Abstract
Background
Pre-operative hypoalbuminemia is known to predict negative outcomes for patients undergoing major surgeries. However, various cut-off points for starting exogenous albumin have been recommended.
Objective
This study investigated the association between pre-operative severe hypoalbuminemia, in-hospital death, and length of hospital stay in patients undergoing gastrointestinal surgery.
Methods
A retrospective cohort study using a database analysis was undertaken on hospitalized patients who underwent major gastrointestinal surgery. The pre-operative serum albumin level was classified into three groups: severe hypoalbuminemia (< 2.0 mg/dL) and non-severe hypoalbuminemia (≥ 2.0–3.4 g/dL) and normal level (3.5–5.5 g/dL). To compare between different cut-offs, a sensitivity analysis using another albumin level classification as severe hypoalbuminemia (< 2.5 mg/dL) and non-severe hypoalbuminemia (≥ 2.5–3.4 g/dL) and normal level (3.5–5.5 g/dL) was applied. The primary outcome was post-operative in-hospital death. Propensity-score adjusted regression analyses were applied.
Results
A total of 670 patients were included. Their average age was 57.4 ± 16.3 years, and 56.1% were men. Only 59 patients (8.8%) had severe hypoalbuminemia. Overall, a total of 93 in-hospital deaths (13.9%) occurred among all included patients, but there were 24/59 (40.7%) deaths among patients with severe hypoalbuminemia, 59/302 (19.5%) deaths among patients with non-severe hypoalbuminemia, and 10/309 (3.2%) deaths among patients with normal albumin level. The adjusted odds ratio for post-operative in-hospital death comparing patients with severe hypoalbuminemia and patients with normal albumin level was 8.11 (3.31–19.87; p < 0.001), while the odds ratio for in-hospital death comparing patients with non-severe and patients with normal albumin level was 3.89 (1.87–8.10; p < 0.001). A sensitivity analysis showed similar findings, the odds ratio for in-hospital death for severe hypoalbuminemia (cut-off as < 2.5 g/dL) was 7.44 (3.38–16.36; p < 0.001), while the odds ratio for in-hospital death for severe hypoalbuminemia (cut-off as 2.5–3.4 g/dL) was 3.02 (1.40–6.52; p = 0.005).
Conclusions
Severe pre-operative hypoalbuminemia in patients undergoing gastrointestinal surgery was associated with an increased risk of in-hospital mortality. The risk of death for patients with severe hypoalbuminemia was relatively similar when using different cut-offs such as < 2.0 and <2.5 g/dL.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40801-023-00364-4.
Key Points
| Severe hypoalbuminemia is associated with an increase in post-operative in-hospital death in patients undergoing gastrointestinal surgeries. |
| Different cut-offs for severe hypoalbuminemia as < 2.0 and <2.5 g/dL had similar risks of post-operative in-hospital death. |
| Severe hypoalbuminemia prolongs the length of hospital stays. |
| The findings are important for clinical and policymakers to decide the treatment strategies in patients undergoing gastrointestinal surgeries. |
Introduction
Albumin is a major component of plasma protein in human blood. It maintains vascular permeability and oncotic pressure and exerts platelet aggregation [1]. Serum albumin is commonly used as a biochemical and nutritional marker in pre-operative assessments of patients undergoing cardiac, trauma, and general surgeries [2–5]. It falls rapidly during the first hour after surgery and remains low until the third day [6]. Serum albumin typically decreases by around 33.0% [7]. Patients with hypoalbuminemia preoperatively have higher risks of complications and death and extended hospital stays [2, 8, 9]. A previous study indicated that serum albumin was a predictor of surgical complications, including sepsis, acute renal failure, bleeding, and failed ventilator weaning [10].
Exogenous albumin appears to increase serum albumin [11]. One guideline recommends using albumin injections for patients with hypoalbuminemia before surgery [12]. The serum albumin correction before surgery in patients with hypoalbuminemia might improve their outcomes. Unfortunately, several studies found that exogenous albumin had been inappropriately prescribed in 63.2–96.0% of cases [13–17]. Prescription control strategies are necessary to reduce the inappropriate use of exogenous albumin. Exogenous albumin injections should be considered according to the patient’s clinical conditions and serum albumin levels [13, 15]. Even though the association between lower albumin levels and negative surgical outcomes has been studied, several cut-offs have been applied, such as albumin levels < 2.0, < 2.5, or < 3.4 g/dL [12, 18–21]. In our setting, the pre-operative albumin level of < 2.5 g/dL has been used as a criterion for starting exogenous albumin, which was consistent with some practice recommendations [19, 20]. However, a practice guideline recommended using the albumin level of < 2.0 g/dL for starting exogenous albumin [12]. Our clinicians and policymakers would like to have evidence to decide whether the cut-off pre-operative albumin level could be changed from 2.5 to 2.0 g/dL with no significantly worse clinical outcomes for patients undergoing major surgeries. Thus, we conducted this study to associate the pre-operative albumin level with post-operative in-hospital death and length of hospital stay (LOS) in patients undergoing gastrointestinal (GI) surgery as a case study for major surgery.
Materials and Methods
A retrospective cohort study using the electronic databases of a tertiary hospital was conducted in Thailand. Before the research began, its protocol was approved by the hospital’s ethics committee (RYHREC No. E026/2564).
Data Sources
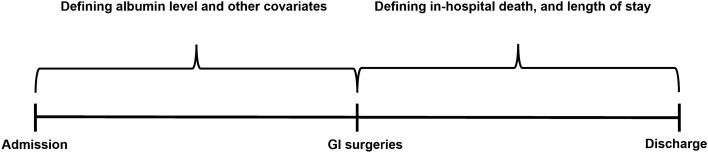
Electronic databases were obtained from a hospital in eastern Thailand. The hospital was a regional hospital serving different patient complexities. The hospital’s demographics, inpatient diagnosis, pharmacy, and laboratory databases were accessed. They contained information on encrypted patient ID; age; sex; health insurance cover; date of birth; diagnosis (using the International Classification of Diseases, Tenth Revision); admission date; procedure code; exogenous albumin dispensation date, code; and laboratory name, code, date, and findings. The pre-surgical period was used to determine the albumin level and other covariates. In contrast, the post-surgical period was used to determine post-operative in-hospital death and LOS, which were outcomes of interest (Fig. 1).
Fig. 1.
Data collection timeline. GI gastrointestinal
Patient Inclusion
Patients were eligible if they were admitted to the hospital for GI surgery between October 2014 and March 2021. Gastric tract, esophagus, duodenum, and colon resections were selected as index surgeries based on clinical consultations with clinical experts. Patients with incomplete albumin level tests in the pre-surgical period were excluded.
Exposure and Outcomes
The included patients were classified into three groups. First is patients with severe hypoalbuminemia, defined as a pre-operative serum albumin level of < 2.0 g/dL. Second is patients with non-severe hypoalbuminemia (pre-operative serum albumin level of 2.0–3.4 g/dL). The last is patients with a normal albumin level (3.5–5.5 g/dL).The cut-off point was selected based on a recommendation by Liumbruno et al. [12] for starting exogenous albumin for patients with hypoalbuminemia undergoing major surgeries. The cut-off was selected by our Pharmaceutical and Therapeutic Committee. However, some guidelines recommended using an albumin level < 2.5 g/dL for starting exogenous albumin for patients with hypoalbuminemia. Thus, we performed a sensitivity analysis by applying the cut-off as < 2.5 g/dL for severe hypoalbuminemia to explore the differences of outcomes among different cut-offs (< 2.0 vs < 2.5 g/dL). The primary outcome of interest was in-hospital death, defined by discharge status. The secondary outcome was LOS.
Statistical Analysis
Descriptive statistics were used to present patient characteristics. As appropriate, independent t tests, Mann–Whitney U tests, chi-square tests, and Fisher’s exact tests were used to compare the patient characteristics of the groups. For a confounder adjustment, multivariable logistic regression with a propensity score adjustment was used to associate the serum albumin level with post-operative in-hospital death. In contrast, a multivariable generalized linear model with log-link and Poisson distribution was employed for LOS. The covariates for propensity score estimation were age, sex, and history of comorbidities (chronic liver disease, renal disease, malignancy, chronic heart failure, ischemic heart disease, hemorrhagic stroke, thyroid disease, diabetes, and hypertension), and procedures. The use of exogenous albumin was treated as a confounder in the final models along with the propensity score. The average marginal effects for LOS were estimated to simplify interpretation.
Two additional analyses were performed. First, we compared the outcomes for severe hypoalbuminemia versus non-severe hypoalbuminemia using two different cut-offs. Second, we compared the outcomes for patients who had a pre-operative serum albumin level of < 2.0 g/dL and 2.0 to < 2.5 g/dL. Probability (p) values less than 0.05 were considered statistically significant. Analyses were performed using STATA, version 15.0 (StataCorp, College Station, TX, USA).
Results
Patient Characteristics
A total of 1973 patients underwent the selected GI surgeries during the study period. Patients without an albumin level at baseline were excluded (Fig. 2), leaving 670 patients who met our inclusion criteria. Their average age was 57.4 ± 16.3 years, and 56.1% were men. Of those, 59 patients (8.8%) had severe hypoalbuminemia (< 2.0 g/dL), 302 patients (45.1%) had non-severe hypoalbuminemia (2.0–3.4 g/dL), and 309 patients (46.1%) had a normal albumin level. Most baseline characteristics were not statistically significant different except procedures including duodenectomy, colectomy, and anastomosis. Forty-two patients with severe hypoalbuminemia (71.2%) received exogenous albumin, 109 patients with non-severe hypoalbuminemia (36.1%) received exogenous albumin, and 27 patients (8.7%) with a normal albumin level received exogenous albumin. All patient characteristics are detailed in Table 1.
Fig. 2.
Flow of patient selection
Table 1.
Characteristics of patients undergoing selected gastrointestinal surgeries
| Characteristics | Severe hypoalbuminemia (< 2.0 g/dL) n (%) (n = 59) |
Non-severe hypoalbuminemia (2.0–3.4 g/dL) n (%) (n = 302) |
Normal albumin level (> 3.4–5.5 g/dL) n (%) (n = 309) |
Total n (%) (N = 670) |
p value |
|---|---|---|---|---|---|
| Age ( years, mean ± SD) | 61.5 ± 18.5 | 56.9 ± 18.0 | 57.1 ± 13.9 | 57.4 ± 16.3 | 0.063 |
| < 18 | 2 (3.4) | 9 (3.0) | 3 (1.0) | 14 (2.1) | 0.079 |
| 18–60 | 21 (35.6) | 154 (51.0) | 158 (51.1) | 333 (49.7) | |
| ≥ 60 | 36 (61.0) | 139 (46.0) | 148 (74.9) | 323 (48.2) | |
| Sex | |||||
| Male | 38 (64.4) | 176 (58.3) | 162 (52.4) | 376 (56.1) | 0.140 |
| Female | 21 (35.6) | 126 (41.7) | 147 (47.6) | 294 (43.9) | |
| Health insurance | |||||
| UCS | 45 (76.3) | 211 (69.9) | 185 (59.9) | 441 (65.8) | 0.080 |
| SSS | 7 (11.8) | 43 (14.2) | 54 (20.7) | 114 (17.0) | |
| CSMBS | 4 (6.8) | 22 (7.3) | 33 (10.7) | 59 (8.8) | |
| Other | 3 (5.1) | 26 (9.6) | 27 (8.7) | 56 (8.4) | |
| Comorbidities | |||||
| Chronic liver disease | 2 (3.4) | 15 (5.0) | 5 (1.6) | 22 (3.3) | 0.052 |
| Renal disease | 2 (3.4) | 3 (1.0) | 1 (0.3) | 6 (0.9) | 0.078 |
| Malignancy | 23 (39.0) | 146 (48.3) | 140 (45.3) | 309 (46.1) | 0.388 |
| Chronic heart failure | 1 (1.7) | 7 (2.3) | 1 (0.3) | 9 (1.3) | 0.085 |
| Ischemic heart disease | 1 (1.7) | 7 (2.3) | 5 (1.6) | 13 (1.9) | 0.813 |
| Hemorrhagic stroke | 1 (1.7) | 2 (0.7) | 1 (0.3) | 4 (0.6) | 0.293 |
| Thyroid disease | 2 (3.4) | 5 (1.7) | 3 (1.0) | 10 (1.5) | 0.244 |
| Diabetes | 8 (13.6) | 46 (15.2) | 35 (11.3) | 89 (13.3) | 0.363 |
| Hypertension | 10 (17.0) | 66 (21.9) | 77 (24.9) | 153 (22.8) | 0.352 |
| Procedure | |||||
| Gastrectomy | 3 ( 5.1) | 13 (4.3) | 11 (3.6) | 27 (4.0) | 0.817 |
| Duodenectomy | 22 (37.3) | 101 (33.4) | 41 (13.3) | 164 (24.5) | <0.001 |
| Colectomy | 33 (55.9) | 168 (55.6) | 219 (70.9) | 420 (62.7) | <0.001 |
| Intestinectomy | 0 (0.0) | 0 (0.0) | 1 (0.3) | 1 (0.15) | 1.000 |
| Anastomosis | 32 ( 54.3) | 180 (59.6) | 140 (45.3) | 352 (52.5) | 0.002 |
CSMBS Civil Servant Medical Benefit Scheme, SD standard deviation, SSS Social Security Scheme, UCS Universal Coverage Scheme
Outcome for Severe Hypoalbuminemia Cut-Off as < 2.0 g/dL
Post-operative In-Hospital Death
The post-operative in-hospital death rate for all patients was 13.9% (93 deaths from 670 patients). The post-operative in-hospital death for patients with severe hypoalbuminemia was 40.7% (24/59 patients). The death rate for patients with non-severe hypoalbuminemia was 19.5% (59/302 patients), while that for patients with a normal albumin level was 3.2% (10/309 patients). The adjusted odds ratio (OR) for post-operative in-hospital death comparing patients with severe hypoalbuminemia to those with a normal albumin level was 8.11 (3.31–19.87; p < 0.001). The adjusted OR for post-operative in-hospital death comparing patients with non-severe hypoalbuminemia to those with a normal albumin level was 3.89 (1.87–8.10; p < 0.001) [Table 2].
Table 2.
Effects of the pre-operative albumin level on post-operative in-hospital death and length of stay in hospital according to serum albumin levels (cut-off of < 2.5 g/dL for severe hypoalbuminemia) at admission
| Number of events (%) | Unadjusted effect sizea (95% CI; p value) | Adjusted effect sizea (95% CI; p value) | |
|---|---|---|---|
| Post operative in-hospital death (N = 670) | |||
| Baseline albumin level | |||
| Normal albumin | 10 (3.2) | Reference | Reference |
| Non-severe hypoalbuminemia | 59 (19.5) | 7.26 (3.64–14.49; p < 0.001) | 3.89 (1.87–8.10; p < 0.001) |
| Severe hypoalbuminemia | 24 (40.7) | 20.50 (9.06–46.39; p < 0.001) | 8.11 (3.31–19.87; p < 0.001) |
| Length of stay [median (IQR)] (days) (N = 670) | |||
| Baseline albumin level | |||
| Normal albumin | 11 (2–16) | Reference | Reference |
| Non-severe hypoalbuminemia | 18 (12–28) | 10.01 (9.35–10.67; p < 0.001) | 6.42 (5.69–7.16; p < 0.001) |
| Severe hypoalbuminemia | 22 (13–35) | 16.57 (15.14–17.99; p < 0.001) | 8.66 (7.35–9.96; p < 0.001) |
Note: all multivariable regression models were adjusted by exogenous albumin use and propensity score, which were predicted by all the baseline observed covariates
CI confidence interval, IQR interquartile range
aOdds ratio for post-operative in-hospital death and mean difference for length of stay
LOS
The median LOS for all patients was 14 (interquartile range 8–23). The median LOS for patients with severe hypoalbuminemia was 22 days (interquartile range 13–35). The median LOS for patients with non-severe hypoalbuminemia and a normal albumin level were 18 (12–28) and 11 (2–16) days, respectively. The adjusted mean differences were 8.66 (7.35–9.96; p < 0.001) and 6.42 (5.69–7.16; p < 0.001) days for severe and non-severe hypoalbuminemia, respectively (Table 2).
Outcome for Severe Hypoalbuminemia Cut-Off as < 2.5 g/dL
Post-operative In-Hospital Death
The post-operative in-hospital death for patients with severe hypoalbuminemia (cut-off as < 2.5 g/dL) was 57.0% (53/148 patients). The death rate for patients with non-severe hypoalbuminemia was 32.3% (30/213 patients), while that for patients with a normal albumin level was 3.2% (10/309 patients). The adjusted OR for post-operative in-hospital death comparing patients with severe hypoalbuminemia to those with a normal albumin level was 7.44 (3.38–16.36; p < 0.001). The adjusted OR for post-operative in-hospital death comparing patients with non-severe hypoalbuminemia to those with a normal albumin level was 3.02 (1.40–6.52; p = 0.005) [Table 3].
Table 3.
Effects of the pre-operative albumin level on post-operative in-hospital death, length of stay according to serum albumin levels (cut-off as < 2.5 g/dL for severe hypoalbuminemia) at admission
| Number of events (%) | Unadjusted effect sizea (95% CI; p value) | Adjusted effect sizea (95% CI; p value) | |
|---|---|---|---|
| Post operative in-hospital death (N = 670) | |||
| Baseline albumin level | |||
| Normal albumin (N = 309) | 10 (3.2) | Reference | Reference |
| Non-severe hypoalbuminemia (N = 213) | 30 (32.3) | 4.90 (2.34–10.26; p < 0.001) | 3.02 (1.40–6.52; p = 0.005) |
| Severe hypoalbuminemia (N =148) | 53 (57.0) | 16.68 (8.17–34.07; p < 0.001) | 7.44 (3.38–16.36; p < 0.001) |
| Length of stay [median (IQR)] (days) (N = 670) | |||
| Baseline albumin level | |||
| Normal albumin (N = 309 | 11 (2–16) | Reference | Reference |
| Non-severe hypoalbuminemia (N = 213) | 18 (12–26) | 9.39 (8.65–10.12; p < 0.001) | 6.67 (5.88–7.46; p < 0.001) |
| Severe hypoalbuminemia (N =148) | 20 (13–33.5) | 13.53 (12.62–14.44; p < 0.001) | 6.75 (5.80–7.70; p < 0.001) |
Note: all multivariable regression models were adjusted by exogenous albumin use and propensity score, which were predicted by all the baseline observed covariates
CI confidence interval, IQR interquartile range
aOdds ratio for post-operative in-hospital death and mean difference for length of stay
LOS
The median LOS for patients with severe hypoalbuminemia (cut-off as < 2.5 g/dL) was 20 days (interquartile range 13–33.5). The median LOS for patients with non-severe hypoalbuminemia and a normal albumin level were 18 (12–26) and 11 (2–16) days, respectively. The adjusted mean differences were 6.75 (5.80–7.70; p < 0.001) and 6.67 (5.88–7.46; p < 0.001) days for severe and non-severe hypoalbuminemia, respectively (Table 3).
Additional Analyses
Comparing Between Severe Hypoalbuminemia Versus Non-severe Hypoalbuminemia
At the cut-offs of < 2.0 g/dL for severe hypoalbuminemia, the adjusted OR for post-operative in-hospital death for severe hypoalbuminemia was 2.07 (1.09–3.93; p = 0.025) compared to non-severe hypoalbuminemia. The adjusted mean difference for LOS for severe hypoalbuminemia compared to non-severe hypoalbuminemia was 4.48 (3.14–5.81; p < 0.001) days (Table A1 of the Electronic Supplementary Material [ESM]).
At the cut-off of < 2.5 g/dL for severe hypoalbuminemia, the adjusted OR for post-operative in-hospital death for severe hypoalbuminemia was 2.54 (1.45–4.43; p = 0.001) compared to non-severe hypoalbuminemia. The adjusted mean difference for LOS for severe hypoalbuminemia compared to non-severe hypoalbuminemia was 1.71 (0.61–2.81; p = 0.002) [Table A1 of the ESM].
Comparing Between Patients Who Had Pre-Operative Serum Albumin Levels of < 2.0 g/dL and 2.0 to < 2.5 g/dL
A total of 163 patients were included in this additional analysis. One hundred and four patients (63.8%) had a pre-operative serum albumin level between 2.0 and < 2.5 g/dL, while 59 patients (36.2%) had a pre-operative serum albumin level < 2.0 g/dL. The in-hospital death rate for patients with an albumin level < 2.0 g/dL was 40.7% (24/59 patients), while that for patients with an albumin level of 2.0 to < 2.5 g/dL was 33.6% (35/104 patients). The adjusted OR for post-operative in-hospital death was 1.25 (0.62–2.51; p = 0.530). The adjusted mean difference for LOS was 4.24 (2.55–5.93; p < 0.001) [Table A2 of the ESM].
Discussion
Our study found an association between pre-operative serum albumin levels and the post-operative in-hospital death and LOS of patients undergoing GI surgery. Patients with severe hypoalbuminemia had an approximately 7.4- to 8.1-fold higher risk of post-operative in-hospital death and 6–8 days longer hospital stays than patients with a normal serum albumin level at a pre-operative assessment. In addition, patients with non-severe hypoalbuminemia also had a higher risk of post-operative in-hospital death and longer hospital stays than patients with a normal serum albumin level. Patients with severe hypoalbuminemia had a significantly higher risk of post-operative in-hospital death and longer LOS than patients with non-severe hypoalbuminemia. However, the risk of death for patients with severe hypoalbuminemia was not statistically significant different between patients with a serum albumin level < 2.0 g/dL and 2.0 to < 2.5 g/dL at a pre-operative assessment.
Hypoalbuminemia is prevalent among admitted and critically ill patients. Critical illness is associated with hypoalbuminemia through a variety of mechanisms. It could alter the distribution of albumin between the intravascular and extravascular compartments resulting in the reduction in albumin synthesis and the increase in albumin degradation and clearance. The reduction in albumin synthesis is a result of the increase in gene transcription for the positive acute-phase proteins (such as C-reactive protein) and a decrease in the albumin messenger RNA transcription rate. However, the increase in albumin degradation and clearance is because of the increased capillary leakage, which is affected by some cytokines in the inflammation process such as tumor necrosis factor-alpha, interleukin-6, prostaglandins, and complement components [22].
Our observed overall post-operative in-hospital death rate was 13.9%. It was consistent with the previous rate reported by another study from a high-income country [18]. The study reported the 30-day mortality rate for patients with colorectal surgeries that ranged from 2.0% in patients with an albumin level of > 4.0 g/dL to 26.9% in patients with an albumin level < 2.5 g/dL. Our observed in-hospital death rate was also consistent with the finding from a previous study in Thailand [23]. The study was conducted in four hospitals for patients undergoing high-risk surgeries. They found that the in-hospital death rate was approximately 10.0%. Specifically, the in-hospital death rate for high-risk GI surgeries was 8.3%.
Our findings align with other investigations that found that patients with hypoalbuminemia are associated with higher in-hospital mortality rates across diseases [24–27]. We also found that patients with severe hypoalbuminemia, cut-offs of either < 2.0 or < 2.5 g/dL, had a significant higher risk of post-operative in-hospital death than both patients with a normal serum albumin level and non-severe hypoalbuminemia. We also found the dose–response relationship between the serum albumin level and the risk of in-hospital death. Patients with non-severe hypoalbuminemia had approximately a three to four times higher risk of in-hospital death than patients with a normal serum albumin level. In addition, patients with severe hypoalbuminemia had an approximately 2.0–2.5 higher risk of in-hospital death than patients with non-severe hypoalbuminemia. We observed that the serum albumin level at a pre-operative assessment is a strong predictor of the risk of in-hospital death. Patients with a lower serum albumin level had a higher risk of death.
We also explored the effects of different cut-offs for severe hypoalbuminemia as < 2.0 and <2.5 g/dL because of the different guidelines recommending different pre-operative serum albumin levels for starting an exogenous albumin injection. We found that the effect sizes of comparing between severe hypoalbuminemia and a normal albumin level for both cut-offs were relative similar. The ORs for post-operative in-hospital death for the cut-offs were not largely different (8.11 for cut-off as < 2.0 g/dL and 7.44 for cut-off as < 2.5 g/dL). In addition, we determined the risk of in-hospital death among patients with a pre-operative serum albumin level < 2.0 g/dL and 2.0 to < 2.5 g/dL to explore whether the risk of death among the patients was different. We found no significant difference among the groups. It indicated that the use of different cut-offs for assess the severity of hypoalbuminemia might not affect the clinical outcome.
The limitations of this study should be discussed. First, because of the nature of retrospective database research, confounding by indication usually exists. We tried to reduce this problem by employing a propensity score adjustment. This approach is a well-known method of reducing confounding bias in retrospective database analyses. Second, there were some missing data in the reviewed databases, particularly laboratory data. We excluded patients with missing data from the analysis. Third, because of the nature of our database, we could not determine the causes of hypoalbuminemia. Fourth, we did not assess the effect of exogenous albumin injection use, which might affect the association of different serum albumin levels and the risk of in-hospital death. It was because we did not know who, how, and why some patients received an exogenous albumin injection but some did not. Estimating the effect of exogenous albumin injection use on the risk of in-hospital death might mislead the readers because of a lack of such information. However, we attempted to minimize the confounding effect of exogenous albumin injection use by adding it as a confounder along with the propensity score in the final regression model. Finally, our research was carried out at a tertiary hospital in Thailand. Consequently, the generalizability of our findings is limited to healthcare settings where the health system and characteristics of the patients are similar to our setting. Extrapolation must be approached with prudence.
This study provided valuable information on the importance of the pre-operative assessment of serum albumin levels for patients who are about to undergo GI surgery. The findings are particularly beneficial for surgeons in low- and middle-income countries.
Conclusions
Severe pre-operative hypoalbuminemia in patients undergoing GI surgery was associated with an increased risk of in-hospital mortality and prolonged LOS. The risk of death for patients with severe hypoalbuminemia was relatively similar when using different cut-offs of < 2.0 and <2.5 g/dL. Our information will be useful for clinicians and policymakers to consider strategies to improve healthcare for patients with GI surgeries.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
This study was partially supported by a grant from the University of Phayao via the Unit of Excellence on Clinical Outcomes Research and Integration (UNICORN; Grant number: FF66-UoE004). The funding source did not involve the study design, data collection, data analysis, data interpretation, or manuscript writing.
Conflict of interest
All authors declare no conflicts of interest related to this study.
Ethics approval
This study was approved by the hospital’s ethics committee (RYHREC No. E026/2564).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and analyzed during the current study are not publicly available because of the confidentiality of data but are available from the corresponding author upon a reasonable request.
Code availability
The codes generated and analyzed during the current study are not publicly available but are available from the corresponding author upon a reasonable request.
Author contributions
Study conception and design: PP-i, SS, PD, PP. Acquisition of data: PP-i, SS, PD. Analysis of data: PP-i, SS, PD. Interpretation of data: PP-i, SS, PP, PD. Drafting of the manuscript: PP-i, SS, PP, PD. Critical revision of the manuscript: PP-i, SS, PP, PD.
Contributor Information
Pochamana Phisalprapa, Email: coco_a105@hotmail.com, Email: a.pochamana@gmail.com.
Piyameth Dilokthornsakul, Email: piyamethd@gmail.com, Email: piyameth.dilok@cmu.ac.th.
References
- 1.Limaye K, Yang JD, Hinduja A. Role of admission serum albumin levels in patients with intracerebral hemorrhage. Acta Neurol Belg. 2016;116(1):27–30. doi: 10.1007/s13760-015-0504-2. [DOI] [PubMed] [Google Scholar]
- 2.Rich MW, Keller AJ, Schechtman KB, Marshall WG, Jr, Kouchoukos NT. Increased complications and prolonged hospital stay in elderly cardiac surgical patients with low serum albumin. Am J Cardiol. 1989;63(11):714–718. doi: 10.1016/0002-9149(89)90257-9. [DOI] [PubMed] [Google Scholar]
- 3.Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160–167. doi: 10.1016/0002-9610(80)90246-9. [DOI] [PubMed] [Google Scholar]
- 4.Detsky AS, Baker JP, O'Rourke K, Johnston N, Whitwell J, Mendelson RA, et al. Predicting nutrition-associated complications for patients undergoing gastrointestinal surgery. JPEN J Parenter Enteral Nutr. 1987;11(5):440–446. doi: 10.1177/0148607187011005440. [DOI] [PubMed] [Google Scholar]
- 5.Goiburu ME, Goiburu MM, Bianco H, Diaz JR, Alderete F, Palacios MC, et al. The impact of malnutrition on morbidity, mortality and length of hospital stay in trauma patients. Nutr Hosp. 2006;21(5):604–610. [PubMed] [Google Scholar]
- 6.Norberg A, Rooyackers O, Segersvard R, Wernerman J. Leakage of albumin in major abdominal surgery. Crit Care. 2016;20(1):113. doi: 10.1186/s13054-016-1283-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norberg A, Rooyackers O, Segersvard R, Wernerman J. Albumin kinetics in patients undergoing major abdominal surgery. PLoS ONE. 2015;10(8):e0136371. doi: 10.1371/journal.pone.0136371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Issangya CE, Msuya D, Chilonga K, Herman A, Shao E, Shirima F, et al. Perioperative serum albumin as a predictor of adverse outcomes in abdominal surgery: prospective cohort hospital based study in Northern Tanzania. BMC Surg. 2020;20(1):155. doi: 10.1186/s12893-020-00820-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Truong A, Hanna MH, Moghadamyeghaneh Z, Stamos MJ. Implications of preoperative hypoalbuminemia in colorectal surgery. World J Gastrointest Surg. 2016;8(5):353–362. doi: 10.4240/wjgs.v8.i5.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kudsk KA, Tolley EA, DeWitt RC, Janu PG, Blackwell AP, Yeary S, et al. Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J Parenter Enteral Nutr. 2003;27(1):1–9. doi: 10.1177/014860710302700101. [DOI] [PubMed] [Google Scholar]
- 11.Statkevicius S, Bonnevier J, Fisher J, Bark BP, Larsson E, Oberg CM, et al. Albumin infusion rate and plasma volume expansion: a randomized clinical trial in postoperative patients after major surgery. Crit Care. 2019;23(1):191. doi: 10.1186/s13054-019-2477-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G. Recommendations for the transfusion of red blood cells. Blood Transfus. 2009;7(1):49–64. doi: 10.2450/2008.0020-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farsad BF, Hadavand N, Masumii S, Salehi H. Albumin utilization review to evaluate the efficacy and cost, perform as a qualitative study in special wards in Shaheed Rajaei Cardiovascular, Medical & Research Center. Biosci Biotech Res Asia. 2016;13(3):1469–1477. doi: 10.13005/bbra/2290. [DOI] [Google Scholar]
- 14.Jahangard-Rafsanjani Z, Javadi MR, Torkamandi H, Alahyari S, Hajhossein Talasaz A, Gholami K. The evaluation of albumin utilization in a teaching university hospital in Iran. Iran J Pharm Res. 2011;10(2):385–390. [PMC free article] [PubMed] [Google Scholar]
- 15.Kazemi Y, Hadavand N, Hayatshahi A, Torkamandi H, Gholami K, Hadjibabaie M, et al. Albumin utilization in a teaching hospital in Tehran: time to revise the prescribing strategies. J Pharm Care. 2013;1(4):127–132. [Google Scholar]
- 16.Talasaz AH, Jahangard-Rafsanjani Z, Ziaie S, Fahimi F. Evaluation of the pattern of human albumin utilization at a university affiliated hospital. Arch Iran Med. 2012;15(2):85–87. [PubMed] [Google Scholar]
- 17.Nafisi S, Akhavan S, Shiva A, Ghasempour M, Dariush P, Makhdoomi KH, et al. Evaluation of human albumin use pattern in a referral teaching hospital. J Pharm Care. 2019;7(3):41–48. [Google Scholar]
- 18.Montomoli J, Erichsen R, Antonsen S, Nilsson T, Sorensen HT. Impact of preoperative serum albumin on 30-day mortality following surgery for colorectal cancer: a population-based cohort study. BMJ Open Gastroenterol. 2015;2(1):e000047. doi: 10.1136/bmjgast-2015-000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Javan-Noughabi J, Parnian E, Hajiesmaeili M, Salehiniya H, Setoodehzadeh F. The impact of a guideline to prevent inappropriate albumin administration in a hospital in Iran. Br J Healthcare Manag. 2020;26(10):1–7.
- 20.Akirov A, Masri-Iraqi H, Atamna A, Shimon I. Low albumin levels are associated with mortality risk in hospitalized patients. Am J Med. 2017;130(12):1465.e11–9. doi: 10.1016/j.amjmed.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Jellinge ME, Henriksen DP, Hallas P, Brabrand M. Hypoalbuminemia is a strong predictor of 30-day all-cause mortality in acutely admitted medical patients: a prospective, observational, cohort study. PLoS ONE. 2014;9(8):e105983. doi: 10.1371/journal.pone.0105983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gounden V, Vashisht R, Jialal I. Hypoalbuminemia. Treasure Island: StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 23.Kongpakwattana K, Dilokthornsakul P, Dhippayom T, Chaiyakunapruk N. Clinical and economic burden of postsurgical complications of high-risk surgeries: a cohort study in Thailand. J Med Econ. 2020;23(10):1046–1052. doi: 10.1080/13696998.2020.1787420. [DOI] [PubMed] [Google Scholar]
- 24.Plakht Y, Gilutz H, Shiyovich A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction II (SAMI-II) project. Int J Cardiol. 2016;219:20–24. doi: 10.1016/j.ijcard.2016.05.067. [DOI] [PubMed] [Google Scholar]
- 25.Arques S, Roux E, Sbragia P, Gelisse R, Pieri B, Ambrosi P. Usefulness of serum albumin concentration for in-hospital risk stratification in frail, elderly patients with acute heart failure. Insights from a prospective, monocenter study. Int J Cardiol. 2008;125(2):265–267. doi: 10.1016/j.ijcard.2007.07.094. [DOI] [PubMed] [Google Scholar]
- 26.Cho YM, Choi IS, Bian RX, Kim JH, Han JY, Lee SG. Serum albumin at admission for prediction of functional outcome in ischaemic stroke patients. Neurol Sci. 2008;29(6):445–449. doi: 10.1007/s10072-008-1024-0. [DOI] [PubMed] [Google Scholar]
- 27.Boonpipattanapong T, Chewatanakornkul S. Preoperative carcinoembryonic antigen and albumin in predicting survival in patients with colon and rectal carcinomas. J Clin Gastroenterol. 2006;40(7):592–595. doi: 10.1097/00004836-200608000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.