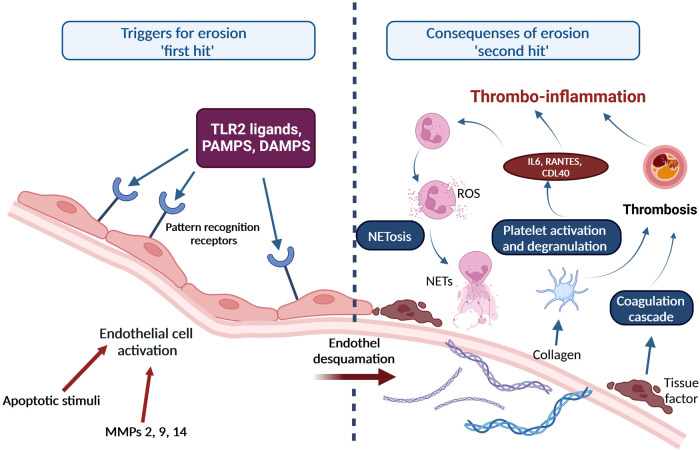
Figure 2.
“Two-hit” theory of development of atherosclerotic lesions involving NETosis and thrombo-inflammation. Upon endothelial cell activation by MMPs or apoptotic stimuli, pathogen-associated molecular patterns (PAMPs), danger-associated molecular patterns (DAMPs) and other ligands bind to pattern recognition receptors on the surface of endothelial cells. Subsequently, inflammatory cells and modified lipoproteins promote apoptosis of endothelial cells. In parallel, matrix metalloproteinases attack constituents of the basement membrane, which leads to disruption of the endothelial cell adhesion to the basement membrane, desquamation of the endothelium, and superficial erosion (first “hit”). Several processes are initiated once the endothelial erosion starts: (1) A desquamated and dying endothelial cell releases microparticles that bear tissue factor which initiates the blood coagulation cascade; (2) Exposed sub-endothelial matrix provides a substrate for neutrophil adhesion and activation, which results in neutrophil death and formation of NETs; (3) Exposure of the sub-endothelial extracellular matrix macromolecules activates platelets causing them to degranulate and release pro-inflammatory mediators, e.g. interleukin-6 (IL-6), RANTES, plasminogen activator inhibitor-1 (PAI-1), which enhances thrombosis, activates neutrophils and further promotes NETosis, a concept named thrombo-inflammation. Adapted from Quillard et al. (64) Created with BioRender.com.