Abstract
Purpose:
The purpose of the study was to increase the proportion of youth living with HIV (YLWH) aged ≥11 years who undergo developmentally appropriate disclosure about their HIV status.
Methods:
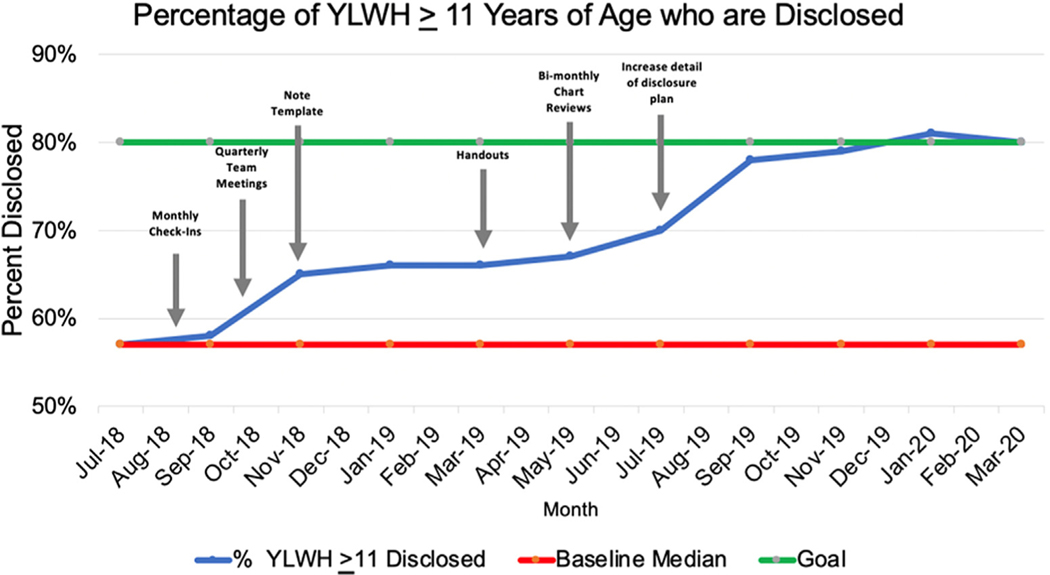
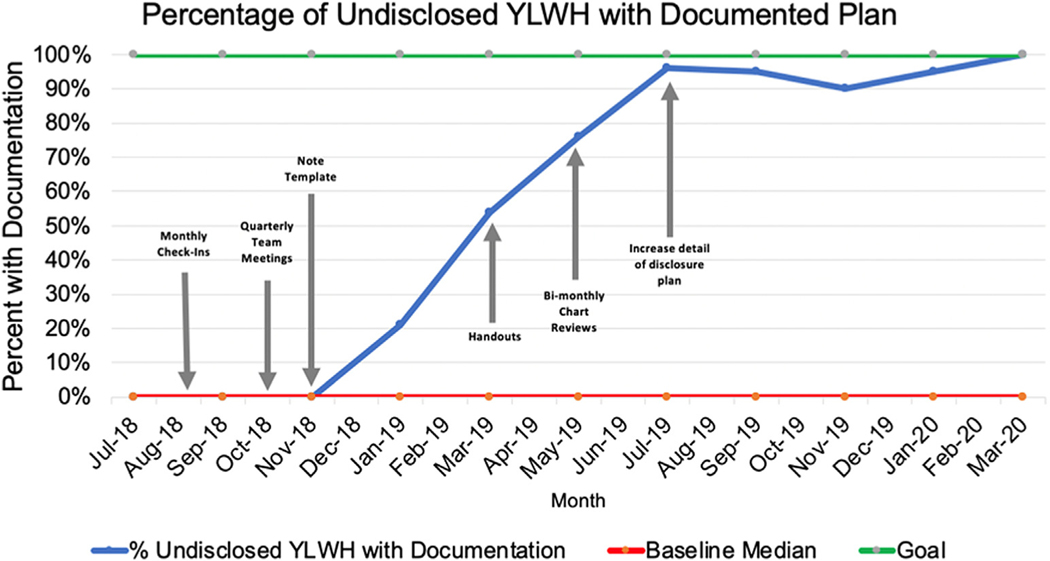
A quality improvement project was initiated at an urban pediatric HIV clinic between July 2018 and March 2020. The primary outcome measure was the proportion of YLWH aged ≥11 years who were disclosed to about their HIV status. The proportion of undisclosed YLWH who had documented nondisclosure status was also assessed as a process measure. Plan-Do-Study-Act (PDSA) cycles for change included monthly clinic staff check-ins to discuss new disclosures, quarterly team meetings to discuss strategies to improve disclosure, and modifying a clinic note template to prompt providers to document disclosure status. Annotated run charts were used to analyze the data.
Results:
Before the first PDSA cycle, 26/46 (57%) of the target population of YLWH aged ≥11 years had their HIV status disclosed to them, and none of the undisclosed youth had disclosure status documented in their medical record. After 20 months and six PDSA cycles, the proportion of YLWH aged ≥11 years disclosed to about their HIV status increased to 80% and the proportion of undisclosed YLWH with documentation of their disclosure status increased to 100%.
Conclusions:
Several interventions integrated throughout the pediatric HIV care process were associated with an increase in the proportion of YLWH with developmentally appropriate HIV disclosure and documentation of disclosure status, an important psychosocial aspect of care in these individuals.
Keywords: HIV, Quality improvement, Disclosure, Adolescent health
Since the onset of the HIV pandemic, the incidence of perinatally acquired HIV infection has drastically decreased with the implementation of antiretroviral therapy and prevention of mother-to-child transmission services [1]. However, clinicians should be knowledgeable about the management approach to youth living with HIV (YLWH) as new cases occur every year, even in well-resourced countries such as the U.S. In 2018, 91 youths younger than 13 years were diagnosed with HIV in the U.S., and 66 of them had confirmed perinatally acquired infection [2]. In addition, internationally born youth with perinatally acquired HIV (IB-YPHIV) represent a steadily growing majority of pediatric and adolescent HIV cases in the U.S., now accounting for 70% of YLWH younger than 13 years [3]. Developmentally appropriate disclosure of HIV status to YLWH, among many other medical and psychosocial issues that providers need to address, increases the likelihood of optimal health outcomes for these young adolescents [4].
The American Academy of Pediatrics and World Health Organization recommend that YLWH have their HIV status disclosed to them by school age [5,6]. Several studies have suggested that YLWH who know their HIV status have higher self-esteem than those who do not know, and parents of disclosed YLWH experience less depression than parents of undisclosed YLWH [7–9]. If disclosure is carried out incrementally over time and with sensitivity to young adolescents’ developmental status and capacity for understanding, it may be associated with better psychological and emotional well-being [5,10–13]. Furthermore, a study from Namibia demonstrated that YLWH who were disclosed to early and appropriately were more adherent to their treatment as they became young adults and gained independence in their health care [14]; and in turn, they had a reduced risk of death [5,14]. On the other hand, inadvertent and/or abrupt disclosure may adversely affect the well-being and health outcomes of YLWH [5].
Despite the importance of timely disclosure, prior studies performed in various high-resource countries, such as the U.S. and European countries, have demonstrated that the proportion of YLWH who are disclosed to about their status ranges from 10% to 75% across these settings [10]. Decisions regarding disclosure of HIV status to YLWH are complex as health-care providers must consider stigma associated with HIV, the availability of social support, individual cultural norms, the dynamic of family relations, parental skills, and young adolescents’ emotional and maturational ability to maintain privacy and understand and cope with having a chronic disease. In addition, YPHIV who are disclosed of their status may also inadvertently learn their mother’s HIV status, further complicating the disclosure process [5,15,16].
Owing to these factors, clinic visit time constraints, and other high-priority concerns during routine HIV clinic encounters, the disclosure process may often be delayed. For example, clinicians might focus on improving medication adherence rather than facilitating developmentally appropriate disclosure; however, effort toward disclosure might ultimately promote improved medication adherence while also contributing to other important outcomes.
Before the start of this quality improvement initiative, only 57% of YLWH aged ≥11 years at an urban pediatric HIV clinic in the Southeastern U.S. were disclosed to about their HIV status. In addition, none of the undisclosed patients had documentation of their undisclosed status or a plan for future disclosure in their electronic medical record (EMR). The aim of this quality improvement project was to prioritize optimal disclosure of YLWH and increase the proportion of YLWH aged ≥11 years who are disclosed to about their status to ≥80% within 2 years.
Methods
The Institute for Healthcare Improvement’s model for improvement was used for this project. This model is a simple and frequently used tool for accelerating improvement in various health-care settings. The model involves first establishing the aim of the project and the measure of improvement and then determining which changes can be made to result in improvement [17]. These changes are then tested by Plan-Do-Study-Act (PDSA) cycles, which involve (1) planning the intervention and method for data collection; (2) performing the intervention; (3) analyzing the data after intervention; and (4) refining the intervention based on the results [18]. This project was approved by the Vanderbilt University Institutional Review Board (IRB# 200681). The institutional review board did not require that informed consent be obtained as all data were collected as part of routine care and in aggregate without personal identifiers.
Study population
Our initiative took place from July 1, 2018 to March 10, 2020. The target population included YLWH aged 3–25 years who were followed up at an urban pediatric HIV clinic in the Southeastern U.S. To promote independence in their health care, disclosed adolescents were transitioned to an adolescent HIV clinic on an ongoing basis. Transition to adolescent or adult HIV care was sometimes delayed in older YLWH despite being disclosed to about their status until they were emotionally ready to transition to a new provider. Once patients were transitioned to the adolescent clinic, they were no longer a part of our patient list from which we abstracted data and therefore were excluded from our ongoing assessments. The denominators for proportion calculations were updated accordingly during each segment of analysis.
Setting/context
The pediatric HIV clinic, which cared for 69 YLWH at the start of this project and was situated in an urban university-affiliated medical center, evaluated and treated patients during the dedicated HIV clinic one half-day each week. Patients resided in urban, suburban, and rural areas within the region, and some had as long as a 2-hour commute to the clinic. The HIV clinic team consisted of two rotating pediatric infectious disease attending physicians, a rotating pediatric infectious disease fellow, and an occasional rotating pediatric resident, medical student, and/or pharmacy resident. A pediatric nurse who knew all of the YLWH well was present for all of the clinic sessions and kept the providers up-to-date on the patient’s disclosure status. Occasionally, a social worker, who also knew the YLWH well, would join the clinic. Although many trainees rotated through the clinic, one of two different pediatric infectious disease attending physicians supervised every patient encounter. The attending physician and/or fellow were responsible for addressing the disclosure status of the patient with the caregiver and for documentation of the clinic visit in the EMR. The nurse regularly notified the providers of the adolescent HIV clinic about YLWH who would be eligible for transition to adolescent care.
Before our initiative, the process of disclosure was unique to each patient, with no standardized process for disclosing HIV status to young adolescents. In general, when the patient was school aged, their understanding of basic concepts of health and disease was assessed. Then, over the course of several visits and in age-appropriate language, they were taught about the immune system, host-virus interactions, the role of medication, and the importance of medication adherence. Eventually, the virus was called out by name, HIV, and modes of HIV transmission and risk behaviors were discussed within the broader context of adolescent and sexual health. The content and order of these conversations were further guided by patient and caregiver questions, and families were encouraged to continue these conversations at home between clinic visits. They were considered fully disclosed when they knew they had a virus called HIV.
Measures
The primary outcome measure was the proportion of YLWH aged ≥11 years who were disclosed to about their HIV status. The proportion of undisclosed YLWH of all ages with documentation in their chart about their disclosure status was assessed as a process measure. Documented status was defined as a simple declaration of whether or not the patient was disclosed to about their status in the last HIV clinic visit note filed in the EMR. Both the primary outcome and process measures were abstracted from medical records every 2 months, and aggregate data were used to construct run charts (graphs of the outcome and process measures plotted over time) that were assessed on an ongoing basis [17].
Interventions
Based on the results of initial and ongoing data collection, several interventions were developed for iterative PDSA cycles. The run charts described previously were annotated with these interventions to improve assessment of the relative impact of each intervention/PDSA cycle.
Since July 2018, six interventions/PDSA cycles were iteratively implemented:
August 2018: The first intervention to kick off the project involved checking in with the clinic nurse, who was present at all HIV clinic sessions, to discuss new patient disclosures each month. This also prompted the nurse to encourage the physicians to begin the disclosure process for undisclosed YLWH.
October 2018: Quarterly meetings were organized by the project leader to allow for physician input regarding subsequent interventions to improve the disclosure process. During these meetings, run charts would be presented to the whole clinic team. These run charts motivated the providers to implement new interventions and to prioritize disclosure to reach our goal of optimizing the proportion of YLWH aged ≥11 years who were disclosed.
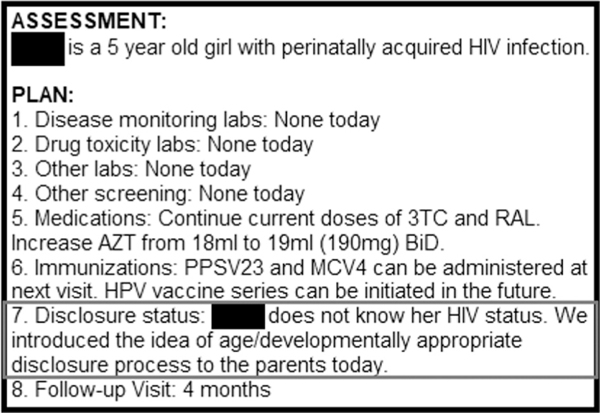
November 2018: Our team created and implemented a new pediatric HIV outpatient clinic visit note template. This template included a section to document disclosure status in the plan portion of the note to remind providers to address and/or document the patients’ disclosure status (Figure 1). A major challenge to implementing this intervention was the extra time required to remember and create new notes for patients rather than copying forward prior clinic notes. To overcome this challenge, the project leader notified clinicians about patients who were not transitioned to the new note template during quarterly meetings.
March 2019: To help initiate the process of disclosure for undisclosed patients, we reviewed published handouts intended for caregivers of YLWH and compiled them in the pediatric HIV clinic to be available for physicians to share with caregivers [19,20]. These handouts served as another reminder for physicians to prioritize disclosure during clinic visits, while also providing families a resource for continuing the disclosure process outside the confines of the HIV clinic.
May 2019: Around this time, the project leader noticed that waiting for quarterly meetings to notify providers about lack of documentation of disclosure status led to potential delay in the disclosure process if a clinic visit for a YLWH took place before the next quarterly meeting. To prevent this delay, the project leader reviewed charts twice monthly and notified the responsible clinicians about their undisclosed YLWH lacking documentation of disclosure or a disclosure plan.
July 2019: The pediatric infectious disease fellows rotating in the HIV clinic noted that documented disclosure plans lacked sufficient detail needed to determine the extent to which disclosure had been discussed with patients and families, especially when the disclosure process was started by a different physician. The team decided to provide more elaborate documentation in the previously developed disclosure plan template to ensure clarity about what had or had not been discussed with undisclosed YLWH. The goal was to prompt a new provider taking over care of a YLWH to resume the process of disclosure as planned by the previous provider and to prevent repeating disclosure steps from prior visits, thus avoiding further delays in disclosure.
Figure 1.
The gray box highlights the section of the plan within the HIV clinic note template where providers are prompted to document disclosure status and plan.
Results
At baseline, 69 YLWH aged 3–25 years were followed up at the pediatric HIV clinic, and 47 (68%) of them were aged ≥11 years. Because YLWH were transitioned to adolescent HIV clinic throughout the study period, only 57 YLWH were followed in the pediatric HIV clinic by March 2020, and of those, 40 (70%) were aged ≥11 years.
Outcome measure
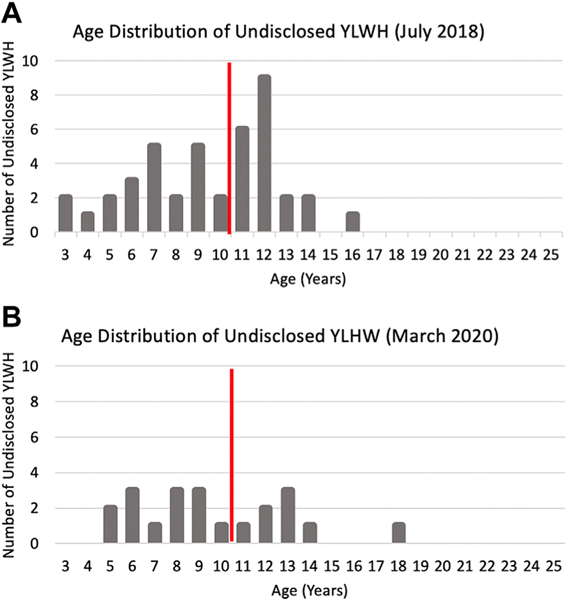
At baseline, 26/46 (57%) YLWH aged ≥11 years were disclosed to about their HIV status. Twenty months and six PDSA cycles after starting this project, 80% (32/40) of YLWH aged ≥11 years were disclosed to about their status (Figure 2). Of the eight YLWH aged ≥11 years who remained undisclosed, seven were aged 11–14 years (Figure 3). The remaining undisclosed YLWH in this group was an 18 year old with significant intellectual disability; although the importance of disclosure was discussed with the family, the provider and family made a joint decision to continue to further postpone nuanced conversations about the patient’s HIV status.
Figure 2.
The blue line represents the percentage of YLWH aged ≥11 years disclosed at the time represented on the horizontal axis, the red line represents the baseline percentage of disclosed YLWH before the initiation of the project (57%), and the green line represents the goal percentage of YLWH to be disclosed (≥80%). Gray arrows indicate the interventions/PDSA cycles.
Figure 3.
Panel A represents the distribution of ages of undisclosed YLWH before the start of the QI project, in July 2018. Panel B represents the distribution of undisclosed YLWH after the end of the QI project, in March 2020. The x-axes represent the age of YLWH, and the y-axes represent the number of undisclosed YLWH for each age. Undisclosed YLWH aged ≥11 years are represented to the right of the red vertical line.
Process measure
At the start of the project, none of the undisclosed patients (including YLWH aged ≤10 years) had a disclosure status or plan for disclosure documented in their medical record. Twenty months later,100% (21/21) of all undisclosed YLWH (regardless of age) had documentation of their disclosure status in the clinic note (Figure 4). Of note, after implementing the new note template, the percentage of undisclosed YLWH of all ages who had documentation of their disclosure status rapidly increased from 0% to over 90% in 8 months, which is at least in part a reflection that disclosure plans were previously in place but had not previously been documented.
Figure 4.
The blue line represents the percentage of undisclosed YLWH of all ages with documentation of their HIV status at the time represented on the horizontal axis, the red line represents the baseline percentage of undisclosed YLWH with documented status before the initiation of the project (0%), and the green line represents the goal percentage of undisclosed YLWH to have a documented status (100%). Gray arrows indicate the interventions/PDSA cycles.
Discussion
Increasing team prioritization of early discussions of disclosure of HIV status and implementation of various interventions were associated with substantial and rapid improvement in the disclosure process of YLWH in the pediatric HIV clinic. Disclosure is vital to successful transition to adolescent and young adult care to support optimal health outcomes as YLWH gain independence in their health care and may begin engaging in behaviors that increase the risk of transmission of HIV. Early disclosure is imperative to prevent sudden and traumatic disclosure. In addition, minors in our state are legally allowed to consent to certain medical decisions, such as sexually transmitted infection testing and treatment; thus, complete disclosure of their HIV status at an appropriate age may support their ability to make these decisions.
Implementation of the note template precipitated a dramatic increase in the percentage of undisclosed YLWH with documentation of their status; however, it is likely that the integration of all of the interventions promoted increased provider awareness of the importance of disclosure among other clinical priorities, and in turn, an overall increase in the number of older YLWH who were appropriately disclosed to about their HIV status. In addition, by achieving 100% documentation of YLWH undisclosed status, unintended disclosure by non-HIV providers caring for these children may be prevented, reducing the risk of potentially traumatic inadvertent disclosure. To further minimize the risk of inadvertent disclosure, a future system improvement that could be considered for implementation is the use of an EMR “flag,” including the disclosure status on the face sheet of patients’ medical records, thereby mitigating the need for providers to access the most recent HIV clinic note to know whether the patient is aware of their HIV status.
One of the barriers to initiating the disclosure process for undisclosed YLWH is the limited timeframe of a single clinic visit and the limited number of visits per year; physicians often have a number of clinical priorities to address in each visit, including medication adherence, medication dose adjustments, routine monitoring and screening labs, and acute complaints. The availability and incorporation of handouts geared toward caregivers assisted with overcoming this barrier by allowing for caregivers to spend more time thinking about the disclosure process and overcoming their hesitancy in between visits, thus facilitating and expediting conversations with the physicians. However, our team did not systematically track which families received these handouts. Doing so could help elucidate the impact of this intervention. Despite incorporation of educational handouts, more time and an increase in the number of individual clinic encounters may be necessary to surpass our primary goal in increasing disclosure status among YLWH aged ≥11 years.
However, a goal of 100% disclosed YLWH may not be achievable because of developmental delay or intellectual disability present in some of these adolescents. Owing to concern for lack of understanding of the disease process or social implications of HIV, disclosure is often postponed into late adolescence or young adulthood in individuals with cognitive limitations. Even if adolescents and young adults with cognitive delay continue to receive assistance from their caregivers in managing HIV, they remain at risk for unknowingly transmitting infection if they engage in high-risk behaviors. Moreover, a sudden accidental disclosure in a previously undisclosed adolescent with HIV can be traumatizing and lead to mistrust of their caregivers and support system. A qualitative study of children and adolescents living with HIV in Brazil supported a developmentally appropriate and stepwise disclosure process, which starts at childhood and continues at all ages, to reduce adverse effects of sudden disclosure [21]. Further studies evaluating effective methods to adapt a stepwise disclosure process for children and adolescents with developmental delay and intellectual disability are needed.
In addition to time constraints of clinic visits, parental hesitancy due to fear of stigma their child may face if they accidently reveal their HIV status to others contributed to delayed disclosure. In IB-YPHIV, culturally determined norms and community-level stigma, along with disclosure of maternal status and parental guilt regarding vertical transmission of HIV to their child, were also factors contributing to delayed disclosure [22]. The incorporation of handouts emphasizing the importance and effective ways of safely disclosing HIV status to YLWH and physicians spending more time with YLWH and their caregivers in clinic to address these issues is vital to overcoming these barriers. In addition, if caregivers are amenable to meeting with other caregivers of YLWH, caregiver support groups can facilitate the process of disclosure. Furthermore, family group psychotherapy has been shown to increase psychological well-being and decrease anxiety regarding the disclosure process in families [23]. Because physicians are not always specifically trained to assist families with the psychosocial support required to facilitate the disclosure process, HIV clinics should be supported by social workers, psychologists, and/or child-life specialists to assist with the disclosure process. Clinics should also consider employing peer advocates who are living with HIV and have completed the disclosure process to support families undergoing the process.
Limitations and future directions
Of note, we excluded YLWH who were transitioned to the adolescent HIV clinic, but disclosure of many of these patients took place at our pediatric clinic. Therefore, we likely underestimated the proportion of YLWH aged ≥11 years who underwent disclosure during our study period. We also collected cumulative data from our entire pediatric HIV clinic population rather than fragmented data focused on individual time periods, which led to less variation of the outcomes around the baseline median and, in turn, less certainty as to which interventions directly led to improvement. By only collecting aggregate data, we did not delineate demographic variability among our population. Additional studies comparing the rates of disclosure among children of varying sociodemographic backgrounds and between biological and adopted children would be helpful. Moreover, while our interventions helped drive age-appropriate disclosure, prior research on the effect of pediatric HIV disclosure on medication adherence is inconclusive [10]. Further longitudinal assessment of our population will be needed to determine if timely disclosure is associated with enhanced adherence and other improved patient outcomes such as viral suppression, retention in care, and disclosure-related stress and/or stigma.
Although this project enabled timely disclosure and identification of undisclosed patients, it did not identify the stage of disclosure of partially disclosed YLWH, who were considered undisclosed for the purpose of our initiative. It is possible that this lack of detail in documentation of disclosure status may lead to delays in complete disclosure if, within a group practice, a new provider, who is unfamiliar with the exact stage of disclosure, assumes care of these partially disclosed patients. Future interventions or PDSA cycles could include implementation of a standardized and stepwise disclosure process and a systemic approach to documentation of each step. For example, a staged cartoon book was developed to assist with the disclosure process for YLWH in Namibia, and this intervention greatly improved provider confidence with the disclosure process [24]. In the U.S., Cantrell et al. [25] developed a 10-stage structured framework of disclosure to adapt to young adolescents’ cognitive development and correlating progression of illness understanding. The sequential stages of disclosure were clearly described and easily followed by providers in their pediatric HIV clinic [25]. A standardized staged disclosure process, which takes into account factors such as the developmental status of YLWH and cultural values of IB-YPHIV, could help maintain or surpass the initial goals of this project and ensure adolescents who are in transition of responsibility for their health care are no longer undisclosed about their HIV status.
Conclusions
Implementation of strategies within the HIV care team to enhance disclosure, including regular meetings and a modified clinic note template, was associated with substantial increases in the proportion of YLWH with developmentally appropriate HIV disclosure and documentation of disclosure status. Future interventions to ensure optimal disclosure practices in the clinic will include adapting methods of stepwise disclosure that have been proven effective in other settings.
IMPLICATIONS AND CONTRIBUTION.
Developmentally appropriate disclosure of HIV status to school-aged youth living with HIV prepares them for optimal health outcomes as they gain independence in their health care as young adults. However, several factors may result in delayed or traumatic disclosure. Team awareness and systematic clinic-based interventions can effectively optimize the disclosure process for youth living with HIV.
Acknowledgments
This work was presented as a poster presentation at the Vanderbilt Symposium on Implementation Research in the Learning Health System in May 2019 and IDWeek in October 2019.
Funding Sources
Keerti Dantuluri was supported by the NIAID under the award number T32A1095202 (PI: Mark Denison).
Footnotes
Conflicts of interest: None of the authors have any conflicts of interest.
References
- [1].Hazra R, Siberry GK, Mofenson LM. Growing up with HIV: Children, adolescents, and young adults with perinatally acquired HIV infection. Annu Rev Med 2010;61:169–85. [DOI] [PubMed] [Google Scholar]
- [2].CDC. HIV surveillance report, 2018. (preliminary). Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance.html. Accessed March 13, 2020.
- [3].Nesheim SR, Linley L, Gray KM, et al. Country of birth of children with diagnosed HIV infection in the United States, 2008–2014. J Acquir Immune Defic Syndr 2018;77:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sabharwal S, Mitchell JW, Fan VY. Should there be a disclosure mandate for physicians caring for perinatally infected adolescents who don’t know their HIV serostatus? AMA J Ethics 2018;20:E743–9. [DOI] [PubMed] [Google Scholar]
- [5].WHO. Guideline on HIV disclosure counseling for children up to 12 years of age HIV/AIDS programme. 2011. Available at: https://www.who.int/hiv/pub/hiv_disclosure/en/. Accessed November 4, 2020. [PubMed]
- [6].AAP AIDS. Disclosure of illness status to children and adolescents with HIV infection. Pediatrics 1999;103:164–6. [DOI] [PubMed] [Google Scholar]
- [7].Siberry GK. Preventing and managing HIV infection in infants, children, and adolescents in the United States. Pediatr Rev 2014;35:268–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wiener LS, Battles HB. Untangling the web: A close look at diagnosis disclosure among HIV-infected adolescents. J Adolesc Health 2006;38: 307–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mellins CA, Brackis-Cott E, Dolezal C, et al. Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psychiatry 2002;7:101–14. [Google Scholar]
- [10].Wiener L, Mellins CA, Marhefka S, et al. Disclosure of an HIV diagnosis to children: History, current research, and future directions. J Dev Behav Pediatr 2007;28:155–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sisk BA, Bluebond-Langner M, Wiener L, et al. Prognostic disclosures to children: A historical perspective. Pediatrics 2016;138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Butler AM, Williams PL, Howland LC, et al. Impact of disclosure of HIV infection on health-related quality of life among children and adolescents with HIV infection. Pediatrics 2009;123:935–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Santamaria EK, Dolezal C, Marhefka SL, et al. Psychosocial implications of HIV serostatus disclosure to youth with perinatally acquired HIV. AIDS Patient Care STDS 2011;25:257–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Beima-Sofie KM, Brandt L, Hamunime N, et al. Pediatric HIV disclosure intervention improves knowledge and clinical outcomes in HIV-infected children in Namibia. J Acquir Immune Defic Syndr 2017;75:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Domek GJ. Debunking common barriers to pediatric HIV disclosure. J Trop Pediatr 2010;56:440–2. [DOI] [PubMed] [Google Scholar]
- [16].Klitzman R, Marhefka S, Mellins C, et al. Ethical issues concerning disclosures of HIV diagnoses to perinatally infected children and adolescents. J Clin Ethics 2008;19:31–42. [PMC free article] [PubMed] [Google Scholar]
- [17].Langley G. The improvement guide: A practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- [18].IHI. How to improve with the model for improvement. Available at: http://www.ihi.org/education/IHIOpenSchool/resources/Pages/QI-102-How-toImprove-with-the-Model-for-Improvement.aspx. Accessed January 30, 2020.
- [19].New York State Department of Health. Living with HIV. Caring for children with special needs. 2003. Available at: https://www.health.ny.gov/diseases/aids/general/resources/child/. Accessed November 4, 2020. [Google Scholar]
- [20].New York State Department of Health. Taking with young people about HIV and AIDS: A handbook for parents and caregivers. 2005. Available at: https://www.health.ny.gov/publications/0243.pdf. Accessed November 4, 2020.
- [21].Abadia-Barrero CE, Larusso MD. The disclosure model versus a developmental illness experience model for children and adolescents living with HIV/AIDS in Sao Paulo, Brazil. AIDS Patient Care STDS 2006;20:36–43. [DOI] [PubMed] [Google Scholar]
- [22].Fields EL, Bogart LM, Thurston IB, et al. Qualitative comparison of barriers to antiretroviral medication adherence among perinatally and behaviorally HIV-infected youth. Qual Health Res 2017;27:1177–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Nicastro E, Continisio GI, Storace C, et al. Family group psychotherapy to support the disclosure of HIV status to children and adolescents. AIDS Patient Care STDS 2013;27:363–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].O’Malley G, Beima-Sofie K, Feris L, et al. “If i take my medicine, i will be strong: ”evaluation of a pediatric HIV disclosure intervention in Namibia. J Acquir Immune Defic Syndr 2015;68:e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Cantrell K, Patel N, Mandrell B, et al. Pediatric HIV disclosure: A process-oriented framework. AIDS Educ Prev 2013;25:302–14. [DOI] [PubMed] [Google Scholar]