Abstract
The management of constitutional knee deformities may be a challenge. In most cases, the deformities are limited and accessible to conventional osteotomy techniques. This case reports an adult with extreme epiphyseal dysplasia of both distal femurs, and its management by a new osteotomy technique. At the last follow-up, 2.8 years after the previous surgery, the patient was walking without limitation or pain, and all osteotomies were healed. He had a Knee Society Score (KSS) of 57 and a functional KSS score of 100.
Keywords: Distal femoral osteotomy, Major valgus, Epiphyseal dysplasia
1. Introduction
The correction of congenital or acquired limb deformities may sometimes present a real medical and surgical challenge. This is the case of a 35-year-old refugee patient consulting for bilateral distal femoral epiphysometaphyseal dysplasias causing significant aesthetic and social distress.
The patient had these deformities since early childhood with progressive limb deviation during growth. He had unlimited walking, with a Knee Society Score (KSS) score of 18, and a functional KSS score of 100. On clinical examination, he had retained mobility with full extension and 90° flexion. He also had good adaptability with flexible hips proximally including 120° rotational mobility, healthy leg segments distally and flexible ankles. The patient's clinical presentation is described in Video 1.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.jcot.2023.102167
The following is the supplementary data related to this article.
Therefore, the deformity was essentially in the distal femur, with a 15° mechanical lateral distal femur (mLDFA) angle and 85° femoral anteversion in both sides, associated with permanent dislocation of the patella. An osteotomy technique had to be found that would: 1) restore the limb to its frontal and sagittal axes; 2) medialize the patella and extensor apparatus; 3) correct the excess anteversion of the femoral necks.
2. Surgical technique
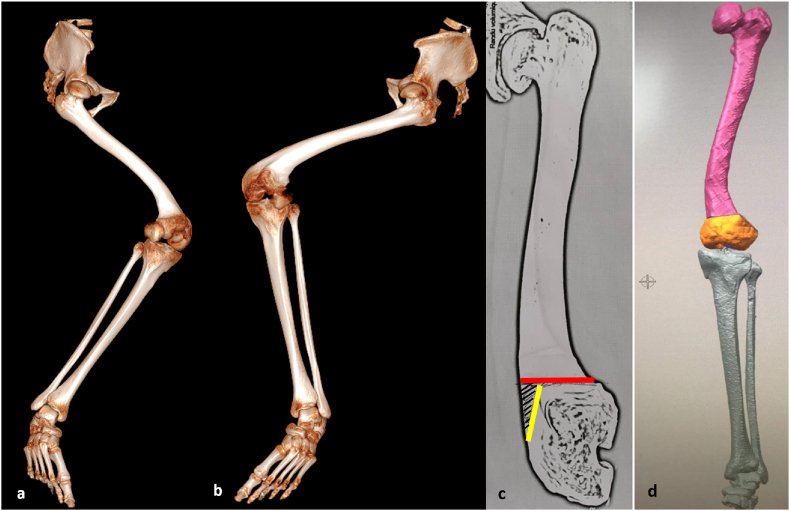
A three-dimensional simulation was used to arbitrarily define two cutting planes to align the epiphyses and diaphyses. A first cross-section was perpendicular to the femoral mechanical axis, and then a second sagittal section was made parallel to the distal condyles. The objective of this technique was to correct these deformities while maintaining maximum bone contact. Following this bilateral preoperative planning, custom-made cutting guides were made (Addidream, Limoges, France). The three-dimensional simulation of the osteotomy technique is reported in Fig. 1.
Fig. 1.
CT-scan images in three-dimensional bone reconstruction with front view of the right (a) and left (b) knees. Illustration of the two osteotomy lines (c). The hatched area represents the bone resection associated with this technique. Three-dimensional CT modeling to determine custom cutting guides (d).
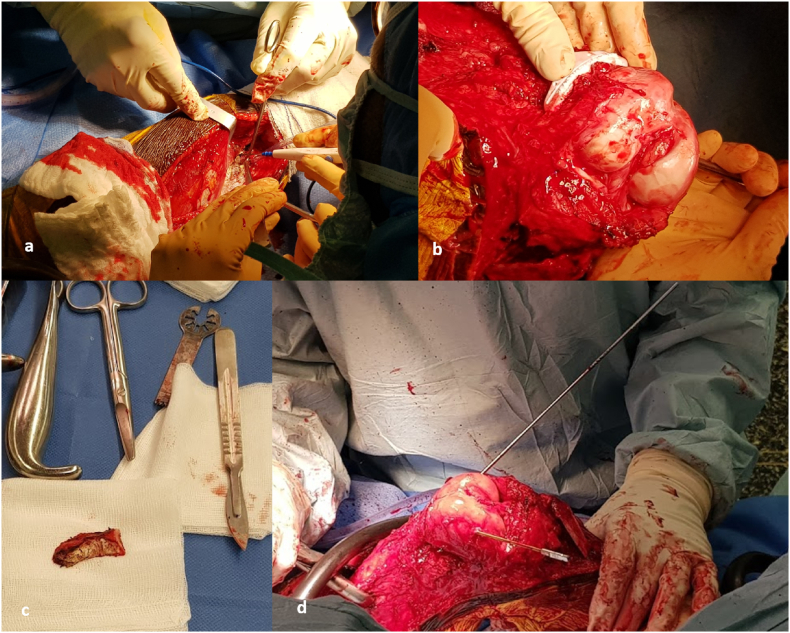
The same surgical strategy was used on both sides, six weeks apart. The approach used was lateral longitudinal from the greater trochanter to the anterior tibial tuberosity. The first step was the release of the extensor apparatus: lengthening of the fascia lata, tenotomy of the biceps femoris muscle, detachment of the entire quadriceps muscle from the femoral shaft, then elevation of the tibial tuberosity and excision of hoffa fat pad allowing medialization of the whole extensor apparatus. The cuts were then made using dedicated guides, starting with the cut perpendicular to the mechanical axis. Only one infracentimeter bone wedge was resected according to preoperative planning. The confrontation of these two cuts allowed us to straighten the deformity while allowing rotation around the horizontal plane to decrease femoral hyper anteversion to have symmetrical hip mobility in internal and external rotation. It was held in place by a cross screwing with 6.5 mm diameter cannulated screws (Stryker, Pusigna, France), then completed by a stainless-steel plate bent and curved to fit on the external femoral surface. At the end of the procedure, the anterior tibial tuberosity was repositioned with medialization and elevation to allow the release of the extensor apparatus and better patellar engagement. Illustrations of the surgical steps are reported in Fig. 2.
Fig. 2.
External approach with release of the extensor apparatus (a). Application of the custom-made cutting guide (b). Minimal bone resection slice (c). Result of osteotomy before cross pinning and plate synthesis (d).
3. Outcomes
In the post-operative follow-up of the right knee, the patient developed a deficit in the territory of the common fibular nerve, with spontaneous resolution at three months. The postoperative guidelines were identical on both sides: analgesic immobilization in a custom-made brace for 7 days postoperatively, then a six-week discharge was performed after each surgery. After this period, full support and active quadricipital strengthening were recommended. At the last follow-up, 2.8 years after the previous surgery, the patient was satisfied and was walking without limitation or pain. He had a KSS score of 57 and a functional KSS score of 100 (Fig. 3 and video 2). The mLDFA angles were 90° on the right and 91° on the left, respectively, with femoral anteversion measured by CT-scan of 12° on the right side and 9° on the left side. The patella has been partially medialized due to the absence of the femoral trochlea, allowing active knee extension. He had symmetrical mobilities with 10° flessum and 110° range of motion. Osteotomies were all healed at the last follow-up. X-rays at the last follow-up are reported in Fig. 4.
Fig. 3.
Clinical result at last follow-up. Full weight-bearing gait (a). Maximum bilateral flexion of 120° (b), and residual extension deficit of 10° (c).
Fig. 4.
Radiological findings at last follow-up (a), with profile radiographs of right (b) and left (c) knees.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.jcot.2023.102167
The following is the supplementary data related to this article.
4. Discussion
This clinical presentation required a multi-professional preoperative evaluation (surgeon, PRM physician, radiologist) to ensure no functional deterioration. To our knowledge, such an osteotomy has never been described in the literature. The particularity of this genetic dysplastic condition is the predominant involvement of the distal femoral epiphysis and metaphysis. To correct long bone deformities, opening or closing osteotomies are more frequently used,1, 2, 3 most often in the context of osteoarthritis and not of aesthetic or social discomfort.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 However, those techniques are limited in their corrective power and are not suitable for such deformities. It is also possible to propose staggered osteotomies for large deformities, which allows for a better distribution of the corrections. These osteotomies are particularly indicated in Paget's disease or osteogenesis imperfecta. In the present case, the focal nature of the deformity made these osteotomies unsuitable. Since the osteotomy line was centered on the metaphysis, curvilinear osteotomy could have been a solution by allowing realignment without lateral translation of the epiphysis. Finally, we could have chosen a custom-made osteosynthesis, but we preferred a synthesis with two transverse screws and a curved plate. This choice allowed us to adjust the synthesis with more flexibility than an anatomical plate.
Concerning the etiological assessment, the suspicion of deficiency dysplasia due to rickets was eliminated on the one hand because of the predominant involvement of the distal femur, and on the other hand because of the familial character. Indeed, his three children (two daughters and one son, for a median age of 5 years (ranging from 8 to 4 years)) presented identical damage, two by large valgus, and one in large varus (Fig. 5). After consultation with an expert geneticist, the most likely diagnosis was multiple epiphyseal dysplasia type 5, autosomal dominant.15 Unfortunately, the patient did not wish to undergo genetic testing which could have confirmed this clinical suspicion.
Fig. 5.
Family presentation of children with large valgus (a), or varus (b) deformities. Radiographs of child a from front (c) and side (d).
5. Conclusion
This osteotomy technique may be of interest in managing rare cases of complex distal femoral dysplasia with significant deformities in all three planes of space.
Declaration of competing interest
None.
References
- 1.Fujita K., Sawaguchi T., Goshima K., Shigemoto K., Iwai S. Influence of lateral hinge fractures on biplanar medial closing-wedge distal femoral osteotomy for valgus knee: a new classification of lateral hinge fracture. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-04212-4. [DOI] [PubMed] [Google Scholar]
- 2.Ishimatsu T., Takeuchi R., Ishikawa H., Maeyama A., Osawa K., Yamamoto T. Femoral morphology affects postoperative alignment of the lower extremities in hybrid closed-wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2022;142(12):3675–3685. doi: 10.1007/s00402-021-03974-1. [DOI] [PubMed] [Google Scholar]
- 3.Konrads C., Ahrend M.D., Beyer M.R., Stöckle U., Ahmad S.S. Rotation osteotomy of the distal femur influences coronal femoral alignment and the ischiofemoral space. Arch Orthop Trauma Surg. 2022;142(5):711–720. doi: 10.1007/s00402-020-03704-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sali E., Hardy A., Grimaud O., Meyer A. An original all-arthroscopic technique for bony fixation of lateral meniscus allograft via four tibial tunnels: a cadaver study. Orthop Traumatol Surg Res. 2018;104(8):1205–1208. doi: 10.1016/j.otsr.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Pasquier G.J.M., Huten D., Common H., Migaud H., Putman S. Extraction of total knee arthroplasty intramedullary stem extensions. Orthop Traumatol Surg Res. 2020;106(1S):S135–S147. doi: 10.1016/j.otsr.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Jones G.G., Clarke S., Jaere M., Cobb J.P. Failed high tibial osteotomy: a joint preserving alternative to total knee arthroplasty. Orthop Traumatol Surg Res. 2019;105(1):85–88. doi: 10.1016/j.otsr.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Denjean S., Chatain F., Tayot O. One-stage computer-assisted total knee arthroplasty and tibial osteotomy. Orthop Traumatol Surg Res. 2017;103(3):381–386. doi: 10.1016/j.otsr.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Tripon M., Sautet P., Argenson J.N., Jacquet C., Martz P., Ollivier M. Is the lateral tibial spine a reliable landmark for planning tibial or femoral valgus osteotomies? Orthop Traumatol Surg Res. 2022;108(3) doi: 10.1016/j.otsr.2022.103253. [DOI] [PubMed] [Google Scholar]
- 9.Nicolau X., Jenny J.Y., Bonnomet F., Ollivier M., Favreau H., Ehlinger M. Accuracy of the correction achieved after a valgus high tibial osteotomy: comparison of the Hernigou table and navigation. Orthop Traumatol Surg Res. 2022;108(3) doi: 10.1016/j.otsr.2022.103241. [DOI] [PubMed] [Google Scholar]
- 10.Sabnis B.M. A review of role of osteotomy in knee ligament injuries. J Clin Orthop Trauma. 2022;29 doi: 10.1016/j.jcot.2022.101891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lahoti O., Bansal M. Osteotomies for lateral compartment knee osteoarthritis. J Clin Orthop Trauma. 2021;25 doi: 10.1016/j.jcot.2021.101726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prakash J., Boruah T., Mehtani A., Chand S., Lal H. Experience of supracondylar cheveron osteotomy for genu valgum in 115 adolescent knees. J Clin Orthop Trauma. 2017;8(3):285–292. doi: 10.1016/j.jcot.2017.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tuhanioğlu Ü., Oğur H.U., Seyfettinoğlu F., Çiçek H., Gültekin A. High tibial osteotomy in obese patients: is successful surgery enough for a good outcome? J Clin Orthop Trauma. 2019;10(Suppl 1):S168–S173. doi: 10.1016/j.jcot.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yadav A.K., Parihar M., Pawar E.D., Ahuja D., Gavhale S., Khanna V. Functional outcome of high tibial osteotomy in patients with medial compartment osteoarthritis using dynamic axial fixator -a prospective study. J Clin Orthop Trauma. 2020;11(Suppl 5):S902–S908. doi: 10.1016/j.jcot.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briggs M.D., Wright M.J., Mortier G.R. GeneReviews®; Seattle: 2003. Multiple Epiphyseal Dysplasia, Autosomal Dominant. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.