness levels in vitro afforded improved patient outcomes, thus supporting immunomodulatory functionality as a clinically relevant mechanism of action for MSC(M). In support of these findings, Chen et al. showed that the levels of intracellular IDO protein expression in IFN‐γ-stimulated MSC(AT) in vitro were significantly correlated with in vitro suppression of T-cell proliferation as well as improvements in KOOS sports, VAS and IKDC scores in OA patients receiving intra-articular injections of MSC(AT) [127]. Notably, while the findings of both studies [119, 127] support an immunomodulatory mechanism of action of MSCs in OA, neither study found changes in synovitis scores by MRI [119, 127], pointing to the relative insensitivity of MRI in detecting changes in synovial inflammation, at least over shorter time intervals [127]. Matas et al. have also reported the measurement of secreted thrombospondin-2 to select MSC(WJ) donors in their RCT for OA, citing the role of thrombospondin-2 in regulating chondrogenic differentiation [69]. Interestingly, thrombospondin-2 has also been shown to exert anti-inflammatory effects in rheumatoid arthritis models [170], suggesting that the MSC(WJ) used in Matas et al. may also have exhibited augmented immunomodulatory fitness, at least in vitro.
Delivery strategies are also likely to influence mechanisms of action, and the administration of freshly thawed cryopreserved MSCs can influence their cell viability and apoptotic status [171] and diminish their immunosuppressive capacity [172]. Cryopreservation also influences cell membrane integrity, which in turn facilitates complement binding and subsequent innate effector cell recognition [173]. Evidence from Antebi et al. demonstrated that 24-h in vitro culture post-thaw provided sufficient recovery time for human MSC(M) to regain the expression of angiogenic and anti-inflammatory genes as well as in vitro T-cell immunosuppression [174]. Interestingly, the application of MSC(CB) commercialized by MEDIPOST as CARTISTEM® for the treatment of degenerative arthritis includes a culture-rescue period in the final passage prior to surgical implantation to treat cartilage defects [175]. Nonetheless, positive effects on PROMs and cartilage repair have been reported using both cryopreserved and fresh or culture-rescued cells, although these have not been directly compared in OA clinical trials. While fresh low-passage MSCs may be expected to have higher baseline therapeutic fitness, there are conflicting preclinical data, and the interplay between the combinatorial effects of fresh/frozen status, freeze/thaw methods, and other manufacturing or donor-specific variables collectively influences disease-specific mechanisms of action and overall treatment efficacy, as has been recently reviewed [173].
The tissue sources for MSCs represent an important variable that could also influence MSC mechanisms of action. To date, bone marrow, adipose tissue and umbilical tissues represent the most commonly used MSC sources in OA clinical trials. An elegant study by Ménard et al. investigated matched human MSC(AT) and MSC(M) from 14 donors and demonstrated distinct transcriptional profiles that were imprinted by the tissue of origin in each MSC population, with different sets of immunomodulatory genes and chemokines upregulated in MSC(AT) and MSC(M). MSC(AT) displayed reduced HLADR expression, as well as augmented neutrophil recruitment and suppression of T-cell proliferation in vitro, whereas MSC(M) were better able to suppress natural killer (NK) cell proliferation in experiments with paired donors [176]. Binch et al. also investigated the responses of donor-matched MSC(M) and MSC(AT) to proinflammatory cytokine stimulation and hypoxia, reporting that MSC(AT) upregulated angiogenic and neurotrophic factors under hypoxic and proinflammatory conditions relative to MSC(M) [177]. The findings from these studies using donor-matched MSCs from multiple tissue sources offer important insights into the effects of the tissue of origin on the functional properties of MSCs. While cord blood and Wharton’s jelly also represent common MSC sources, the fetal origin of MSC(CB) and MSC(WJ) prevents donor-matched comparisons to MSC(M) or MSC(AT). Nonetheless, several studies have compared the gene expression profiles and immunomodulatory properties of MSC(AT), MSC(M), MSC(CB), and MSC(WJ) from different donor populations [178, 179], but the optimal tissue source in the context of OA remains unclear and may be dependent on individual donor and manufacturing parameters. Furthermore, there are limited clinical data in OA to draw reliable conclusions on the most suitable tissue source for MSC procurement. Indeed, meta-analyses comparing MSC(M) and MSC(AT) have reached conflicting conclusions, with the findings of one study supporting the improved clinical efficacy of MSC(M) [78], while the findings of other studies support MSC(AT) [81, 180, 181]. Thus, additional research is needed to investigate tissue-dependent effects on MSC treatment efficacy.
The choice of autologous versus allogeneic MSCs is another factor that may impact mechanisms of action. An advantage of allogeneic MSC sources is that they offer the ability to select healthy donors and screen for MSCs with high fitness levels, as we have postulated [91]; we also noted significant donor-driven heterogeneity that correlated with clinical effectiveness [119] (Robb et al., manuscript in preparation). MSCs from allogeneic sources can be expanded in large quantities to treat multiple patients and used off-the-shelf, reducing the cost of manufacturing in an industry driven by cost margins [182]. However, immune recognition is a consideration for the use of allogeneic MSCs for which further study in OA is needed, especially for repeat injections and at higher cell doses. Equine studies have documented alloantibody production in serum after intra-articular injection of allogeneic MSCs, including in a chemically induced OA model where lower antibody responses were observed in half-matched haplotype donors and in proinflammatory cytokine-primed MSC(M) relative to mismatched naïve MSC(M) after a second injection [183], and in healthy joints where cytotoxic antibodies were observed in response to allogeneic but not autologous synovial membrane-derived MSCs [184]. A RCT by Wang et al. reported alloantibody detection in anterior cruciate ligament (ACL) injury patients who underwent ACL reconstruction followed by intra-articular injection of the allogeneic MSC(M) Mesoblast product (single injection, 75 × 106 cryopreserved cells) combined with HA injection. However, significant improvements in KOOS and 36-item Short Form Survey (SF-36) scores and reduced joint space narrowing were observed in the MSC(M)+HA group relative to the HA alone group, suggesting that allorecognition did not preclude treatment efficacy in this study [185]. To our knowledge, clinical data on alloantibody production against MSCs have not been reported in OA; indeed, improved efficacy of repeat versus single injection of allogeneic MSC(WJ) has been reported [69]. The study by Gupta et al. using a single injection of allogeneic MSC(M) from pooled donors (Stempeucel®) also showed greater albeit nonsignificant improvements in PROMs at lower doses relative to moderate and high doses [65]. While not tracked in either of these studies, alloantibodies may have been produced; however, further research is needed to understand whether these may have adverse effects on patient outcomes or side effects for consideration of repeat injection, dosing and use of pooled allogeneic versus single MSC donors. [183], and in healthy joints, where cytotoxic antibodies were observed in response to allogeneic but not autologous synovial membrane-derived MSCs [184].
In contrast, autologous sourcing would circumvent alloantibody production, but donor site morbidity and variable basal MSC therapeutic fitness, which can be impacted by donor factors including age, sex, BMI, physical activity and health status, must be factored in with its use. For example, MSCs obtained from older donors may be more prone to senescence, which may limit the cell numbers required for specific dosing, skew their secretory phenotype and diminish their functional immunomodulatory properties [186]. Thus, autologous MSC treatment efficacy could be limited to individuals for whom adequate doses of potent autologous MSC products can be obtained. Other strategies to enhance “nonfit” autologous MSCs may also be considered, including in vitro priming with exogenous cytokines [187], hormones, growth factors, or senolytic agents, as well as modulating matrix mechanics, oxygen tension, and the use of 3D culture formats [167, 188]. Genetic engineering approaches may also be considered to enhance MSC potency, including revitalizing the paracrine functionality of culture-expanded MSCs through transduction with a cocktail of transcription factors, as reported by Nakahara et al. [189].
Summary of current knowledge on MSC mechanisms of action in OA
There is limited clinical evidence on MSC mechanisms of action in OA. Recent clinical data have supported immunomodulation as a relevant mechanism of action for MSCs in OA [119–121, 127], but more research is needed to understand the systemic and local effects of intra-articular MSC injections on cellular and humoral immune responses. Clinical trials have shown that MSCs may exert cartilage reparative and/or chondroprotective effects on OA, as evidenced by imaging, second-look arthroscopy, histology, and biomarker analyses; however, additional higher-powered and controlled studies are needed to confirm these findings. While these results are promising and suggest disease-modifying effects, they provide little insight into clinical mechanisms of action given that MSCs may achieve these effects directly through the release of chondroprotective or growth factors, indirectly through the modulation of the joint microenvironment, or through some combination of the two. Similarly, investigations on antifibrotic and angiogenic mechanisms combined with greater attention to all joint tissues, including the synovium, infrapatellar fat pad, subchondral bone, menisci, and ligaments, are needed. Importantly, MSC tissue sources, donor factors, manufacturing parameters, and delivery strategies should be carefully considered, as these may impact the mechanisms of action and overall therapeutic efficacy. Altogether, an improved understanding of MSC mechanisms of action in OA could accelerate efficacious clinical translation, especially when coupled with knowledge of OA patient clinical phenotypes and endotypes to select patients for MSC therapies, as discussed in the subsequent section.
Roadmap for successful MSC OA trials
Selecting the right OA patient endotype for MSC therapies
OA is a heterogeneous disease, and at least six clinical phenotype subsets have been identified [12], including mechanical, chronic pain, metabolic, inflammatory, bone and cartilage phenotypes and minimal joint disease, representing different combinations of symptom manifestations [13]. Additionally, patients need to be classified into more complex and overlapping molecular endotypes (which include existing soluble biomarkers (reviewed in [190]). Emerging transcriptomic, lipidomic, and miR profile datasets (reviewed in [190]) will provide insights into molecular mechanisms that drive the multiple clinical phenotypes, and this represents an active area of research in better defining OA pathogenesis [13].
Categorizing OA patients with the inflammatory phenotype (based on synovial inflammation) may be most relevant to MSC therapies with their proposed anti-inflammatory mechanisms of action. Indeed, the current most effective therapeutic treatments for OA symptoms and pain are nonsteroidal anti-inflammatory drugs (NSAIDs) and intra-articular corticosteroid injections that work through anti-inflammatory effects on synovial inflammation with large effect sizes [191]. Synovial inflammation is associated with joint failure [192] and is characterized by macrophage infiltration and activation; our group has shown an inverse correlation between PROMs and the frequency of specific synovial fluid MΦ subsets in knee OA patients [97]. Given the immunomodulatory functionality of MSCs, particularly their important effects on host MΦs [99], targeting patients with molecular endotypes of inflammation for MSC treatments may be the most expedient first step in stratifying patients clinically. However, identifying this subset of patients is not easy and is postulated to be one of the reasons why clinical trials of therapies targeting inflammation, including anti-IL1 and anti-TNF therapies, have failed [193]. Indeed, subset analyses in some of these studies show significant effects, for example, of etanercept (TNF blocker) in symptomatic hand OA patients (identified by swelling/erythema and positive power Doppler by ultrasound (US) imaging) who showed significant improvements in pain and structural damage [194] when the overall cohort did not.
Part of the conundrum is that it is not clear that an inflammatory phenotype is a true OA clinical phenotype [191] or is just part of the continuum of OA pathogenesis and severity, happening on fluctuating temporal scales, dependent on obesity, physical activity and other personalized metrics [115]. Indeed, tools for measuring clinical inflammation (which may not fully reflect molecular endotypes) are varied with different sensitivities, including contrast- and noncontrast-enhanced MRI measurements [195], US measurements of synovial effusion [196], and serum biomarkers such as the degradation of C-reactive protein (CRP), connective tissue type 1 collagen turnover (C1M), and matrix metalloproteinase 3 (MMP3) [197]. Serum and local synovial fluid biomarkers may be more sensitive and reflective of molecular endotypes. However, all these measurements may be confounded by changes in body mass index and physical activity [115].
US imaging has been postulated to be one such measurement modality for identifying patients with increased inflammation [13] and has been shown to correlate with histopathological findings [198]. Indeed, in our MSC(M) knee OA trial, we used US imaging to identify patients with synovial fluid accumulation at the time of enrollment as an inclusion criterion that facilitated baseline measurements of synovial fluid immune cell subsets and proinflammatory mediators [119]. Our preliminary assessment showed interesting correlations of baseline levels of biomarkers for inflammation and cartilage degradation with patient pain and function responses at follow-up timepoints up to 24 months after single injections of autologous MSC(M) intra-articular injections (Robb et al., manuscript in preparation).
Ultimately, the use of combinatorial tools, including US and MRI, serum biomarkers, and synovial fluid levels of immune cell subsets and proinflammatory mediators, will help identify true inflammatory patient endotypes (vs. clinical phenotypes) that might be most receptive to MSC treatments based on their proposed anti-inflammatory and immunomodulatory effects, particularly on host MΦs. Flow cytometry evaluations would thus be valuable to profile cellular responses within local joint biopsy samples, including immune cell profiling of synovial fluid as we have previously shown [97, 119], as well as mass cytometry approaches as employed by Yager et al. [199] Importantly, we [97] and others [200, 201] have shown divergent profiles of local vs. circulating immune cells in OA, emphasizing the need to sample joint-specific tissues and fluids for more accurate representations of disease endotypes. Indeed, profiling patient-specific immune cells to understand host immune responses and their interactions with exogenously administered MSCs will be key to understanding and selecting appropriate patient endotypes that are responsive to MSC therapies and thus to designing successful clinical trials in OA patients [202].
The identification of circulating miR biomarkers [203] using unbiased sequencing and other omics-based approaches (genome-wide association studies [204], proteomics [205], metabolomics [206]) may provide deeper insights into patient endotype. The use of AI algorithms and bioinformatics to cohesively knit large omics datasets [207] to systematically classify patient endotypes can further advance the field. Organ-on-chip technology, which can incorporate patient-specific blood, synovial fluid, urine and/or tissue biopsy samples, offers the dual potential of providing patient baseline disease endotype information and surrogate in vitro readouts of the efficacy of various drugs or test therapeutics [208].
Designing the right MSC therapeutic product for OA
As discussed above, the immunomodulatory basal fitness of MSCs, which can be modulated by age, sex, BMI, comorbidities, manufacturing parameters and cryopreservation and can be quantified by a range of quantitative CQAs [91], is an important parameter in selecting an appropriately fit MSC therapeutic product [202]. Similar to their utility for patient endotyping, omics-based approaches may be useful to profile donor MSCs that achieve efficacious outcomes in OA clinical trials to establish correlative CQAs that correspond to beneficial patient responses and are relevant to disease-specific mechanisms of action in OA. Indeed, using MSC(M) patient samples from our previous OA clinical trial with autologous MSC(M), we performed miR sequencing and identified miR candidates that correlated with PROM improvements (Robb et al., manuscript in preparation). These miRs are currently under investigation and will provide useful insights into MSC mechanisms of action in OA and/or be used as CQAs to define MSC immunomodulatory basal fitness (Robb et al., manuscript in preparation).
Functional high-content in vitro potency assays that are relevant to the mechanisms of action may also be useful for characterizing MSCs to better understand the influence of basal fitness levels on treatment efficacy [209]. MSC(WJ) donor selection based on in vitro proliferation, trilineage differentiation and the secretion of thrombospondin-2 (a regulator of chondrogenic differentiation) was recently applied by Matas et al. in selecting basally fit MSC(WJ) for treatment groups in their RCT, from which they reported efficacious outcomes of MSC treatment [69].
As discussed above, dosing, carrier choice and selection are also not fully understood, and in many cases medium to high (≥40 × 106) doses of MSC(M) or MSC(AT) seem to provide more beneficial analgesic and cartilage structural improvements than lower doses. Including the combination of MSCs and HA or PRP or MSCs with surgical approaches has shown mixed effects on MSC-mediated chondroprotection or cartilage repair, depending on the study. To this end, cell tracking studies could provide useful insights. We have done this using iron nanoparticles approved for iron-deficiency anemia in the USA and Canada [111] to label mouse syngeneic MSC(M) and track them in a mouse surgical model of OA. Translating this to clinical trials and using MRI contrast agents such as Ferraheme® would advance our understanding of cell distribution, retention, and mechanisms of action in the joints of immunocompetent OA patients and help us better understand the MSC dosing needed for successful anti-inflammatory, analgesic and structural outcomes.
Limited short-term clinical evidence supports repeat dosing of autologous and allogeneic MSCs, albeit without a full understanding of the potential implications of alloreactions to repeat allogeneic MSC dosing. Clinical trials using allogeneic MSCs should incorporate measurements of humoral and cellular responses to better discern the correlation, if any, between alloreactions and reduced clinical efficacy. Importantly, data on longer-term structural changes as well as symptom and disease modification are not sufficient to recommend repeat injections, but they merit investigation in future clinical trials.
Ultimately, there are conflicting data regarding dosing from the RCTs and non-RCTs, and this seems to be driven in part by the baseline patient characteristics or clinical phenotyping; from our analyses, it appears that often the patients receiving lower doses of MSC products seem to have lower baseline pain/symptom scores, which confounds the analysis on dosing. Of the 15 RCTs, we noted differences in dose ranges tested for autologous (4.11–100 × 106) vs. allogeneic (3.9–150 × 106) MSCs, but we noted that this included different patient baseline characteristics; different delivery of PRP, HA, or corticosteroids; and different implementation of surgical interventions, all of which make it difficult to draw reliable conclusions regarding dosing. Moderate to higher dosing (≥40 × 106 MSCs) or repeat dosing does seem to result in more cartilage structural changes [45, 68, 126, 129, 131], but larger sample sizes, longer-term patient follow-up, and baseline patient phenotyping and endotyping are needed.
Next-generation MSCs, with improved immunomodulatory basal fitness and designed to be fit-for-purpose (for OA treatment), are also being evaluated preclinically and clinically. Small-diameter MSC(CB) grown in hypoxic conditions in calcium-rich medium with improved basal fitness, including the ability to polarize MΦs to proresolving subtypes [210], are currently being clinically tested in mid-stage OA patients in S. Korea [211]. Other non-genetic physical modification methods to enhance MSC basal fitness include transient 3D culturing to improve basal immunomodulatory fitness [91], pulsed electromagnetic field therapy to increase basal MSC chondrogenesis via TGF-β signaling [212, 213], and low-level laser therapy-primed MSCs (rev. in [214]) to improve the proliferative index.
Induced-pluripotent stem cell (iPSC)-derived MSCs (iMSCs) represent another next generation MSC product currently under clinical evaluation for the treatment of tibiofemoral knee OA in a Phase III double-blinded, randomized, controlled trial [215]. These allogeneic iMSCs will be repeatedly injected (3x) into patients randomized to the treatment arm at weeks 1, 3 and 52 at 25 × 106 cells. Importantly, the iMSCs are derived from iPSCs from a single donor, eliminating the heterogeneity challenge of using MSCs sourced from multiple donors to manufacture multiple batches needed to generate sufficient cell numbers for clinical evaluations. The safety and efficacy of injecting iMSCs will be evaluated over 24 months using pain, function and cartilage thickness measurement instruments [215]. iPSCs can be expanded as needed to generate multiple differentiated batches of relatively homogenous MSCs, ostensibly without fatiguing the MSCs or having them become senescent, as has been tested in clinical trials for GVHD [216]. However, iPSCs are not without risks, including the tumorigenicity, allorejection and heterogeneity of mixed populations containing differentiated and partially differentiated cells. The elimination of residual undifferentiated cells through various technologies [217, 218], including the incorporation of inducible suicide genes, will be a salient safety feature [219] to enable the commercialization of iPSC-differentiated cells. Different protocols to generate iPSC-derived chondrocytes, including IPSC-MSC-chondrocytes, are also being evaluated for cell-replacement therapies in OA (rev. in [220]). If iMSC OA trials are successful, this could also pave the way for the use of genetically modified iMSCs [221].
MSC-derived EVs with cargo consisting of proteins, mitochondria, miRs, ions, and lipids are also being evaluated preclinically [222, 223] for the treatment of OA. The donor heterogeneity, fitness, dosing, and mechanism of action challenges that surround MSCs will also need to be addressed for MSC-derived EVs for OA. MSC EVs for OA are currently being evaluated for safety and feasibility in Phase I/II trials (NCT05060107; NCT04314661; clinicaltrials.gov). Engineered EVs that contain cargoes of high levels of one or more key factors or exogenous therapeutic molecules are also being evaluated in various indications and will likely be of interest for OA therapeutics [224–226]. Identifying the key factors while maintaining a cocktail of other factors will require an in-depth understanding of OA etiopathogenesis to circumvent the failure of single tested therapeutics [224–226].
In summary, there are several technologies to aid in the selection or engineering of basally fit autologous or allogeneic MSC therapeutic products or engineering MSC-derived EVs that can be specifically curated for OA therapeutics. Ultimately, MSCs with multimodal anti-inflammatory, immunomodulatory, chondroprotective and antifibrotic functionalities will likely be of greatest benefit. Dosing remains an open question, although meta-analysis results seem to suggest that cartilage structural changes are feasible with >40–50 × 106 MSCs [81, 89]. Dosing needs to be understood in the context of baseline patient characteristics, both endotype and phenotype, and the interactive effects of MSC dose, MSC fitness, and baseline disease burden.
Considerations for successful clinical trial design for MSC products for OA
Clinical trials investigating MSC treatments in OA should incorporate additional readouts on putative mechanisms of action to facilitate future regulatory approvals of MSC products in OA and to tailor next-generation MSC therapies that have specific therapeutic properties and CQAs that are tuned for relevance in OA (Fig. 3). MSC mechanisms of action in OA should be investigated from at least two different perspectives: (i) detailed analyses of patient OA molecular endotype, clinical phenotype and responses to MSC treatment and (ii) detailed basal characterizations of therapeutically fit MSCs. Analyses of patient factors could involve liquid and, if permitted by ethics boards, tissue biopsy specimens collected locally from the joint and systemically at baseline and subsequently post-MSC injection. Tissue specimens could include synovial fluid, blood, urine and cartilage or synovium collected through arthroscopic debridement. Samples collected at baseline may provide insights into both the clinical phenotype and the molecular endotype based on diverse selection of biomarkers (using proteomics, metabolomics, transcriptomics, miRs, etc.), imaging modalities and PROMs and can be used to inform future patient stratification to receive precision-matched MSC therapies. Samples collected at follow-up timepoints can be used to help determine the effects of MSC injections on inflammatory, catabolic, anabolic, and fibrotic biomarkers, as we have shown previously [119].
Fig. 3.
Levers for enabling successful mesenchymal stromal cell trials in osteoarthritis - Four aspects that need to be addressed to enable successful patient outcomes. PROMs patient-reported outcome measures, CPPs critical process parameters, CQAs critical quality attributes, MSCs mesenchymal stromal cells, OA osteoarthritis
The episodic nature of OA, termed “flare-ups”, is poorly understood etiologically [227]; these flare-ups can be of varying durations and intensities and involve not only the exacerbation of pain, stiffness, and swelling of the joint but also the psychological and other consequential aspects of the flare-ups [228]. Appropriate timing of delivery for MSC therapies to coincide with flare-ups might result in both short-term symptom- and disease-modifying effects and longer-term disease-modifying sequalae, as OA is being better understood as an “acute-on-chronic" disease [227]. However, current instruments may be insufficient to investigate the temporal kinetics of “flare-ups”. Clinical trials can be designed with combinatorial measurement tools, including patient-reported data, biomarker and biomechanic evaluations [229–231], to capture the extent and frequency of “flare-ups”. Correlation between the occurrence of “flare-ups” and patient responses to MSC treatments in the short and longer term will inform future patient stratification strategies and timing of MSC treatments relative to OA “flare-ups”.
There are existing guidelines for clinical trial design considerations, including the selection of OA patient populations, as put out by the European Medicines Agency (EMA) [232]. This guideline spells out the following multiple design requirements: (i) the need for including patients with baseline symptomatic and structural changes; (ii) documenting patient characteristics (clinical phenotype), including the extent of disease, the duration of symptoms, joint misalignment, overuse due to work, sports, etc. (which would capture patient-reported data regarding OA flare ups); (iii) recommendations for enrolling patients with at least >40 mm on the VAS scale (0–100 mm); (iv) using the absolute change in validated pain scales as the primary endpoint for the evaluation of symptom-modifying drugs; and (v) using joint-space narrowing measured by standardized radiographic measures as an indications for structure-altering drugs even though the correlation between structural changes and patient outcomes is weak. Indeed, the FDA issued draft guidance on the basis of new data submitted by invited OA experts that showed a correlation of structural endpoint changes with patient symptoms and pain [233]. There is recognition by regulators that radiographic changes or those identified by MRI may not translate into clinically meaningful outcomes for patients, and there is an openness to consider other biomarkers that better correlate structural changes with patient outcomes [234]. Thus, clinical trials should incorporate traditional pain, function, and structural endpoints using validated patient-reported outcome instruments and radiological and imaging modalities and include a large number of secondary endpoints that can help capture local and systemic inflammatory changes and changes to cartilage degradation biomarkers, as we did [119]. Additionally, detailed collection and reporting of basal and follow-up patient characterization to include clinical phenotype and molecular endotype (using PROMs, biomarkers, and imaging and biomechanical measurements) will be critically important in parsing out the effects of MSC treatment with respect to different patient clinical phenotypes and disease endotypes in subsequent post hoc and meta-analyses.
Cost is another consideration for the commercialization of successful MSC therapeutic products. The extent of the effect size and whether there are symptom-modifying or disease-modifying effects (as evaluated by a combination of PROMs, imaging, and biomarker and biomechanic assays) will determine the willingness to pay of the health care system and market. Using patient survey-based methods, Piuzzi et al. obtained pricing information for same-day minimally manipulated autologous cell preparations from 65 centers in the USA and found that the mean price was US$ 5156 ± 2446 for a single treatment [235]. Many of these procedures are not approved by regulatory bodies and have no evidence or mixed levels of evidence of efficacy, are usually marketed directly to consumers, and require out-of-pocket pay. Even with these caveats, these findings showcase a willingness among OA patients to pay for these therapies. Specifically, a S. Korea MSC(CB) product for treatment of degenerative arthritis showed that the incremental cost-effectiveness ratio (ICER) in terms of quality-adjusted life-years (QALYs) was US$ 16,812 per QALY when compared to microfracture [182], a surgical procedure involving drilling holes in the bone and enabling clot formation and endogenous cartilage repair. Efficacy data were obtained from 5-year follow-up from RCTs, while health care utilization costs were based on the S. Korean health care system. Even with these caveats, the ICER is lower than cost-effectiveness thresholds in different countries [236], typically benchmarked to the gross domestic product (GDP), including the USA (US$ 50 000), Canada (US$ 15–22,000) and UK (US$ 24–36,000). This lends optimism to having a reimbursable MSC product for OA, particularly if longer-term effects can be demonstrated. Thus, the follow-up of patients (beyond the typical 12-month endpoints) and understanding changes in disease trajectory, including further requirements for surgical interventions (and the time scale of those), will be important data for sponsors to obtain to support health cost economic analyses. Ultimately, a successful MSC therapeutic product is one that is not only authorized by regulators but also routinely used by clinicians and is reimbursed by health care payers.
Summary
Even with 15 completed RCTs, the sample size of 610 treated patients (with MSCs and control treatments) is relatively small to reach definitive conclusions on optimal dosing, baseline patient endotype and phenotype, delivery strategies, MSC sourcing, manufacturing, and overall treatment efficacy. Nonetheless, the findings of meta-analyses and our own analyses revealed positive effects on pain, function and symptoms at final follow-up endpoints in MSC-treated patients relative to baseline (12/15). In 11/15 RCTs, there were improvements in these metrics relative to the control group (HA, PRP, or surgical intervention) at 6 months or longer, depending on the dose of MSC, MSC basal fitness, the baseline clinical phenotype of the patient and the choice of the control comparator. MSCs have also demonstrated chondroprotective or regenerative effects on cartilage in 18/21 clinical studies, including 11/15 RCTs. MSCs have multimodal mechanisms of action, including chondroprotective effects, effects on cartilage repair and ECM anabolism, and pro-angiogenic, antifibrotic, anti-inflammatory and immunomodulatory effects, but there is a dearth of clinical data to confirm these mechanisms in OA. Defining baseline patient disease endotype along with clinical phenotyping will help identify and stratify patients who are receptive to receiving MSC therapies. Patient endotyping will require combinatorial tools, including different types of omics data, levels of systemic and local inflammatory markers, and immune cell subpopulations, which will need to be correlated with patient clinical outcomes and structural changes to validate them as sensitive and reliable biomarkers of patient endotypes. The episodic nature of OA further confounds the categorization of patients by clinical phenotype and/or disease endotyping but should be factored in to better understand the highly heterogeneous, personalized and temporally variable nature of disease progression. The selection of basally fit MSC products involves selecting MSCs from a host of donors that display CQAs that are relevant in the context of OA, including immunomodulatory properties, angiogenic properties and tissue remodeling properties. CQAs are modifiable by culture expansion and cryopreservation, and hence, care needs to be taken to optimize these parameters to maintain the CQAs of MSC products for clinical use. Ultimately, basally fit MSC products may be genetically engineered or nongenetically primed to be “fit-for-OA" with enhanced immunomodulatory and/or pro-angiogenic and/or cartilage-reparative properties to override reliance on donor heterogeneity and culture parameters. A combination of basally fit MSCs that are applied to a subset of knee OA patients who are receptive to receiving MSC treatments (based on disease endotyping and clinical phenotyping) will result in successful outcomes. Statistical modeling will need to be used to collect data from different trials to show the correlation between patient basal status, MSC basal fitness status and ultimately responder/nonresponder status. To enable this, larger sample sizes (for example, a 1020 patient Phase III trial to investigate the safety and efficacy of INVOSSA™, a gene-engineered cell therapy product for OA [237]) or, alternatively, a pooled, registry-based approach with agreements in place to facilitate open sharing of collected data will be necessary to overcome the significant challenges posed by this multifactorial disease, which has proven refractory to multiple therapeutics. Clinical trials will need to be designed with this in mind and actively strive to collect and report on multiple variables to enable patient endotyping/clinical phenotyping and follow-up involving patient outcomes, structural changes (imaging) and biomarkers. Longer periods of follow-up will increase confidence in the effects and the duration of the effects on outcome measures and enable cost justification of MSC therapies. These approaches will entail higher costs for clinical trial sponsors and may behoove a collaborative, consortium-based approach that the FDA has signaled a willingness to entertain [238]. Ultimately, larger, well-designed, targeted clinical trials with extensive characterization of the OA patient population and the MSC product or pooled data from several clinical trials through nontraditional consortium approaches will be needed to advance MSC therapies in OA.
Acknowledgements
This research was funded by the Canadian Institutes of Health Research (CIHR) (PJT-166089) and the Natural Sciences and Engineering Research Council of Canada (NSERC) (RGPIN-2018-05737). This work is in part supported by the Schroeder Arthritis Institute via the Toronto General and Western Hospital Foundation (University Health Network). We gratefully acknowledge editing support from Anu Thomas.
Competing interests
SV has 60% ownership of Regulatory Cell Therapy Consultants Inc., which does not conflict with this paper in any way. KR and GC declare no conflicts of interest.
Footnotes
These authors contributed equally: Griffin Copp, Kevin P. Robb.
References
- 1.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. doi: 10.1016/j.eclinm.2020.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:1323–30. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 3.Prevalence Trends of Site‐Specific Osteoarthritis From 1990 to 2019: Findings From the Global Burden of Disease Study 2019 - Long − 2022 - Arthritis & Rheumatology - Wiley Online Library [Internet]. [cited 2022 Dec 28]. Available from: https://onlinelibrary.wiley.com/doi/10.1002/art.42089 [DOI] [PMC free article] [PubMed]
- 4.Canada PHA of Life with arthritis in Canada: a personal and public health challenge [Internet]. 2010 [cited 2021 Nov 23]. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/arthritis/life-arthritis-canada-a-personal-public-health-challenge.html
- 5.Murphy LB, Cisternas MG, Pasta DJ, Helmick CG, Yelin EH. Medical Expenditures and Earnings Losses Among US Adults With Arthritis in 2013. Arthritis Care Res (Hoboken). 2018;70:869–76. [DOI] [PubMed]
- 6.Billesberger LM, Fisher KM, Qadri YJ, Boortz-Marx RL. Procedural treatments for knee osteoarthritis: a review of current injectable therapies. Pain Res Manag. 2020;2020:e3873098. doi: 10.1155/2020/3873098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Drumpt RAM, van der Weegen W, King W, Toler K, Macenski MM. Safety and treatment effectiveness of a single autologous protein solution injection in patients with knee osteoarthritis. Biores Open Access. 2016;5:261–8. doi: 10.1089/biores.2016.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lohmander LS, Roos EM. Clinical update: treating osteoarthritis. Lancet. 2007;370:2082–4. doi: 10.1016/S0140-6736(07)61879-0. [DOI] [PubMed] [Google Scholar]
- 9.Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64:1697–707. doi: 10.1002/art.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tonge DP, Pearson MJ, Jones SW. The hallmarks of osteoarthritis and the potential to develop personalised disease-modifying pharmacological therapeutics. Osteoarthr Cartil. 2014;22:609–21. doi: 10.1016/j.joca.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Li G, Yin J, Gao J, Cheng TS, Pavlos NJ, Zhang C, et al. Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes. Arthritis Res Ther. 2013;15:223. doi: 10.1186/ar4405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dell’Isola A, Allan R, Smith SL, Marreiros SSP, Steultjens M. Identification of clinical phenotypes in knee osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord. 2016;17:425. doi: 10.1186/s12891-016-1286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mobasheri A, Saarakkala S, Finnilä M, Karsdal MA, Bay-Jensen AC, van Spil WE. Recent advances in understanding the phenotypes of osteoarthritis. F1000Res. 2019;8:F1000. doi: 10.12688/f1000research.20575.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buckwalter JA. Osteoarthritis and articular cartilage use, disuse, and abuse: experimental studies. J Rheumatol Suppl. 1995;43:13–5. [PubMed] [Google Scholar]
- 15.Guilak F. Biomechanical factors in osteoarthritis. Best Pr Res Clin Rheumatol. 2011;25:815–23. doi: 10.1016/j.berh.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med. 2000;133:321–8. doi: 10.7326/0003-4819-133-5-200009050-00007. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, McAlindon TE, Hannan MT, Chaisson CE, Klein R, Wilson PW, et al. Estrogen replacement therapy and worsening of radiographic knee osteoarthritis: the Framingham Study. Arthritis Rheum. 1998;41:1867–73. doi: 10.1002/1529-0131(199810)41:10<1867::AID-ART20>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 18.Sandmark H, Hogstedt C, Lewold S, Vingård E. Osteoarthrosis of the knee in men and women in association with overweight, smoking, and hormone therapy. Ann Rheum Dis. 1999;58:151–5. doi: 10.1136/ard.58.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. the framingham osteoarthritis study. Arthritis Rheum. 1987;30:914–8. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 20.Cunningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health. 1984;74:574–9. doi: 10.2105/AJPH.74.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Saase JL, van Romunde LK, Cats A, Vandenbroucke JP, Valkenburg HA. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis. 1989;48:271–80. doi: 10.1136/ard.48.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B, Aliabadi P, et al. Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum. 1997;40:728–33. doi: 10.1002/art.1780400420. [DOI] [PubMed] [Google Scholar]
- 23.Davis MA, Ettinger WH, Neuhaus JM, Cho SA, Hauck WW. The association of knee injury and obesity with unilateral and bilateral osteoarthritis of the knee. Am J Epidemiol. 1989;130:278–88. doi: 10.1093/oxfordjournals.aje.a115334. [DOI] [PubMed] [Google Scholar]
- 24.Puenpatom RA, Victor TW. Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med. 2009;121:9–20. doi: 10.3810/pgm.2009.11.2073. [DOI] [PubMed] [Google Scholar]
- 25.Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T. Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol. 2011;38:921–30. doi: 10.3899/jrheum.100569. [DOI] [PubMed] [Google Scholar]
- 26.Sowers M, Karvonen-Gutierrez CA, Palmieri-Smith R, Jacobson JA, Jiang Y, Ashton-Miller JA. Knee osteoarthritis in obese women with cardiometabolic clustering. Arthritis Rheum. 2009;61:1328–36. doi: 10.1002/art.24739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh P, Marcu KB, Goldring MB, Otero M. Phenotypic instability of chondrocytes in osteoarthritis: on a path to hypertrophy. Ann N. Y Acad Sci. 2019;1442:17–34. doi: 10.1111/nyas.13930. [DOI] [PubMed] [Google Scholar]
- 28.Hwang HS, Kim HA. Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int J Mol Sci. 2015;16:26035–54. doi: 10.3390/ijms161125943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Kraan PM, van den Berg WB. Chondrocyte hypertrophy and osteoarthritis: role in initiation and progression of cartilage degeneration? Osteoarthr Cartil. 2012;20:223–32. doi: 10.1016/j.joca.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Yuan XL, Meng HY, Wang YC, Peng J, Guo QY, Wang AY, et al. Bone-cartilage interface crosstalk in osteoarthritis: potential pathways and future therapeutic strategies. Osteoarthr Cartil. 2014;22:1077–89. doi: 10.1016/j.joca.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 31.Zhen G, Wen C, Jia X, Li Y, Crane JL, Mears SC, et al. Inhibition of TGF–β signaling in subchondral bone mesenchymal stem cells attenuates osteoarthritis. Nat Med. 2013;19:704. doi: 10.1038/nm.3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Funck-Brentano T, Cohen-Solal M. Subchondral bone and osteoarthritis. Curr Opin Rheumatol. 2015;27:420–6. doi: 10.1097/BOR.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 33.De Bari C, Dell’Accio F, Tylzanowski P, Luyten FP. Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum. 2001;44:1928–42. doi: 10.1002/1529-0131(200108)44:8<1928::AID-ART331>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 34.Iwanaga T, Shikichi M, Kitamura H, Yanase H, Nozawa-Inoue K. Morphology and functional roles of synoviocytes in the joint. Arch Histol Cytol. 2000;63:17–31. doi: 10.1679/aohc.63.17. [DOI] [PubMed] [Google Scholar]
- 35.Man GS, Mologhianu G. Osteoarthritis pathogenesis—a complex process that involves the entire joint. J Med Life. 2014;7:37–41. [PMC free article] [PubMed] [Google Scholar]
- 36.Bondeson J, Blom AB, Wainwright S, Hughes C, Caterson B, van den Berg WB. The role of synovial macrophages and macrophage-produced mediators in driving inflammatory and destructive responses in osteoarthritis. Arthritis Rheum. 2010;62:647–57. doi: 10.1002/art.27290. [DOI] [PubMed] [Google Scholar]
- 37.Bondeson J, Wainwright SD, Lauder S, Amos N, Hughes CE. The role of synovial macrophages and macrophage-produced cytokines in driving aggrecanases, matrix metalloproteinases, and other destructive and inflammatory responses in osteoarthritis. Arthritis Res Ther. 2006;8:R187. doi: 10.1186/ar2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacDonald IJ, Liu SC, Su CM, Wang YH, Tsai CH, Tang CH. Implications of angiogenesis involvement in arthritis. Int J Mol Sci. 2018;19:2012. doi: 10.3390/ijms19072012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henrotin Y, Pesesse L, Lambert C. Targeting the synovial angiogenesis as a novel treatment approach to osteoarthritis. Ther Adv Musculoskelet Dis. 2014;6:20–34. doi: 10.1177/1759720X13514669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Larsson S, Englund M, Struglics A, Lohmander LS. Interleukin-6 and tumor necrosis factor alpha in synovial fluid are associated with progression of radiographic knee osteoarthritis in subjects with previous meniscectomy. Osteoarthr Cartil. 2015;23:1906–14. doi: 10.1016/j.joca.2015.05.035. [DOI] [PubMed] [Google Scholar]
- 41.Wojdasiewicz P, Poniatowski ŁA, Szukiewicz D. The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediat Inflamm. 2014;2014:561459. doi: 10.1155/2014/561459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Osteoarthritis endotype discovery via clustering of biochemical marker data | Annals of the Rheumatic Diseases [Internet]. [cited 2022 Dec 24]. Available from: https://ard.bmj.com/content/81/5/666 [DOI] [PubMed]
- 43.Rahmati M, Mobasheri A, Mozafari M. Inflammatory mediators in osteoarthritis: a critical review of the state-of-the-art, current prospects, and future challenges. Bone. 2016;85:81–90. doi: 10.1016/j.bone.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 44.Song Y, Jorgensen C. Mesenchymal stromal cells in osteoarthritis: evidence for structural benefit and cartilage repair. Biomedicines. 2022;10:1278. doi: 10.3390/biomedicines10061278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014;32:1254–66. doi: 10.1002/stem.1634. [DOI] [PubMed] [Google Scholar]
- 46.Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC, et al. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One. 2012;7:e47559. doi: 10.1371/journal.pone.0047559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barry F. MSC therapy for osteoarthritis: an unfinished story. J Orthop Res. 2019;37:1229–35. doi: 10.1002/jor.24343. [DOI] [PubMed] [Google Scholar]
- 48.Thompson M, Mei SHJ, Wolfe D, Champagne J, Fergusson D, Stewart DJ, et al. Cell therapy with intravascular administration of mesenchymal stromal cells continues to appear safe: an updated systematic review and meta-analysis. EClinicalMedicine. 2020;19:100249. doi: 10.1016/j.eclinm.2019.100249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wright A, Arthaud-Day ML, Weiss ML. Therapeutic Use of Mesenchymal Stromal Cells: The Need for Inclusive Characterization Guidelines to Accommodate All Tissue Sources and Species. Front Cell Develop Biol [Internet]. 2021 [cited 2022 Dec 15];9. Available from: https://www.frontiersin.org/articles/10.3389/fcell.2021.632717 [DOI] [PMC free article] [PubMed]
- 50.Levy O, Kuai R, Siren EMJ, Bhere D, Milton Y, Nissar N, et al. Shattering barriers toward clinically meaningful MSC therapies. Sci Adv. 2020;6:eaba6884. doi: 10.1126/sciadv.aba6884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robb KP, Fitzgerald JC, Barry F, Viswanathan S. Mesenchymal stromal cell therapy: progress in manufacturing and assessments of potency. Cytotherapy. 2019;21:289–306. doi: 10.1016/j.jcyt.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 52.Medipost Co Ltd. Evaluation of Safety and Exploratory Efficacy of CARTISTEM®, a Cell Therapy Product for Articular Cartilage Defects: A Phase I/IIa Clinical Trial in Patients With Focal, Full-thickness Grade 3-4 Articular Cartilage Defects of the Knee [Internet]. clinicaltrials.gov; 2021 Jul [cited 2022 Dec 21]. Report No.: NCT01733186. Available from: https://clinicaltrials.gov/ct2/show/NCT01733186
- 53.Limited M Mesoblast Receives Complete Response Letter From the FDA for Biologics License Application for Steroid-Refractory Acute Graft Versus Host Disease in Children [Internet]. GlobeNewswire News Room. 2020 [cited 2021 Feb 10]. Available from: http://www.globenewswire.com/news-release/2020/10/01/2102679/0/en/Mesoblast-Receives-Complete-Response-Letter-From-the-FDA-for-Biologics-License-Application-for-Steroid-Refractory-Acute-Graft-Versus-Host-Disease-in-Children.html
- 54.Muthu S, Jeyaraman M, Narula A, Ravi VR, Gandi A, Khanna M, et al. Factors influencing the yield of progenitor cells in bone marrow aspiration concentrate—a retrospective analysis of 58 patients. Biomedicines. 2023;11:738. doi: 10.3390/biomedicines11030738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ha CW, Park YB, Kim SH, Lee HJ. Intra-articular mesenchymal stem cells in osteoarthritis of the knee: a systematic review of clinical outcomes and evidence of cartilage repair. Arthroscopy. 2019;35:277–88.e2. doi: 10.1016/j.arthro.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 56.Lamo-Espinosa JM, Mora G, Blanco JF, Granero-Moltó F, Núñez-Córdoba JM, López-Elío S, et al. Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: long-term follow up of a multicenter randomized controlled clinical trial (phase I/II) J Transl Med. 2018;16:213. doi: 10.1186/s12967-018-1591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee WS, Kim HJ, Kim KI, Kim GB, Jin W. Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med. 2019;8:504–11. doi: 10.1002/sctm.18-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Freitag J, Bates D, Wickham J, Shah K, Huguenin L, Tenen A, et al. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: a randomized controlled trial. Regen Med. 2019;14:213–30. doi: 10.2217/rme-2018-0161. [DOI] [PubMed] [Google Scholar]
- 59.Lamo-Espinosa JM, Blanco JF, Sánchez M, Moreno V, Granero-Moltó F, Sánchez-Guijo F, et al. Phase II multicenter randomized controlled clinical trial on the efficacy of intra-articular injection of autologous bone marrow mesenchymal stem cells with platelet rich plasma for the treatment of knee osteoarthritis. J Transl Med. 2020;18:356. doi: 10.1186/s12967-020-02530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lamo-Espinosa JM, Mora G, Blanco JF, Granero-Moltó F, Nuñez-Córdoba JM, Sánchez-Echenique C, et al. Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: multicenter randomized controlled clinical trial (phase I/II) J Transl Med. 2016;14:246. doi: 10.1186/s12967-016-0998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lu L, Dai C, Zhang Z, Du H, Li S, Ye P, et al. Treatment of knee osteoarthritis with intra-articular injection of autologous adipose-derived mesenchymal progenitor cells: a prospective, randomized, double-blind, active-controlled, phase IIb clinical trial. Stem Cell Res Ther. 2019;10:143. doi: 10.1186/s13287-019-1248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bastos R, Mathias M, Andrade R, Amaral RJFC, Schott V, Balduino A, et al. Intra-articular injection of culture-expanded mesenchymal stem cells with or without addition of platelet-rich plasma is effective in decreasing pain and symptoms in knee osteoarthritis: a controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2020;28:1989–99. doi: 10.1007/s00167-019-05732-8. [DOI] [PubMed] [Google Scholar]
- 63.Emadedin M, Labibzadeh N, Liastani MG, Karimi A, Jaroughi N, Bolurieh T, et al. Intra-articular implantation of autologous bone marrow–derived mesenchymal stromal cells to treat knee osteoarthritis: a randomized, triple-blind, placebo-controlled phase 1/2 clinical trial. Cytotherapy. 2018;20:1238–46. doi: 10.1016/j.jcyt.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 64.Injectable Cultured Bone Marrow–Derived Mesenchymal Stem Cells in Varus Knees With Cartilage Defects Undergoing High Tibial Osteotomy: A Prospective, Randomized Controlled Clinical Trial With 2 Years’ Follow-up - ClinicalKey [Internet]. [cited 2023 Jan 11]. Available from: https://www.clinicalkey.com/#!/content/playContent/1-s2.0-S0749806313010736?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0749806313010736%3Fshowall%3Dtrue&referrer= [DOI] [PubMed]
- 65.Gupta PK, Chullikana A, Rengasamy M, Shetty N, Pandey V, Agarwal V, et al. Efficacy and safety of adult human bone marrow-derived, cultured, pooled, allogeneic mesenchymal stromal cells (Stempeucel®): preclinical and clinical trial in osteoarthritis of the knee joint. Arthritis Res Ther. 2016;18:301. doi: 10.1186/s13075-016-1195-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen CF, Hu CC, Wu CT, Wu HTH, Chang CS, Hung YP, et al. Treatment of knee osteoarthritis with intra-articular injection of allogeneic adipose-derived stem cells (ADSCs) ELIXCYTE®: a phase I/II, randomized, active-control, single-blind, multiple-center clinical trial. Stem Cell Res Ther. 2021;12:562. doi: 10.1186/s13287-021-02631-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Khalifeh Soltani S, Forogh B, Ahmadbeigi N, Hadizadeh Kharazi H, Fallahzadeh K, Kashani L, et al. Safety and efficacy of allogenic placental mesenchymal stem cells for treating knee osteoarthritis: a pilot study. Cytotherapy. 2019;21:54–63. doi: 10.1016/j.jcyt.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 68.Vega A, Martín-Ferrero MA, Del Canto F, Alberca M, García V, Munar A, et al. Treatment of knee osteoarthritis with allogeneic bone marrow mesenchymal stem cells: a randomized controlled trial. Transplantation. 2015;99:1681–90. doi: 10.1097/TP.0000000000000678. [DOI] [PubMed] [Google Scholar]
- 69.Matas J, Orrego M, Amenabar D, Infante C, Tapia-Limonchi R, Cadiz MI, et al. Umbilical cord-derived mesenchymal stromal cells (MSCs) for knee osteoarthritis: repeated MSC dosing is superior to a single MSC dose and to hyaluronic acid in a controlled randomized phase I/II trial. Stem Cells Transl Med. 2019;8:215–24. doi: 10.1002/sctm.18-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kuah D, Sivell S, Longworth T, James K, Guermazi A, Cicuttini F, et al. Safety, tolerability and efficacy of intra-articular Progenza in knee osteoarthritis: a randomized double-blind placebo-controlled single ascending dose study. J Transl Med. 2018;16:49. doi: 10.1186/s12967-018-1420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Koh YG, Kwon OR, Kim YS, Choi YJ. Comparative outcomes of open-wedge high tibial osteotomy with platelet-rich plasma alone or in combination with mesenchymal stem cell treatment: a prospective study. Arthrosc J Arthrosc Relat Surg. 2014;30:1453–60. doi: 10.1016/j.arthro.2014.05.036. [DOI] [PubMed] [Google Scholar]
- 72.Molnar V, Pavelić E, Vrdoljak K, Čemerin M, Klarić E, Matišić V, et al. Mesenchymal stem cell mechanisms of action and clinical effects in osteoarthritis: a narrative review. Genes. 2022;13:949. doi: 10.3390/genes13060949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tan SSH, Tjio CKE, Wong JRY, Wong KL, Chew JRJ, Hui JHP, et al. Mesenchymal stem cell exosomes for cartilage regeneration: a systematic review of preclinical in vivo studies. Tissue Eng Part B Rev. 2021;27:1–13. doi: 10.1089/ten.teb.2019.0326. [DOI] [PubMed] [Google Scholar]
- 74.Xiang XN, Zhu SY, He HC, Yu X, Xu Y, He CQ. Mesenchymal stromal cell-based therapy for cartilage regeneration in knee osteoarthritis. Stem Cell Res Ther. 2022;13:14. doi: 10.1186/s13287-021-02689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Freitag J, Ford J, Bates D, Boyd R, Hahne A, Wang Y, et al. Adipose derived mesenchymal stem cell therapy in the treatment of isolated knee chondral lesions: design of a randomised controlled pilot study comparing arthroscopic microfracture versus arthroscopic microfracture combined with postoperative mesenchymal stem cell injections. BMJ Open. 2015;5:e009332. doi: 10.1136/bmjopen-2015-009332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Awad ME, Hussein KA, Helwa I, Abdelsamid MF, Aguilar-Perez A, Mohsen I, et al. Meta-analysis and evidence base for the efficacy of autologous bone marrow mesenchymal stem cells in knee cartilage repair: methodological guidelines and quality assessment. Stem Cells Int. 2019;2019:3826054. doi: 10.1155/2019/3826054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cao Z, Li Y, Gao F, Wu R, Dou P, Wang W, et al. Mesenchymal stem cells: a new choice for nonsurgical treatment of OA? Results from a Bayesian network meta-analysis. Biomed Res Int. 2021;2021:6663003. doi: 10.1155/2021/6663003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tan SHS, Kwan YT, Neo WJ, Chong JY, Kuek TYJ, See JZF, et al. Intra-articular injections of mesenchymal stem cells without adjuvant therapies for knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2021;49:3113–24. doi: 10.1177/0363546520981704. [DOI] [PubMed] [Google Scholar]
- 79.Song Y, Zhang J, Xu H, Lin Z, Chang H, Liu W, et al. Mesenchymal stem cells in knee osteoarthritis treatment: a systematic review and meta-analysis. J Orthop Transl. 2020;24:121–30. doi: 10.1016/j.jot.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Qu H, Sun S. Efficacy of mesenchymal stromal cells for the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2021;16:11. doi: 10.1186/s13018-020-02128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jeyaraman M, Muthu S, Ganie PA. Does the source of mesenchymal stem cell have an effect in the management of osteoarthritis of the knee? Meta-analysis of randomized controlled trials. Cartilage. 2021;13:1532S–47S. doi: 10.1177/1947603520951623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cui GH, Wang YY, Li CJ, Shi CH, Wang WS. Efficacy of mesenchymal stem cells in treating patients with osteoarthritis of the knee: a meta-analysis. Exp Ther Med. 2016;12:3390–400. doi: 10.3892/etm.2016.3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Iijima H, Isho T, Kuroki H, Takahashi M, Aoyama T. Effectiveness of mesenchymal stem cells for treating patients with knee osteoarthritis: a meta-analysis toward the establishment of effective regenerative rehabilitation. NPJ Regen Med. 2018;3:15. doi: 10.1038/s41536-018-0041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maheshwer B, Polce EM, Paul K, Williams BT, Wolfson TS, Yanke A, et al. Regenerative potential of mesenchymal stem cells for the treatment of knee osteoarthritis and chondral defects: a systematic review and meta-analysis. Arthroscopy. 2021;37:362–78. doi: 10.1016/j.arthro.2020.05.037. [DOI] [PubMed] [Google Scholar]
- 85.Hwang JJ, Rim YA, Nam Y, Ju JH. Recent developments in clinical applications of mesenchymal stem cells in the treatment of rheumatoid arthritis and osteoarthritis. Front Immunol [Internet]. 2021 [cited 2022 Dec 24];12. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2021.631291 [DOI] [PMC free article] [PubMed]
- 86.Steenkamp W, Rachuene PA, Dey R, Mzayiya NL, Ramasuvha BE. The correlation between clinical and radiological severity of osteoarthritis of the knee. SICOT J. 2022;8:14. doi: 10.1051/sicotj/2022014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Moretti B, Spinarelli A, Varrassi G, Massari L, Gigante A, Iolascon G, et al. Influence of sex and gender on the management of late-stage knee osteoarthritis. Musculoskelet Surg. 2022;106:457–67. doi: 10.1007/s12306-021-00725-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kuçi Z, Bönig H, Kreyenberg H, Bunos M, Jauch A, Janssen JWG, et al. Mesenchymal stromal cells from pooled mononuclear cells of multiple bone marrow donors as rescue therapy in pediatric severe steroid-refractory graft-versus-host disease: a multicenter survey. Haematologica. 2016;101:985–94. doi: 10.3324/haematol.2015.140368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Doyle EC, Wragg NM, Wilson SL. Intraarticular injection of bone marrow-derived mesenchymal stem cells enhances regeneration in knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2020;28:3827–42. doi: 10.1007/s00167-020-05859-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Galipeau J, Sensébé L. Mesenchymal stromal cells: clinical challenges and therapeutic opportunities. Cell Stem Cell. 2018;22:824–33. doi: 10.1016/j.stem.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Robb KP, Audet J, Gandhi R, Viswanathan S. Putative critical quality attribute matrix identifies mesenchymal stromal cells with potent immunomodulatory and angiogenic “fitness” ranges in response to culture process parameters. Front Immunol. 2022;13:972095. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2022.972095/abstract [DOI] [PMC free article] [PubMed]
- 92.August 13, 2020: Meeting of the Oncologic Drugs Advisory Committee Meeting Announcement - 08/13/2020 - 08/13/2020 [Internet]. FDA. 2020 [cited 2022 Dec 22]. Available from: https://www.fda.gov/advisory-committees/advisory-committee-calendar/august-13-2020-meeting-oncologic-drugs-advisory-committee-meeting-announcement-08132020-08132020
- 93.Woodell-May JE, Sommerfeld SD. Role of inflammation and the immune system in the progression of osteoarthritis. J Orthop Res. 2020;38:253–7. doi: 10.1002/jor.24457. [DOI] [PubMed] [Google Scholar]
- 94.Sanchez-Lopez E, Coras R, Torres A, Lane NE, Guma M. Synovial inflammation in osteoarthritis progression. Nat Rev Rheumatol. 2022;18:258–75. doi: 10.1038/s41584-022-00749-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Culemann S, Grüneboom A, Nicolás-Ávila JÁ, Weidner D, Lämmle KF, Rothe T, et al. Locally renewing resident synovial macrophages provide a protective barrier for the joint. Nature. 2019;572:670–5. doi: 10.1038/s41586-019-1471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zeng N, Yan ZP, Chen XY, Ni GX. Infrapatellar fat pad and knee osteoarthritis. Aging Dis. 2020;11:1317–28. doi: 10.14336/AD.2019.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gómez-Aristizábal A, Gandhi R, Mahomed NN, Marshall KW, Viswanathan S. Synovial fluid monocyte/macrophage subsets and their correlation to patient-reported outcomes in osteoarthritic patients: a cohort study. Arthritis Res Ther. 2019;21:26. doi: 10.1186/s13075-018-1798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li YS, Luo W, Zhu SA, Lei GH. T cells in osteoarthritis: alterations and beyond. Front Immunol. 2017;8:356. doi: 10.3389/fimmu.2017.00356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Galipeau J. Macrophages at the nexus of mesenchymal stromal cell potency: the emerging role of chemokine cooperativity. Stem Cells. 2021;39:1145–54. doi: 10.1002/stem.3380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Song N, Scholtemeijer M, Shah K. Mesenchymal stem cell immunomodulation: mechanisms and therapeutic potential. Trends Pharm Sci. 2020;41:653–64. doi: 10.1016/j.tips.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Najar M, Martel-Pelletier J, Pelletier JP, Fahmi H. Mesenchymal stromal cell immunology for efficient and safe treatment of osteoarthritis. Front Cell Develop Biol [Internet]. 2020 [cited 2023 Mar 13];8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7536322/ [DOI] [PMC free article] [PubMed]
- 102.Fahy N, de Vries-van Melle ML, Lehmann J, Wei W, Grotenhuis N, Farrell E, et al. Human osteoarthritic synovium impacts chondrogenic differentiation of mesenchymal stem cells via macrophage polarisation state. Osteoarthr Cartil. 2014;22:1167–75. doi: 10.1016/j.joca.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 103.Manferdini C, Maumus M, Gabusi E, Piacentini A, Filardo G, Peyrafitte JA, et al. Adipose-derived mesenchymal stem cells exert antiinflammatory effects on chondrocytes and synoviocytes from osteoarthritis patients through prostaglandin E2. Arthritis Rheum. 2013;65:1271–81. doi: 10.1002/art.37908. [DOI] [PubMed] [Google Scholar]
- 104.Hamilton AM, Cheung WY, Gómez-Aristizábal A, Sharma A, Nakamura S, Chaboureau A, et al. Iron nanoparticle-labeled murine mesenchymal stromal cells in an osteoarthritic model persists and suggests anti-inflammatory mechanism of action. PLoS One. 2019;14:e0214107. doi: 10.1371/journal.pone.0214107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schelbergen RF, Dalen S, van, Huurne M, ter, Roth J, Vogl T, Noël D, et al. Treatment efficacy of adipose-derived stem cells in experimental osteoarthritis is driven by high synovial activation and reflected by S100A8/A9 serum levels. Osteoarthr Cartil. 2014;22:1158–66. doi: 10.1016/j.joca.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 106.van Dalen SCM, Blom AB, Walgreen B, Slöetjes AW, Helsen MMA, Geven EJW, et al. IL-1β-Mediated activation of adipose-derived mesenchymal stromal cells results in PMN reallocation and enhanced phagocytosis: a possible mechanism for the reduction of osteoarthritis pathology. Front Immunol [Internet]. 2019 [cited 2022 Dec 22];10. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2019.01075 [DOI] [PMC free article] [PubMed]
- 107.Grady ST, Britton L, Hinrichs K, Nixon AJ, Watts AE. Persistence of fluorescent nanoparticle-labeled bone marrow mesenchymal stem cells in vitro and after intra-articular injection. J Tissue Eng Regen Med. 2019;13:191–202. doi: 10.1002/term.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Delling U, Brehm W, Metzger M, Ludewig E, Winter K, Jülke H. In vivo tracking and fate of intra-articularly injected superparamagnetic iron oxide particle-labeled multipotent stromal cells in an ovine model of osteoarthritis. Cell Transpl. 2015;24:2379–90. doi: 10.3727/096368914X685654. [DOI] [PubMed] [Google Scholar]
- 109.Feng C, Luo X, He N, Xia H, Lv X, Zhang X, et al. Efficacy and persistence of allogeneic adipose-derived mesenchymal stem cells combined with hyaluronic acid in osteoarthritis after intra-articular injection in a sheep model. Tissue Eng Part A. 2018;24:219–33. doi: 10.1089/ten.tea.2017.0039. [DOI] [PubMed] [Google Scholar]
- 110.Barrachina L, Remacha AR, Romero A, Vitoria A, Albareda J, Prades M, et al. Assessment of effectiveness and safety of repeat administration of proinflammatory primed allogeneic mesenchymal stem cells in an equine model of chemically induced osteoarthritis. BMC Vet Res. 2018;14:241. doi: 10.1186/s12917-018-1556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Health Canada Approves Feraheme® (ferumoxytol) to Treat Iron Deficiency Anemia in Adults with Chronic Kidney Disease [Internet]. 2011 [cited 2022 Dec 28]. Available from: https://www.businesswire.com/news/home/20111212005685/en/Health-Canada-Approves-Feraheme%C2%AE-ferumoxytol-to-Treat-Iron-Deficiency-Anemia-in-Adults-with-Chronic-Kidney-Disease
- 112.Oh J, Son YS, Kim WH, Kwon OK, Kang BJ. Mesenchymal stem cells genetically engineered to express platelet-derived growth factor and heme oxygenase-1 ameliorate osteoarthritis in a canine model. J Orthop Surg Res. 2021;16:43. doi: 10.1186/s13018-020-02178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vincent TL. Mechanoflammation in osteoarthritis pathogenesis. Semin Arthritis Rheum. 2019;49:S36–8. doi: 10.1016/j.semarthrit.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 114.Meehan RT, Regan EA, Hoffman ED, Wolf ML, Gill MT, Crooks JL, et al. Synovial fluid cytokines, chemokines and MMP levels in osteoarthritis patients with knee pain display a profile similar to many rheumatoid arthritis patients. J Clin Med. 2021;10:5027. doi: 10.3390/jcm10215027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roze RH, Bierma-Zeinstra SMA, Agricola R, Oei EHG, Waarsing JH. Differences in MRI features between two different osteoarthritis subpopulations: data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2016;24:822–6. doi: 10.1016/j.joca.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 116.Krampera M. Mesenchymal stromal cell “licensing”: a multistep process. Leukemia. 2011;25:1408–14. doi: 10.1038/leu.2011.108. [DOI] [PubMed] [Google Scholar]
- 117.Kwon DG, Kim MK, Jeon YS, Nam YC, Park JS, Ryu DJ. State of the art: the immunomodulatory role of MSCs for osteoarthritis. Int J Mol Sci. 2022;23:1618. doi: 10.3390/ijms23031618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Markov A, Thangavelu L, Aravindhan S, Zekiy AO, Jarahian M, Chartrand MS, et al. Mesenchymal stem/stromal cells as a valuable source for the treatment of immune-mediated disorders. Stem Cell Res Ther. 2021;12:192. doi: 10.1186/s13287-021-02265-1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 119.Chahal J, Gómez-Aristizábal A, Shestopaloff K, Bhatt S, Chaboureau A, Fazio A, et al. Bone marrow mesenchymal stromal cell treatment in patients with osteoarthritis results in overall improvement in pain and symptoms and reduces synovial inflammation. Stem Cells Transl Med. 2019;8:746–57. doi: 10.1002/sctm.18-0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Li J, Shao Q, Zhu X, Sun G. Efficacy of autologous bone marrow mesenchymal stem cells in the treatment of knee osteoarthritis and their effects on the expression of serum TNF-α and IL-6. J Musculoskelet Neuronal Interact. 2020;20:128–35. [PMC free article] [PubMed] [Google Scholar]
- 121.Sadri B, Tamimi A, Nouraein S, Bagheri Fard A, Mohammadi J, Mohammadpour M, et al. Clinical and laboratory findings following transplantation of allogeneic adipose-derived mesenchymal stromal cells in knee osteoarthritis, a brief report. Connect Tissue Res. 2022;63:663–74. doi: 10.1080/03008207.2022.2074841. [DOI] [PubMed] [Google Scholar]
- 122.Conaghan PG, Hunter DJ, Maillefert JF, Reichmann WM, Losina E. Summary and recommendations of the OARSI FDA osteoarthritis Assessment of Structural Change Working Group. Osteoarthr Cartil. 2011;19:606–10. doi: 10.1016/j.joca.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hunter DJ, Guermazi A, Roemer F, Zhang Y, Neogi T. Structural correlates of pain in joints with osteoarthritis. Osteoarthr Cartil. 2013;21:1170–8. doi: 10.1016/j.joca.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 124.Eitner A, Hofmann GO, Schaible HG. Mechanisms of Osteoarthritic pain. Studies in humans and experimental models. Front Mol Neurosci [Internet]. 2017 [cited 2023 Jan 7];10. Available from: https://www.frontiersin.org/articles/10.3389/fnmol.2017.00349 [DOI] [PMC free article] [PubMed]
- 125.O’Neill TW, Felson DT. Mechanisms of Osteoarthritis (OA) Pain. Curr Osteoporos Rep. 2018;16:611–6. doi: 10.1007/s11914-018-0477-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Song Y, Du H, Dai C, Zhang L, Li S, Hunter DJ, et al. Human adipose-derived mesenchymal stem cells for osteoarthritis: a pilot study with long-term follow-up and repeated injections. Regen Med. 2018;13:295–307. doi: 10.2217/rme-2017-0152. [DOI] [PubMed] [Google Scholar]
- 127.Chen HH, Chen YC, Yu SN, Lai WL, Shen YS, Shen PC, et al. Infrapatellar fat pad-derived mesenchymal stromal cell product for treatment of knee osteoarthritis: a first-in-human study with evaluation of the potency marker. Cytotherapy. 2022;24:72–85. doi: 10.1016/j.jcyt.2021.08.006. [DOI] [PubMed] [Google Scholar]
- 128.Orozco L, Munar A, Soler R, Alberca M, Soler F, Huguet M, et al. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: a pilot study. Transplantation. 2013;95:1535–41. doi: 10.1097/TP.0b013e318291a2da. [DOI] [PubMed] [Google Scholar]
- 129.Soler Rich R, Munar A, Soler Romagosa F, Peirau X, Huguet M, Alberca M, García SA, Sancho JL. Treatment of knee osteoarthritis with autologous expanded bone marrow mesenchymal stem cells: 50 cases clinical and MRI results at one year follow-up. J Stem Cell Res Ther. 2015;5:1–7.
- 130.Soler R, Orozco L, Munar A, Huguet M, López R, Vives J, et al. Final results of a phase I-II trial using ex vivo expanded autologous Mesenchymal Stromal Cells for the treatment of osteoarthritis of the knee confirming safety and suggesting cartilage regeneration. Knee. 2016;23:647–54. doi: 10.1016/j.knee.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 131.Al-Najar M, Khalil H, Al-Ajlouni J, Al-Antary E, Hamdan M, Rahmeh R, et al. Intra-articular injection of expanded autologous bone marrow mesenchymal cells in moderate and severe knee osteoarthritis is safe: a phase I/II study. J Orthop Surg Res. 2017;12:190. doi: 10.1186/s13018-017-0689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhao X, Ruan J, Tang H, Li J, Shi Y, Li M, et al. Multi-compositional MRI evaluation of repair cartilage in knee osteoarthritis with treatment of allogeneic human adipose-derived mesenchymal progenitor cells. Stem Cell Res Ther. 2019;10:308. doi: 10.1186/s13287-019-1406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lu L, Dai C, Du H, Li S, Ye P, Zhang L, et al. Intra-articular injections of allogeneic human adipose-derived mesenchymal progenitor cells in patients with symptomatic bilateral knee osteoarthritis: a Phase I pilot study. Regen Med. 2020;15:1625–36. doi: 10.2217/rme-2019-0106. [DOI] [PubMed] [Google Scholar]
- 134.Park YB, Ha CW, Lee CH, Yoon YC, Park YG. Cartilage regeneration in osteoarthritic patients by a composite of allogeneic umbilical cord blood-derived mesenchymal stem cells and hyaluronate hydrogel: results from a clinical trial for safety and proof-of-concept with 7 years of extended follow-up: MSCs for cartilage regeneration in osteoarthritis. Stem Cells Transl Med. 2017;6:613–21. doi: 10.5966/sctm.2016-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cosenza S, Ruiz M, Toupet K, Jorgensen C, Noël D. Mesenchymal stem cells derived exosomes and microparticles protect cartilage and bone from degradation in osteoarthritis. Sci Rep. 2017;7:16214. doi: 10.1038/s41598-017-15376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ruiz M, Toupet K, Maumus M, Rozier P, Jorgensen C, Noël D. TGFBI secreted by mesenchymal stromal cells ameliorates osteoarthritis and is detected in extracellular vesicles. Biomaterials. 2020;226:119544. doi: 10.1016/j.biomaterials.2019.119544. [DOI] [PubMed] [Google Scholar]
- 137.Wang R, Maimaitijuma T, Ma YY, Jiao Y, Cao YP. Mitochondrial transfer from bone-marrow-derived mesenchymal stromal cells to chondrocytes protects against cartilage degenerative mitochondrial dysfunction in rats chondrocytes. Chin Med J (Engl) 2021;134:212–8. doi: 10.1097/CM9.0000000000001057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wu J, Kuang L, Chen C, Yang J, Zeng WN, Li T, et al. miR-100-5p-abundant exosomes derived from infrapatellar fat pad MSCs protect articular cartilage and ameliorate gait abnormalities via inhibition of mTOR in osteoarthritis. Biomaterials. 2019;206:87–100. doi: 10.1016/j.biomaterials.2019.03.022. [DOI] [PubMed] [Google Scholar]
- 139.Shin L, Peterson DA. Human mesenchymal stem cell grafts enhance normal and impaired wound healing by recruiting existing endogenous tissue stem/progenitor cells. Stem Cells Transl Med. 2013;2:33–42. doi: 10.5966/sctm.2012-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Meretoja VV, Dahlin RL, Wright S, Kasper FK, Mikos AG. Articular chondrocyte redifferentiation in 3D co-cultures with mesenchymal stem cells. Tissue Eng Part C Methods. 2014;20:514–23. doi: 10.1089/ten.tec.2013.0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kim YG, Choi J, Kim K. Mesenchymal stem cell-derived exosomes for effective cartilage tissue repair and treatment of osteoarthritis. Biotechnol J. 2020;15:e2000082. doi: 10.1002/biot.202000082. [DOI] [PubMed] [Google Scholar]
- 142.Gupta PK, Krishna M, Chullikana A, Desai S, Murugesan R, Dutta S, et al. Administration of adult human bone marrow-derived, cultured, pooled, allogeneic mesenchymal stromal cells in critical limb ischemia due to Buerger’s disease: phase II study report suggests clinical efficacy. Stem Cells Transl Med. 2017;6:689–99. doi: 10.5966/sctm.2016-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ashraf S, Walsh DA. Angiogenesis in osteoarthritis. Curr Opin Rheumatol. 2008;20:573–80. doi: 10.1097/BOR.0b013e3283103d12. [DOI] [PubMed] [Google Scholar]
- 144.Nagao M, Hamilton JL, Kc R, Berendsen AD, Duan X, Cheong CW, et al. Vascular endothelial growth factor in cartilage development and osteoarthritis. Sci Rep. 2017;7:13027. doi: 10.1038/s41598-017-13417-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yan D, Chen D, Cool SM, van Wijnen AJ, Mikecz K, Murphy G, et al. Fibroblast growth factor receptor 1 is principally responsible for fibroblast growth factor 2-induced catabolic activities in human articular chondrocytes. Arthritis Res Ther. 2011;13:R130. doi: 10.1186/ar3441. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 146.Laudy ABM, Bakker EWP, Rekers M, Moen MH. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med. 2015;49:657–72. doi: 10.1136/bjsports-2014-094036. [DOI] [PubMed] [Google Scholar]
- 147.Filardo G, Previtali D, Napoli F, Candrian C, Zaffagnini S, Grassi A. PRP injections for the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Cartilage. 2021;13:364S–75S. doi: 10.1177/1947603520931170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Belk JW, Kraeutler MJ, Houck DA, Goodrich JA, Dragoo JL, McCarty EC. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49:249–60. doi: 10.1177/0363546520909397. [DOI] [PubMed] [Google Scholar]
- 149.Corliss BA, Azimi MS, Munson J, Peirce SM, Murfee WL. Macrophages: an inflammatory link between angiogenesis and lymphangiogenesis. Microcirculation. 2016;23:95–121. doi: 10.1111/micc.12259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Boregowda SV, Krishnappa V, Haga CL, Ortiz LA, Phinney DG. A clinical indications prediction scale based on TWIST1 for human mesenchymal stem cells. EBioMedicine. 2015;4:62–73. doi: 10.1016/j.ebiom.2015.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Chambers DC, Enever D, Ilic N, Sparks L, Whitelaw K, Ayres J, et al. A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology. 2014;19:1013–8. doi: 10.1111/resp.12343. [DOI] [PubMed] [Google Scholar]
- 152.Karantalis V, DiFede DL, Gerstenblith G, Pham S, Symes J, Zambrano JP, et al. Autologous mesenchymal stem cells produce concordant improvements in regional function, tissue perfusion, and fibrotic burden when administered to patients undergoing coronary artery bypass grafting. Circ Res. 2014;114:1302–10. doi: 10.1161/CIRCRESAHA.114.303180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rim YA, Ju JH. The role of fibrosis in osteoarthritis progression. Life (Basel) 2020;11:3. doi: 10.3390/life11010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rockel JS, Rabani R, Viswanathan S. Anti-fibrotic mechanisms of exogenously-expanded mesenchymal stromal cells for fibrotic diseases. Semin Cell Dev Biol. 2020;101:87–103. doi: 10.1016/j.semcdb.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 155.ter Huurne M, Schelbergen R, Blattes R, Blom A, de Munter W, Grevers LC, et al. Antiinflammatory and chondroprotective effects of intraarticular injection of adipose-derived stem cells in experimental osteoarthritis. Arthritis Rheum. 2012;64:3604–13. doi: 10.1002/art.34626. [DOI] [PubMed] [Google Scholar]
- 156.Ibáñez L, Guillem-Llobat P, Marín M, Guillén MI. Connection between mesenchymal stem cells therapy and osteoclasts in osteoarthritis. Int J Mol Sci. 2022;23:4693. doi: 10.3390/ijms23094693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Tofiño-Vian M, Guillén MI, Pérez del Caz MD, Castejón MA, Alcaraz MJ. Extracellular vesicles from adipose-derived mesenchymal stem cells downregulate senescence features in osteoarthritic osteoblasts. Oxid Med Cell Longev. 2017;2017:7197598. doi: 10.1155/2017/7197598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60:831–9. doi: 10.1002/art.24383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ramos-Mucci L, Javaheri B, van ‘t Hof R, Bou-Gharios G, Pitsillides AA, Comerford E, et al. Meniscal and ligament modifications in spontaneous and post-traumatic mouse models of osteoarthritis. Arthritis Res Ther. 2020;22:171. doi: 10.1186/s13075-020-02261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chamberlain CS, Saether EE, Aktas E, Vanderby R. Mesenchymal stem cell therapy on tendon/ligament healing. J Cytokine Biol. 2017;2:112. doi: 10.4172/2576-3881.1000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yu H, Adesida AB, Jomha NM. Meniscus repair using mesenchymal stem cells—a comprehensive review. Stem Cell Res Ther. 2015;6:86. doi: 10.1186/s13287-015-0077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kuznetsov SA, Mankani MH, Bianco P, Robey PG. Enumeration of the colony-forming units–fibroblast from mouse and human bone marrow in normal and pathological conditions. Stem Cell Res. 2009;2:83–94. doi: 10.1016/j.scr.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang J, Liao L, Wang S, Tan J. Cell therapy with autologous mesenchymal stem cells-how the disease process impacts clinical considerations. Cytotherapy. 2013;15:893–904. doi: 10.1016/j.jcyt.2013.01.218. [DOI] [PubMed] [Google Scholar]
- 164.Siegel G, Kluba T, Hermanutz-Klein U, Bieback K, Northoff H, Schäfer R. Phenotype, donor age and gender affect function of human bone marrow-derived mesenchymal stromal cells. BMC Med. 2013;11:146. doi: 10.1186/1741-7015-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Serena C, Keiran N, Ceperuelo-Mallafre V, Ejarque M, Fradera R, Roche K, et al. Obesity and type 2 diabetes alters the immune properties of human adipose derived stem cells. Stem Cells. 2016;34:2559–73. doi: 10.1002/stem.2429. [DOI] [PubMed] [Google Scholar]
- 166.Wilson A, Hodgson-Garms M, Frith JE, Genever P. Multiplicity of mesenchymal stromal cells: finding the right route to therapy. Front Immunol. 2019;10:1112. doi: 10.3389/fimmu.2019.01112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yin JQ, Zhu J, Ankrum JA. Manufacturing of primed mesenchymal stromal cells for therapy. Nat Biomed Eng. 2019;3:90–104. doi: 10.1038/s41551-018-0325-8. [DOI] [PubMed] [Google Scholar]
- 168.Frontiers | Senescence in Mesenchymal Stem Cells: Functional Alterations, Molecular Mechanisms, and Rejuvenation Strategies [Internet]. [cited 2022 Dec 22]. Available from: https://www.frontiersin.org/articles/10.3389/fcell.2020.00258/full [DOI] [PMC free article] [PubMed]
- 169.Wiese DM, Ruttan CC, Wood CA, Ford BN, Braid LR. Accumulating transcriptome drift precedes cell aging in human umbilical cord-derived mesenchymal stromal cells serially cultured to replicative senescence. Stem Cells Transl Med. 2019;8:945–58. doi: 10.1002/sctm.18-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Park YW, Kang YM, Butterfield J, Detmar M, Goronzy JJ, Weyand CM. Thrombospondin 2 functions as an endogenous regulator of angiogenesis and inflammation in rheumatoid arthritis. Am J Pathol. 2004;165:2087–98. doi: 10.1016/S0002-9440(10)63259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Baust JM, Van Buskirk R, Baust JG. Gene activation of the apoptotic caspase cascade following cryogenic storage. Cell Preserv Technol. 2002;1:63–80. doi: 10.1089/15383440260073301. [DOI] [Google Scholar]
- 172.François M, Copland IB, Yuan S, Romieu-Mourez R, Waller EK, Galipeau J. Cryopreserved mesenchymal stromal cells display impaired immunosuppressive properties as a result of heat-shock response and impaired interferon-γ licensing. Cytotherapy. 2012;14:147–52. doi: 10.3109/14653249.2011.623691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Cottle C, Porter AP, Lipat A, Turner-Lyles C, Nguyen J, Moll G, et al. Impact of cryopreservation and freeze-thawing on therapeutic properties of mesenchymal stromal/stem cells and other common cellular therapeutics. Curr Stem Cell Rep. 2022;8:72–92. doi: 10.1007/s40778-022-00212-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Antebi B, Asher AM, Rodriguez LA, Moore RK, Mohammadipoor A, Cancio LC. Cryopreserved mesenchymal stem cells regain functional potency following a 24-h acclimation period. J Transl Med. 2019;17:297. doi: 10.1186/s12967-019-2038-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lim HC, Park YB, Ha CW, Cole BJ, Lee BK, Jeong HJ, et al. Allogeneic umbilical cord blood–derived mesenchymal stem cell implantation versus microfracture for large, full-thickness cartilage defects in older patients: a multicenter randomized clinical trial and extended 5-year clinical follow-up. Orthop J Sports Med. 2021;9:2325967120973052. doi: 10.1177/2325967120973052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ménard C, Dulong J, Roulois D, Hébraud B, Verdière L, Pangault C, et al. Integrated transcriptomic, phenotypic, and functional study reveals tissue-specific immune properties of mesenchymal stromal cells. Stem Cells. 2020;38:146–59. doi: 10.1002/stem.3077. [DOI] [PubMed] [Google Scholar]
- 177.Binch ALA, Richardson SM, Hoyland JA, Barry FP. Combinatorial conditioning of adipose derived‐mesenchymal stem cells enhances their neurovascular potential: Implications for intervertebral disc degeneration. JOR Spine. 2019;2:e1072. doi: 10.1002/jsp2.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wiese DM, Wood CA, Ford BN, Braid LR. Cytokine activation reveals tissue-imprinted gene profiles of mesenchymal stromal cells. Front Immunol [Internet]. 2022 [cited 2022 Dec 22];13. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2022.917790 [DOI] [PMC free article] [PubMed]
- 179.Mattar P, Bieback K. Comparing the immunomodulatory properties of bone marrow, adipose tissue, and birth-associated tissue mesenchymal stromal cells. Front Immunol. 2015;6:560. doi: 10.3389/fimmu.2015.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zhao D, Pan JK, Yang WY, Han YH, Zeng LF, Liang GH, et al. Intra-articular injections of platelet-rich plasma, adipose mesenchymal stem cells, and bone marrow mesenchymal stem cells associated with better outcomes than hyaluronic acid and saline in knee osteoarthritis: a systematic review and network meta-analysis. Arthroscopy. 2021;37:2298–314.e10. doi: 10.1016/j.arthro.2021.02.045. [DOI] [PubMed] [Google Scholar]
- 181.Han X, Yang B, Zou F, Sun J. Clinical therapeutic efficacy of mesenchymal stem cells derived from adipose or bone marrow for knee osteoarthritis: a meta-analysis of randomized controlled trials. J Comp Eff Res. 2020;9:361–74. doi: 10.2217/cer-2019-0187. [DOI] [PubMed] [Google Scholar]
- 182.Suh K, Cole BJ, Gomoll A, Lee SM, Choi H, Ha CW, et al. Cost effectiveness of allogeneic umbilical cord blood-derived mesenchymal stem cells in patients with knee osteoarthritis. Appl Health Econ Health Policy. 2023;21:141–52. [DOI] [PMC free article] [PubMed]
- 183.Barrachina L, Cequier A, Romero A, Vitoria A, Zaragoza P, Vázquez FJ, et al. Allo-antibody production after intraarticular administration of mesenchymal stem cells (MSCs) in an equine osteoarthritis model: effect of repeated administration, MSC inflammatory stimulation, and equine leukocyte antigen (ELA) compatibility. Stem Cell Res Ther. 2020;11:52. doi: 10.1186/s13287-020-1571-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Rosa G dos S, Krieck AMT, Padula ET, Stievani F de C, et al. Production of cytotoxic antibodies after intra-articular injection of allogeneic synovial membrane mesenchymal stem cells with and without LPS administration. Front Immunol [Internet]. 2022 [cited 2022 Dec 22];13. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2022.871216 [DOI] [PMC free article] [PubMed]
- 185.Wang Y, Shimmin A, Ghosh P, Marks P, Linklater J, Connell D, et al. Safety, tolerability, clinical, and joint structural outcomes of a single intra-articular injection of allogeneic mesenchymal precursor cells in patients following anterior cruciate ligament reconstruction: a controlled double-blind randomised trial. Arthritis Res Ther. 2017;19:180. doi: 10.1186/s13075-017-1391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Gnani D, Crippa S, Della Volpe L, Rossella V, Conti A, Lettera E, et al. An early-senescence state in aged mesenchymal stromal cells contributes to hematopoietic stem and progenitor cell clonogenic impairment through the activation of a pro-inflammatory program. Aging Cell. 2019;18:e12933. doi: 10.1111/acel.12933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.University of Wisconsin, Madison. Pilot Study of Mesenchymal Stromal Cells in Patients With Xerostomia After Radiation Therapy for Head and Neck Cancer [Internet]. clinicaltrials.gov; 2022 Nov [cited 2022 Dec 27]. Report No.: NCT04489732. Available from: https://clinicaltrials.gov/ct2/show/NCT04489732
- 188.Grezella C, Fernandez-Rebollo E, Franzen J, Ventura Ferreira MS, Beier F, Wagner W. Effects of senolytic drugs on human mesenchymal stromal cells. Stem Cell Res Ther. 2018;9:108. doi: 10.1186/s13287-018-0857-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Nakahara F, Borger DK, Wei Q, Pinho S, Maryanovich M, Zahalka AH, et al. Engineering a haematopoietic stem cell niche by revitalizing mesenchymal stromal cells. Nat Cell Biol. 2019;21:560–7. doi: 10.1038/s41556-019-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mobasheri A, Bay-Jensen AC, Gualillo O, Larkin J, Levesque MC, Henrotin Y. Soluble biochemical markers of osteoarthritis: are we close to using them in clinical practice? Best Pract Res Clin Rheumatol. 2017;31:705–20. doi: 10.1016/j.berh.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 191.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil. 2010;18:476–99. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 192.Sellam J, Berenbaum F. The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol. 2010;6:625–35. doi: 10.1038/nrrheum.2010.159. [DOI] [PubMed] [Google Scholar]
- 193.Mathiessen A, Conaghan PG. Synovitis in osteoarthritis: current understanding with therapeutic implications. Arthritis Res Ther. 2017;19:18. doi: 10.1186/s13075-017-1229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kloppenburg M, Ramonda R, Kwok WY, Bobacz K, Elewaut D, Frallonardo P, et al. OP0095 randomized, placebo-controlled trial to evaluate clinical efficacy and structure modifying properties of subcutaneous etanercept (ETN) in patients with erosive inflammatory hand osteoarthritis (OA) Ann Rheum Dis. 2016;75:90–1. doi: 10.1136/annrheumdis-2016-eular.3663. [DOI] [Google Scholar]
- 195.de Lange-Brokaar BJE, Ioan-Facsinay A, Yusuf E, Visser AW, Kroon HM, Andersen SN, et al. Degree of synovitis on MRI by comprehensive whole knee semi-quantitative scoring method correlates with histologic and macroscopic features of synovial tissue inflammation in knee osteoarthritis. Osteoarthr Cartil. 2014;22:1606–13. doi: 10.1016/j.joca.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 196.Sarmanova A, Hall M, Moses J, Doherty M, Zhang W. Synovial changes detected by ultrasound in people with knee osteoarthritis - a meta-analysis of observational studies. Osteoarthr Cartil. 2016;24:1376–83. doi: 10.1016/j.joca.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Siebuhr AS, Bay-Jensen AC, Jordan JM, Kjelgaard-Petersen CF, Christiansen C, Abramson SB, et al. Inflammation (or synovitis)-driven osteoarthritis: an opportunity for personalizing prognosis and treatment? Scand J Rheumatol. 2016;45:87–98. doi: 10.3109/03009742.2015.1060259. [DOI] [PubMed] [Google Scholar]
- 198.Koski JM, Saarakkala S, Helle M, Hakulinen U, Heikkinen JO, Hermunen H. Power Doppler ultrasonography and synovitis: correlating ultrasound imaging with histopathological findings and evaluating the performance of ultrasound equipments. Ann Rheum Dis. 2006;65:1590–5. doi: 10.1136/ard.2005.051235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Yager N, Cole S, Lledo Lara A, Maroof A, Penkava F, Knight JC, et al. Ex vivo mass cytometry analysis reveals a profound myeloid proinflammatory signature in psoriatic arthritis synovial fluid. Ann Rheum Dis. 2021;80:1559–67. doi: 10.1136/annrheumdis-2021-220280. [DOI] [PubMed] [Google Scholar]
- 200.Rosshirt N, Hagmann S, Tripel E, Gotterbarm T, Kirsch J, Zeifang F, et al. A predominant Th1 polarization is present in synovial fluid of end-stage osteoarthritic knee joints: analysis of peripheral blood, synovial fluid and synovial membrane. Clin Exp Immunol. 2019;195:395–406. doi: 10.1111/cei.13230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Penatti A, Facciotti F, De Matteis R, Larghi P, Paroni M, Murgo A, et al. Differences in serum and synovial CD4+ T cells and cytokine profiles to stratify patients with inflammatory osteoarthritis and rheumatoid arthritis. Arthritis Res Ther. 2017;19:103. doi: 10.1186/s13075-017-1305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Krampera M, Le Blanc K. Mesenchymal stromal cells: putative microenvironmental modulators become cell therapy. Cell Stem Cell. 2021;28:1708–25. doi: 10.1016/j.stem.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 203.Ali SA, Espin-Garcia O, Wong AK, Potla P, Pastrello C, McIntyre M, et al. Circulating microRNAs differentiate fast-progressing from slow-progressing and non-progressing knee osteoarthritis in the Osteoarthritis Initiative cohort. Therapeutic Adv Musculoskelet. 2022;14:1759720X221082917. doi: 10.1177/1759720X221082917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Deciphering osteoarthritis genetics across 826,690 individuals from 9 populations - PubMed [Internet]. [cited 2022 Dec 22]. Available from: https://pubmed.ncbi.nlm.nih.gov/34450027/
- 205.Ali N, Turkiewicz A, Hughes V, Folkesson E, Tjörnstand J, Neuman P, et al. Proteomics profiling of human synovial fluid suggests increased protein interplay in early-osteoarthritis (OA) that is lost in late-stage OA. Mol Cell Proteom. 2022;21:100200. doi: 10.1016/j.mcpro.2022.100200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Costello CA, Rockel JS, Liu M, Gandhi R, Perruccio AV, Rampersaud YR, et al. Individual participant data meta-analysis of metabolomics on sustained knee pain in primary osteoarthritis patients. Rheumatology (Oxford). 2022;keac545. [DOI] [PMC free article] [PubMed]
- 207.Beier F. The impact of omics research on our understanding of osteoarthritis and future treatments. Curr Opin Rheumatol. 2023;35:55. doi: 10.1097/BOR.0000000000000919. [DOI] [PubMed] [Google Scholar]
- 208.Banh L, Cheung KK, Chan MWY, Young EWK, Viswanathan S. Advances in organ-on-a-chip systems for modelling joint tissue and osteoarthritic diseases. Osteoarthr Cartil. 2022;30:1050–61. doi: 10.1016/j.joca.2022.03.012. [DOI] [PubMed] [Google Scholar]
- 209.Galipeau J, Krampera M, Barrett J, Dazzi F, Deans RJ, DeBruijn J, et al. International Society for Cellular Therapy perspective on immune functional assays for mesenchymal stromal cells as potency release criterion for advanced phase clinical trials. Cytotherapy. 2016;18:151–9. doi: 10.1016/j.jcyt.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Lee M, Kim GH, Kim M, Seo JM, Kim YM, Seon MR, et al. PTX-3 secreted by intra-articular-injected SMUP-cells reduces pain in an osteoarthritis rat model. Cells. 2021;10:2420. doi: 10.3390/cells10092420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Medipost Co Ltd. A Open, Single-center, Phase 1 Trial to Evaluate Safety and Explore Efficacy of SMUP-IA-01 in Patients With Knee Osteoarthritis [Internet]. clinicaltrials.gov; 2021 Feb [cited 2022 Dec 21]. Report No.: NCT04037345. Available from: https://clinicaltrials.gov/ct2/show/NCT04037345
- 212.Amin HD, Brady MA, St-Pierre JP, Stevens MM, Overby DR, Ethier CR. Stimulation of chondrogenic differentiation of adult human bone marrow-derived stromal cells by a moderate-strength static magnetic field. Tissue Eng Part A. 2014;20:1612–20. doi: 10.1089/ten.tea.2013.0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Huang J, Liang Y, Huang Z, Zhao P, Liang Q, Liu Y, et al. Magnetic enhancement of chondrogenic differentiation of mesenchymal stem cells. ACS Biomater Sci Eng. 2019;5:2200–7. doi: 10.1021/acsbiomaterials.9b00025. [DOI] [PubMed] [Google Scholar]
- 214.Zhu C, Wu W, Qu X. Mesenchymal stem cells in osteoarthritis therapy: a review. Am J Transl Res. 2021;13:448–61. [PMC free article] [PubMed] [Google Scholar]
- 215.Liu X, Robbins S, Wang X, Virk S, Schuck K, Deveza LA, et al. Efficacy and cost-effectiveness of Stem Cell injections for symptomatic relief and strUctural improvement in people with Tibiofemoral knee OsteoaRthritis: protocol for a randomised placebo-controlled trial (the SCUlpTOR trial) BMJ Open. 2021;11:e056382. doi: 10.1136/bmjopen-2021-056382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Bloor AJC, Patel A, Griffin JE, Gilleece MH, Radia R, Yeung DT, et al. Production, safety and efficacy of iPSC-derived mesenchymal stromal cells in acute steroid-resistant graft versus host disease: a phase I, multicenter, open-label, dose-escalation study. Nat Med. 2020;26:1720–5. doi: 10.1038/s41591-020-1050-x. [DOI] [PubMed] [Google Scholar]
- 217.Ben-David U, Gan QF, Golan-Lev T, Arora P, Yanuka O, Oren YS, et al. Selective elimination of human pluripotent stem cells by an oleate synthesis inhibitor discovered in a high-throughput screen. Cell Stem Cell. 2013;12:167–79. doi: 10.1016/j.stem.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 218.Menendez S, Camus S, Herreria A, Paramonov I, Morera LB, Collado M, et al. Increased dosage of tumor suppressors limits the tumorigenicity of iPS cells without affecting their pluripotency. Aging Cell. 2012;11:41–50. doi: 10.1111/j.1474-9726.2011.00754.x. [DOI] [PubMed] [Google Scholar]
- 219.Liang Q, Monetti C, Shutova MV, Neely EJ, Hacibekiroglu S, Yang H, et al. Linking a cell-division gene and a suicide gene to define and improve cell therapy safety. Nature. 2018;563:701–4. doi: 10.1038/s41586-018-0733-7. [DOI] [PubMed] [Google Scholar]
- 220.Castro-Viñuelas R, Sanjurjo-Rodríguez C, Piñeiro-Ramil M, Hermida-Gómez T, Fuentes-Boquete IM, de Toro-Santos FJ, et al. Induced pluripotent stem cells for cartilage repair: current status and future perspectives. Eur Cell Mater. 2018;36:96–109. doi: 10.22203/eCM.v036a08. [DOI] [PubMed] [Google Scholar]
- 221.Harding J, Vintersten-Nagy K, Shutova M, Yang H, Tang JK, Massumi M, et al. Induction of long-term allogeneic cell acceptance and formation of immune privileged tissue in immunocompetent hosts [Internet]. bioRxiv; 2019 [cited 2022 Dec 28]. p. 716571. Available from: https://www.biorxiv.org/content/10.1101/716571v1
- 222.Jin Z, Ren J, Qi S. Exosomal miR-9-5p secreted by bone marrow-derived mesenchymal stem cells alleviates osteoarthritis by inhibiting syndecan-1. Cell Tissue Res. 2020;381:99–114. doi: 10.1007/s00441-020-03193-x. [DOI] [PubMed] [Google Scholar]
- 223.Jin Z, Ren J, Qi S. Human bone mesenchymal stem cells-derived exosomes overexpressing microRNA-26a-5p alleviate osteoarthritis via down-regulation of PTGS2. Int Immunopharmacol. 2020;78:105946. doi: 10.1016/j.intimp.2019.105946. [DOI] [PubMed] [Google Scholar]
- 224.Herrmann IK, Wood MJA, Fuhrmann G. Extracellular vesicles as a next-generation drug delivery platform. Nat Nanotechnol. 2021;16:748–59. doi: 10.1038/s41565-021-00931-2. [DOI] [PubMed] [Google Scholar]
- 225.Tang TT, Wang B, Lv LL, Liu BC. Extracellular vesicle-based Nanotherapeutics: emerging frontiers in anti-inflammatory therapy. Theranostics. 2020;10:8111–29. doi: 10.7150/thno.47865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Tang TT, Wang B, Wu M, Li ZL, Feng Y, Cao JY, et al. Extracellular vesicle–encapsulated IL-10 as novel nanotherapeutics against ischemic AKI. Sci Adv. 2020;6:eaaz0748. doi: 10.1126/sciadv.aaz0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Thomas MJ, Neogi T. Flare-ups of osteoarthritis: what do they mean in the short-term and the long-term? Osteoarthr Cartil. 2020;28:870–3. doi: 10.1016/j.joca.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Guillemin F, Ricatte C, Barcenilla-Wong A, Schoumacker A, Cross M, Alleyrat C, et al. Developing a preliminary definition and domains of flare in knee and hip osteoarthritis (OA): consensus building of the flare-in-OA OMERACT group. J Rheumatol. 2019;46:1188–91. doi: 10.3899/jrheum.181085. [DOI] [PubMed] [Google Scholar]
- 229.Sharma L, Chang AH, Jackson RD, Nevitt M, Moisio KC, Hochberg M, et al. Varus thrust and incident and progressive knee osteoarthritis. Arthritis Rheumatol. 2017;69:2136–43. doi: 10.1002/art.40224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Zeni JA, Flowers P, Bade M, Cheuy V, Stevens-Lapsley J, Snyder-Mackler L. Stiff knee gait may increase risk of second total knee arthroplasty. J Orthop Res. 2019;37:397–402. doi: 10.1002/jor.24175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Omori G, Narumi K, Nishino K, Nawata A, Watanabe H, Tanaka M, et al. Association of mechanical factors with medial knee osteoarthritis: a cross-sectional study from Matsudai Knee Osteoarthritis Survey. J Orthop Sci. 2016;21:463–8. doi: 10.1016/j.jos.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 232.guideline-clinical-investigation-medicinal-products-used-treatment-osteoarthritis_en.pdf [Internet]. [cited 2023 Jan 7]. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-used-treatment-osteoarthritis_en.pdf
- 233.Osteoarthritis: Structural Endpoints for the Development of Drugs, Devices, and Biological Products for Treatment Guidance for Industry. 2018. https://www.fda.gov/media/71132/download
- 234.Joseph GB, Nevitt MC, McCulloch CE, Neumann J, Lynch JA, Heilmeier U, et al. Associations between molecular biomarkers and MR-based cartilage composition and knee joint morphology: data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2018;26:1070–7. doi: 10.1016/j.joca.2018.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Piuzzi NS, Ng M, Chughtai M, Khlopas A, Ng K, Mont MA, et al. The stem-cell market for the treatment of knee osteoarthritis: a patient perspective. J Knee Surg. 2018;31:551–6. doi: 10.1055/s-0037-1604443. [DOI] [PubMed] [Google Scholar]
- 236.McDougall JA, Furnback WE, Wang BCM, Mahlich J. Understanding the global measurement of willingness to pay in health. J Mark Access Health Policy. 2020;8:1717030. doi: 10.1080/20016689.2020.1717030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Clinical Trials: Kolon TissueGene, Inc. (950160) [Internet]. Kolon TissueGene, Inc. [cited 2023 Jan 6]. Available from: https://www.tissuegene.com/en_US/clinical-trials
- 238.Marks P, Gottlieb S. Balancing safety and innovation for cell-based regenerative medicine. N. Engl J Med. 2018;378:954–9. doi: 10.1056/NEJMsr1715626. [DOI] [PubMed] [Google Scholar]