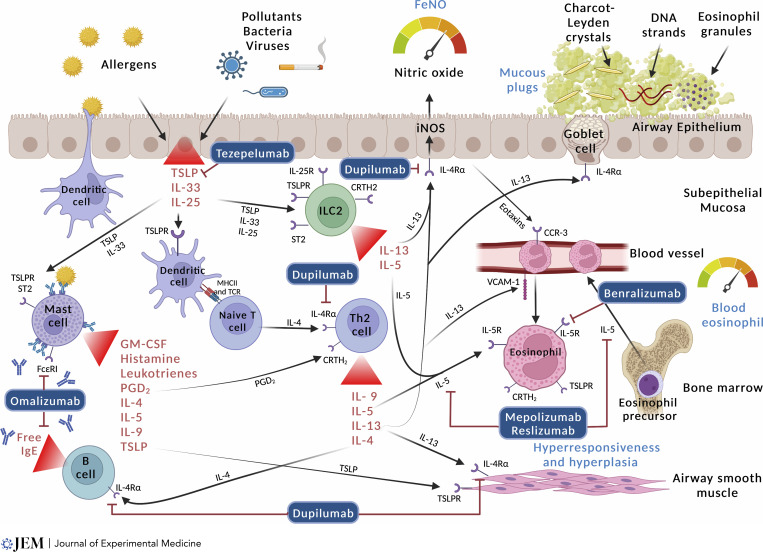
Figure 1.
Type 2 inflammation in asthma and targets for monoclonal antibody treatment. Type 2-high inflammation is the predominant treatable trait in asthma. It is present in both childhood-onset allergic asthma and adult-onset eosinophilic asthma. Different people have different pathways that predominate, and our understanding of why these develop and how to best characterize their activity is developing. In allergen-sensitized people, DCs present inhaled aeroallergens to tissue-resident CD4+ type 2 helper T lymphocytes (Th2 lymphocytes). These produce a large amount of type 2 cytokines (IL-4, IL-5, IL-13, and IL-9). In parallel, alarmins also stimulate the Th2 lymphocyte pathway, as well as ILC2, to produce type 2 cytokines. IL-4 and IL-13 stimulate B cells to mature into plasma cells and secrete IgE. IgE binds to the high-affinity FcεRI on mast cells, leading them to release PGD2 and histamine amongst other cytokines causing bronchoconstriction. Additionally, IL-13 induces the production of nitric oxide via the iNOS enzyme. This process can be measured by FeNO. IL-13 also stimulates mucous hypersecretion and smooth muscle contraction, and both IL-4 and IL-13 facilitate the recruitment of eosinophils from circulation to the airway mucosa. IL-5 enhances the proliferation and activation of eosinophils which degranulate causing tissue damage and producing mucous plugs through the formation of CLCs, eosinophil granules, and eosinophil extracellular traps.