Abstract
Background
The COVID-19 pandemic has led to an increased workload and work pressure on nurses owing to the unpredictable changes during this challenging situation. Herein, we explored the relationship between hopelessness and job burnout in nurses working in China against the backdrop of the COVID-19 outbreak.
Method
This was a cross-sectional study involving 1216 nurses in two hospitals in Anhui Province. The data was collected using an online survey. The mediation and moderation model was constructed, and the data was analyzed using SPSS PROCESS macro software.
Results
Our results showed that the nurses had an average job burnout score of 1.75 ± 0.85. Further analysis revealed a negative correlation between hopelessness and career calling (r = −0.551, P < 0.01) and a positive correlation between hopelessness and job burnout (r = 0.133, P < 0.01). Additionally, a negative correlation was demonstrated between career calling and job burnout (r = −0.138, P < 0.01). Moreover, career calling strongly mediated (by 40.9%) the relationship between hopelessness and job burnout in the nurses. Finally, social isolation in the nurses was a moderating factor for the association between hopelessness and job burnout (β = 0.028, t = 2.851, P < 0.01).
Conclusion
Burnout severity in nurses increased during the COVID-19 pandemic. Career calling mediated the relationship between hopelessness and burnout, with greater burnout levels in nurses who experienced social isolation. Therefore, we suggest that job burnout in nurses can be improved by mitigating the effects of hopelessness and social isolation through psychological interventions and enhancing their sense of career calling through education to strengthen their professional identity.
Keywords: COVID-19, Job burnout, Hopelessness, Career calling, Nurses, Social isolation
1. Introduction
Job burnout is a state of physical and mental fatigue, low work enthusiasm, and emotional exhaustion caused by excessive work demands [1]. Medical staff are often overburdened with work and are constantly under high physical and mental pressure. Under these conditions, the risk of job burnout is extremely high in nurses [2]. Several studies have demonstrated that job burnout was highly prevalent in medical staff during the COVID-19 pandemic [3,4]. Moreover, burnout reduces the self-efficacy of medical staff and promotes depression, irritability, helplessness, and anxiety, affecting their mental health status and decreasing work efficiency [5]. Additionally, some studies have shown that people with severe burnout can develop suicidal behavior [6]. The resulting poor delivery of good quality medical services and the risk of medical accidents can cause irreversible consequences to the affected individuals and patients [7]. Therefore, understanding job burnout in nurses and implementing corresponding interventions could improve the health, reduce the turnover rate, and stabilize the nursing teams [8]. Most previous studies have focused on the incidence of burnout in nurses; however, its underlying mechanisms remain less explored. Furthermore, scarce research has been conducted on the relationship between salient psychological factors and burnout during COVID-19. Therefore, in this study, we aimed to explore the current situation of nurse burnout due to the COVID-19 pandemic and to analyze its underlying mechanisms to provide a theoretical basis and empirical support for developing strategies to alleviate burnout in this group of healthcare professionals.
1.1. Theoretical background and hypothesis
1.1.1. Correlation of hopelessness and job burnout
Studies have shown that individuals with hopelessness can be apathetic and unable to cope with stressful situations, suggesting that hopelessness is closely related to job burnout [9]. Hopelessness refers to a state of constant negative expectations and uncertainty about positive outcomes for future events [10]. According to the job demand-control theory [11], employees experience hopelessness when faced with tasks of high job demand, low job control, and low social support for a long time and have no choice, eventually leading to burnout [12,13]. Previous study on police officers also corroborates the correlation between hopelessness and job burnout [14]. During the COVID-19 outbreak, the workload and work pressure on nurses continually increased owing to the unpredictable changes that arose, including a sharp increase in infected patients and negative public opinion. Furthermore, a negative attitude towards the pandemic-associated changes led to hopelessness in nurses, causing job burnout. Hopelessness has been shown to impair judgment ability and create a negative cognitive evaluation of life, thereby inducing an overall dissatisfaction with life [15,16]. Based on the conservation of resources theory, burnout may occur due to the perceived or actual loss of these resources [17]. During the COVID-19 pandemic, nursing staff were under a high workload and stress for a long period [18], which could have caused individual exhaustion and accelerated emotional depletion. Furthermore, the recurring and unpredictable development of the pandemic might have caused nursing staff to experience increased mental stress, reducing their aspiration and enthusiasm for nursing work and consequently resulting in burnout.
1.1.2. Career calling as a mediator between hopelessness and job burnout
Multiple factors influence the association between hopelessness and job burnout. Career calling is a strong passion towards a particular job, recognition of one’s occupation, and a sense of delivering quality work [19], which helps an individual’s career development [20]. According to the job demand-control theory, job control involves an employee's autonomy in making decisions at work, with individuals having a high sense of career calling exhibiting great self-control in the work process and demonstrating relatively better performance at work [21]. During the COVID-19 situation, the increasing number of infected cases and patient deaths might have led to an increasing sense of powerlessness and even hopelessness in the nurses. Nurses were reported to show a low enthusiasm for work and had become emotionally sensitive, irritable, and hopeless about the future, along with a sense of doubtfulness regarding the meaning and value of their work [22], which could have affected their career calling. The person-environment fit theory also states that when employees' skills are not matched to the requirements of the job, individuals develop a negative work experience and a low level of job meaning [23]. The study points out that such a state of work is not conducive to employees finding the right job role, nor is it conducive to a high level of integration with the profession, reducing the employee's career calling [24,25]. Therefore, we hypothesized that hopelessness negatively correlates with the sense of career calling.
Previous research has indicated that career calling is closely related to burnout and that an increased sense of career calling leads to improved work enthusiasm and job satisfaction in individuals, thereby reducing burnout [26]. Individuals with a sense of career calling have a high degree of alignment between work and self-concept, and career calling imparts a strong sense of value and meaning to work. The role of career calling was supported by resource conservation theory and previous research. Under the influence of career calling, employees allocate more of their psychological resources to tasks, do their best at jobs, have high job satisfaction and less burnout [27]. Similarly, during the COVID-19 pandemic, nurses with a strong sense of career calling would have instinctively spent more time at work, complained less [28], and experienced a strong meaning and value in their work, which could have mitigated job burnout. Based on the above findings, we hypothesized that career calling negatively correlates with job burnout and potentially influences the relationship between hopelessness and job burnout.
1.2. Social isolation as a moderator variable in the association between hopelessness and job burnout
As mentioned above, the argument that hopelessness positively affects burnout is reasonable and acceptable. However, the theoretical association between variables may not be valid in all cases, as a variety of contingent or contextual variables may influence the relationship. Based on the Chinese government's policy on the management of health care workers during the COVID-19, we hypothesise that whether or not one is centrally isolated is a potential moderator.
Social isolation such as seclusion have been known to lead to reduced physical activity, altered dietary habits, smoking and alcohol consumption, and changes in family relationships and work habits, ultimately affecting an individual’s quality of life and psychological well-being [29]. During the COVID-19 outbreak, China adopted strict quarantine and pandemic prevention measures to curb the spread of this infectious disease. However, several studies demonstrated that many hospitalized and quarantined patients with COVID-19 as well as medical staff exhibited anxiety and depression symptoms [30,31]. Consequently, excess workload coupled with social isolation induced a sense of hopelessness, depression, anxiety, fatigue, and mental exhaustion [32]. Based on these findings, we hypothesized that social isolation is a moderating factor in the relationship between hopelessness and job burnout.
1.3. Hypothesis
Based on the literature review, we propose the following hypotheses (Fig. 1):
Hypothesis 1
Hopelessness is positively correlated with job burnout in nurses.
Hypothesis 2
Career calling is a mediating factor in the relationship between hopelessness and job burnout in nurses.
Hypothesis 3
Social isolation moderates the relationship between hopelessness and job burnout in nurses.
Fig. 1.
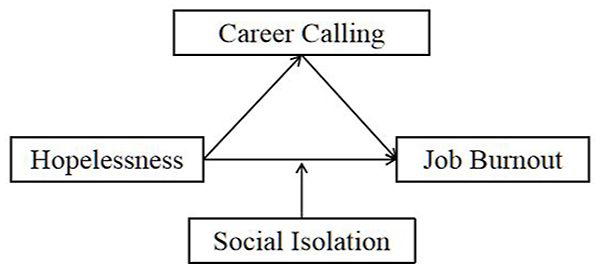
A hypothetical conceptual model explaining job burnout in nurses during the COVID-19 pandemic.
2. Methods
2.1. Participants
Using the convenience sampling method, 1250 nursing staff from the First Affiliated Hospital and the Second Affiliated Hospital of Anhui Medical University in China were selected from January 2022 to April 2022. The participants were included based on the following inclusion criteria: (1) clinically active registered nurses and (2) nursing staff in front-line departments, such as fever outpatient clinics, emergency departments, respiratory departments, and isolation wards, who were involved in the anti-epidemic work. The participants were excluded if they met any of the following exclusion criteria: (1) probationary, internship, or regulation nursing staff, (2) nursing staff with pregnancy or lactation, or (3) nursing staff working part-time in other jobs or on leave during the data collection period. Members of the team contacted the nursing departments of the two hospitals prior to the survey and, after obtaining their consent and support, created an online questionnaire. A link to the questionnaire was sent to the person in charge to explain the purpose of the study and the content of the questionnaire and to give uniform guidance. The survey was conducted on the Questionnaire Star platform and via the internet, breaking through the limitations of time and space. The survey process was also manipulated with a text version of the instructions, a set time for answering questions and pre and post repeated measures, thus increasing its internal effect. A total of 1250 nurses participated in the two hospitals. 34 invalid questionnaires were excluded according to the data exclusion criteria, resulting in 1216 valid questionnaires and a valid return rate of 97.28%. The respondents included 249 male and 967 female participants. Among them, 657 nursing staff had undergone social isolation from the beginning of the pandemic to the present, whereas 559 had not experienced social isolation. This study was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University (PJ2022-01-13). All respondents provided informed consent and voluntarily participated in the survey. The current study was performed in line with the principles of the 1964 Helsinki Declaration (including its later amendments or comparable ethical standards).
2.2. Measures obtained from the survey
2.2.1. Measure of hopelessness
Hopelessness in the nurses was measured using the Beck Hopelessness Scale [33], with a scoring system consisting of 20 items with “yes” (0) or “no” (2) choices, such as Item1 I am full of hope and enthusiasm for the future. The hopelessness level in respondents is grouped according to the total score into the following four grades: 0–3 indicates a normal level of hopelessness; 4–8, mild hopelessness; 9–14, moderate hopelessness; and 14 or above, severe hopelessness. We employed a scale that was validated and found to be highly reliable and accurate in the Chinese population [34,35]. The Cronbach’s α coefficient of the scale was 0.855.
2.2.2. Measure of career calling
The sense of career calling was determined using a revised scale proposed by Zhang Chunyu et al. [36]. The scale comprises 11 items (eg.Item1 My work should contribute to the society.), and the responses range from 1 (strongly disagree) to 5 (strongly agree). Therefore, the total scores can range from 11 to 55, with higher scores indicating a higher degree of career calling. The Cronbach’s α coefficient was 0.935.
2.2.3. Measure of job burnout
The Maslach Burnout Inventory-General Survey is used to evaluate job burnout in healthcare professionals [37]. In this study, a Chinese version of this instrument that has been validated and widely used was adopted [38]. This questionnaire contains three subscales, including emotional exhaustion (items 1–5, eg Item4 Working all day is really stressful for me), depersonalization (items 6–9), and low achievement (items 10–15), comprising 15 items. All items are rated on a 7-point Likert scale (0 = “never” to 6 = “very often”). The score of each of the three subscales is obtained by computing the mean of the sum of the items of the corresponding subscale. The total burnout score was grouped into no burnout (0–1.49), moderate burnout (1.50–3.49), and severe burnout (3.50–6.0) categories, with the moderate and severe burnout categories being classified as burnout groups. The Cronbach’s α coefficient was 0.727 for this scale.
2.2.4. Measure of social isolation
The Lubben Social Network Scale is commonly used to evaluate social isolation. However, this study investigated the nurses' social isolation under COVID-19 restrictions, which had its own specificity. Thus, this scale was not applicable to this research question. Nevertheless, a single-item questionnaire for assessing social isolation with high validity and sensitivity was demonstrated in numerous studies [39]. In the current study, a self-administered question, “Have you ever been centrally quarantined for at least a week because of your involvement in outbreak prevention and control?” was included in the general survey to ascertain the nursing staff's experience of social isolation, using a dichotomous “yes” or “no” response.
2.3. Statistical analysis
Data analyses for the descriptive analyses of the hopelessness level, sense of career calling level, and job burnout in the Chinese nurses were performed using SPSS Version 26.0. All data were tested to be normally distributed before being subjected to further statistical tests. Additionally, the relationships between hopelessness, career calling, and job burnout were evaluated using the Pearson correlation test. Furthermore, the effects of career calling and social isolation on the relationship between hopelessness and job burnout were analyzed using PROCESS Model 4 and Model 1. Lastly, the bootstrap method was also used to test for mediating effects (5000 repetitions of sampling). A two-tailed P-value of <0.05 was considered significant for all statistical tests used in this study.
3. Results
3.1. Common method bias
The data collected in this study were self-reported by the study participants. Thus, Harman’s single-factor test was adopted for the common method bias test. The results showed that eight factors had eigenvalues greater than 1, with the first factor accounting for 22.113% (<40%) of the variance. Moreover, the validation analysis of the single-factor model showed a poor model fit (X2/df = 9.142, RMSEA = 0.135, GFI = 0.438, AGFI = 0.384, RFI = 0.437, NFI = 0.450).
Therefore, no serious common methodological bias was indicated in this study.
3.2. Descriptive statistics and analysis
Table 1 presented the demographic characteristics of the participants. The correlation analysis revealed a negative correlation between hopelessness and career calling (r = −0.551, P < 0.01) and a positive correlation between hopelessness and job burnout (r = 0.133, P < 0.01). Moreover, career calling showed a negative correlation with job burnout (r = −0.138, P < 0.01). Furthermore, a positive correlation was found between hopelessness and social isolation (r = 0.074, P < 0.01). Similarly, job burnout had a negative correlation with social isolation (r = −0.128, P < 0.01), as shown in Table 2.
Table 1.
Demographic characteristics of the study participants (N = 1216).
| Variables | Group | No burnout (N, %) | Job burnout (N, %) |
|---|---|---|---|
| Gender | Male | 84 (33.7) | 165 (66.3) |
| Female | 377 (39.0) | 590 (61.0) | |
| Age | 18–30 | 217 (35.6) | 392 (64.4) |
| 31–40 | 92 (36.7) | 159 (63.3) | |
| 41–50 | 94 (41.4) | 133 (58.6) | |
| 51–60 | 58 (45.0) | 71 (55.0) | |
| Professional title | Senior | 231 (37.6) | 383 (62.4) |
| Supervisor | 142 (40.0) | 213 (60.0) | |
| Deputy or above | 88 (35.6) | 159 (64.4) | |
| Education | Specialties | 100 (39.2) | 155 (60.8) |
| Undergraduate | 216 (36.7) | 373 (63.3) | |
| Masters | 145 (39.0) | 227 (61.0) | |
| Marital status | Unmarried | 207 (41.4) | 293 (58.6) |
| Married | 166 (33.9) | 323 (66.1) | |
| Other | 88 (38.8) | 139 (61.2) |
Table 2.
Descriptive statistics and correlation analysis of each variable.
| Variables | M ± SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| 1. Social isolation | – | 1 | |||
| 2. Hopelessness | 10.18 ± 5.17 | 0.074** | 1 | ||
| 3. Job burnout | 1.75 ± 0.85 | −0.036 | 0.133** | 1 | |
| 4. Career calling | 37.06 ± 10.72 | −0.128** | −0.551** | −0.138** | 1 |
M ± SD, mean ± standard deviation; **P < 0.01.
3.3. Mediation analysis
The results showed that hopelessness was positively correlated with job burnout (β = 0.022, t = 4.684, P < 0.01, 95% CI [confidence interval] = [0.013, 0.031]), supporting hypothesis 1. In hypothesis 2, the nurses' sense of career calling was assumed to affect the relationship between hopelessness and job burnout. hypothesis 2 was tested using the SPSS PROCESS Macro (Model 4). Hopelessness was found to be negatively correlated with career calling (β = −1.144, t = −23.028, P < 0.01) (Table 3). Finally, a negative correlation was revealed between career calling and job burnout (β = −0.007, t = −2.723, P < 0.01); thus, hypothesis 2 was supported (indirect effect = 0.009, SE = 0.003, 95% CI = [0.001, 0.015]). The mediation effect of the nurses' sense of career calling was 40.9% (Table 3, Table 4).
Table 3.
Summary of hierarchical regression analyses predicting job burnout.
| Regression equation |
Overall fit coefficient |
Regression coefficient |
|||||
|---|---|---|---|---|---|---|---|
| Outcome variables | Predictor variables | R | R2 | F | β | SE | t |
| Job burnout | Hopelessness | 0.133 | 0.018 | 21.942** | 0.022 | 0.005 | 4.684** |
| Career calling | Hopelessness | 0.551 | 0.304 | 530.309** | −1.144 | 0.050 | −23.028** |
| Job burnout | Career calling | 0.154 | 0.024 | 14.737** | −0.007 | 0.003 | −2.723** |
| Hopelessness | 0.013 | 0.006 | 2.417* | ||||
Note: *P < 0.05, **P < 0.01.
Table 4.
Direct and indirect effects of hopelessness on job burnout.
| β | SE | 95% CI | Ratio of effect values | |
|---|---|---|---|---|
| Total effect | 0.022 | 0.005 | [0.013, 0.031] | |
| Direct effect | 0.013 | 0.006 | [0.003, 0.024] | 59.1% |
| Mediating effect | 0.009 | 0.003 | [0.001, 0.015] | 40.9% |
Note: *P < 0.05, **P < 0.01.
3.4. Moderation effect analysis
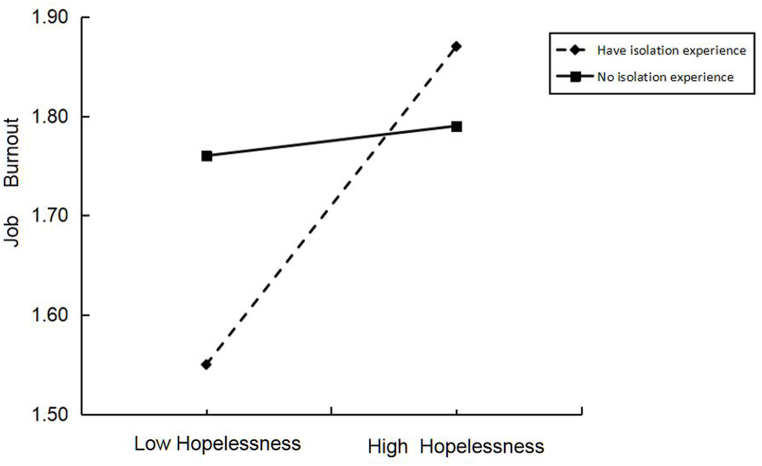
The moderating effect was analyzed using the SPSS PROCESS Macro (Model 1), and the results are shown in Table 5. The level of hopelessness and social isolation in nurses significantly predicted the job burnout level (β = 0.028, t = 2.851, P < 0.01), thereby supporting hypothesis 3. The simple slope test was performed to further explore the interaction between hopelessness, social isolation, and job burnout. As shown in Fig. 2, the effect of hopelessness on job burnout had a steeper slope for nurses who had experienced social seclusion, indicating that hopelessness was a significant predictor for job burnout. All these results suggest that the sense of career calling is a mediator in the interaction between hopelessness and job burnout, while the experience of social isolation moderates this relationship.
Table 5.
Test of the moderating effects.
| Regression equation |
Overall fit coefficient |
Regression coefficient |
|||||
|---|---|---|---|---|---|---|---|
| Outcome variables | Predictor variables | R | R2 | F | β | SE | t |
| Job burnout | Hopelessness | 0.163 | 0.026 | 10.958** | 0.004 | 0.008 | 0.507 |
| Social isolation | −0.359 | 0.110 | −3.276** | ||||
| Hopelessness × Social isolation | 0.028 | 0.010 | 2.851** | ||||
Note: *P < 0.05, **P < 0.01.
Fig. 2.
Moderating effect of social isolation on job burnout.
4. Discussion
The findings revealed that 755 nurses (62.1% of respondents) exhibited high levels of job burnout. Furthermore, the results of the mediating effect analysis revealed that career calling was a weak mediator of the relationship between hopelessness and job burnout. The results of the moderating effect analysis showed that social isolation increased the role of hopelessness on job burnout among nurses. These findings deepen our understanding of the impact of hopelessness and job burnout among nurses during the COVID-19 and provide empirical support and empirical evidence for improving nurses' psychological well-being and enhancing work engagement and quality of care during the latter part of the epidemic.
4.1. Relationship between hopelessness and job burnout
Our study results revealed a positive correlation between hopelessness and job burnout, consistent with previous findings [40,41]. The COVID-19 pandemic has not only affected the mental health of the general population but also that of health providers. Nurses were at a high risk of trauma and serious job burnout in the long term due to relatively higher workloads, work pressure, and work-related stress during this pandemic [42]. Nurses were and continue to be at the forefront of preventing and controlling the COVID-19 spread, where they experience a heavy workload and immense psychological pressure [43]. A stressful life has been demonstrated to induce hopelessness. Particularly, humans feel overwhelmed by prolonged mental stress, leading to hopelessness and disillusionment [44]. During the COVID-19 outbreak, nurses experiencing hopelessness were less enthusiastic about work, easily agitated, irritated, and indifferent to people and situations around them and displayed a negative attitude towards work, with little value for their work. All these factors ultimately aggravated job burnout [45]. This result is supported by the job demands-resources theory, where job demands can create burnout and negative effects on individuals. Nurses were flooded with physical and mental stress and insecurity during the COVID-19, all of which contributed to burnout [46]. Based on this background, we recommend that the physical and mental health of nurses should be given attention. Furthermore, we suggest counselling and education for nurses to enable them to cope with work pressure and maintain a positive attitude against even high-pressure situations. These interventions could help reduce burnout in this group of healthcare providers.
4.2. Mediating effect of career calling
We found that career calling mediated the relationship between hopelessness and job burnout. That is, hopelessness impacts on job burnout by influencing career calling. The results showed a negative association between hopelessness and career calling, which aligned with previous research findings [47]. Empirical studies have shown that hopelessness impairs the cognitive evaluation of life events. Therefore, hopelessness could be closely related to life dissatisfaction [48]. Additionally, hopelessness can cause emotional, physical, and mental exhaustion, leading to job burnout that lowers the sense of career calling [49]. Additionally, we found that career calling negatively correlated with job burnout, indicating that a low sense of career calling increased the probability of job burnout, similar to a previous study result [50].
Resource conservation theory states that when individuals are affected by negative emotions, they consume more attentional resources [17]. Fewer resources are allocated to the work, leaving the individual unable to value the work and with a reduced career calling. The nurse's career calling decreases, as does her enthusiasm and commitment to her work. At the same time, a lack of recognition of one's own values occurs, and negative and indifferent attitudes and behaviors towards patients are displayed [51], ultimately increasing burnout [52].
During the COVID-19 pandemic, nurses were faced with a dramatic increase in infected patients and a sense of powerlessness in failing to save patients' ears, and these negative emotions and work stresses increased the sense of hopelessness among nurses. The high level of hopelessness takes away from the psychological resources of nurses and prevents them from being fully engaged in their work, leading to a reduced sense of self-worth and career calling. This further increases the likelihood that they will deviate from professional norms, thereby endangering the lives of patients and their professional development.
Therefore, hospital managers should pay attention to the cultivation and shaping of nurses' career calling. They can offer career management courses for staff, provide targeted guidance and design for staff's personal career development, and at the same time combine staff's personality, interests, values, strengths and abilities to prompt them to form a clear perception of career development and guide them to actively pursue their own career calling.
4.3. Moderating role of social isolation
Our results showed that social isolation affected the association between hopelessness and job burnout, wherein nurses who had undergone social isolation displayed greater levels of hopelessness and job burnout severity than those who had not experienced social isolation. Studies have shown that during the COVID-19 outbreak, patients and medical workers who had maintained social isolation were more prone to mental health problems, anxiety, and depression [53,54]. Residing in a cramped and unfamiliar living environment for a long time can lead to nurses developing negative emotions such as anxiety and depression [55], while repeated isolation experiences may trigger trauma symptoms [56]. Furthermore, the lack of direct contact with friends and family can reduce nurses' social support and enthusiasm for work, increasing the likelihood of them experiencing emotional imbalance and burnout [57].
Therefore, attention should be paid to nurses who have experienced social isolation to understand their psychological status promptly. Additionally, they should receive the appropriate organizational support and emotional care to alleviate their work stress and reduce burnout.
5. Implications
This study expands our understanding of the effect of hopelessness on nurse burnout during public health emergencies. Previous studies were conducted in a controlled setting; however, data collection in this study was performed during the COVID-19 pandemic. Therefore, our study results are more reflective of the real-world situation. Furthermore, the present study analyzed the mediating role of career calling and the moderating role of social isolation in nurses. The results revealed that increased hopelessness negatively affects career calling and positively influences job burnout in nurses.
In the case of remedial measures, strategies focused on the relationship between the four variables of hopelessness, career calling, job burnout, and social isolation may enable nursing administrators to more efficiently reduce job burnout and improve mental health in nurses during the post-pandemic period. Moreover, staff career management courses can be offered to provide targeted guidance and design for their personal career development, so as to guide them to actively pursue their own career calling and subsequently improve the level of burnout among nurses. Particular attention should be paid to nurses who have been centrally isolated, and more attention should be paid to their psychological health, and their psychological capacity should be enhanced through individual psychological counselling and group psychological counselling as appropriate.
6. Limitations and future directions
This study has a few limitations that must be considered. First, this was a cross-sectional study; therefore, the cause-effect relationships could not be inferred. To address this shortcoming, future longitudinal studies are required to explore the causality of the hypotheses proposed in this study. Second, all the data collected in this study were self-reported responses. This measurement method is subjectively influenced by the topic of the study, which may have led to a focus on the measurement results. Future studies should collect data from multiple healthcare professionals to obtain more inclusive findings. Finally, the nurses included in this study were drawn from a small geographical region. Thus, the study findings may not represent the situation among nurses from other areas. Therefore, further multicenter studies are necessary to validate our findings.
7. Conclusion
Our study results showed that the sense of career calling influences the association between hopelessness and job burnout in nurses. Furthermore, social isolation is a mediating factor in the relationship between hopelessness and burnout. Overall, job burnout in nurses was a critical outcome during the COVID-19 pandemic. Therefore, proactive measures taken by hospital managers, such as ensuring adequate nursing staff, enhancing education on the career calling of nurses and focusing on enhancing the psychological competence of nurses who have experienced isolation can help improve job burnout.
Author contribution statement
Yinhua Zhang: Jiangying Han: Conceived and designed the experiments; Wrote the paper.
Dalin Kuang: Juan Ren: Performed the experiments.
Biaoxin Zhang: Yehai Liu: Analyzed and interpreted the data.
Lijuan Chen: Lin Ning: Xinxin Xie: Contributed reagents, materials, analysis tools or data.
Funding statement
This research was funded by the National Natural Science Foundation of China (82171127).
Data availability statement
Data will be made available on request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e16898.
Contributor Information
Yinhua Zhang, Email: aydyyzyh@sina.com.
Dalin Kuang, Email: 2574219604@qq.com.
Biaoxin Zhang, Email: 532611328@qq.com.
Yehai Liu, Email: liuyehai616@qq.com.
Juan Ren, Email: 1115496657@qq.com.
Lijuan Chen, Email: 105952064@qq.com.
Lin Ning, Email: 393649923@qq.com.
Xinxin Xie, Email: 562115712@qq.com.
Jiangying Han, Email: hanjy7228@163.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu. Rev. Psychol. 2003;52(1):397. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.Zhang W., et al. 2021. Effects of Optimism on Work Satisfaction Among Nurses: A Mediation Model through Work-Family Conflict; p. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medak E., Niedzielski U. 2021. Effects of COVID-19 on Doctors Burnout. (3) [Google Scholar]
- 4.Elhadi M., et al. 2020. Burnout Syndrome Among Hospital Healthcare Workers during the COVID-19 Pandemic and Civil War: A Cross-Sectional Study; p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adriano, et al. 2019. Stress and Burnout Syndrome and Their Associations with Coping and Job Satisfaction in Critical Care Nurses: a Literature Review. [PubMed] [Google Scholar]
- 6.Pompili M., et al. Car accidents as a method of suicide: a comprehensive overview. Forensic Sci. Int. 2012;223(1):1–9. doi: 10.1016/j.forsciint.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Huang C., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Labrague L.J., et al. Organizational politics, nurses' stress, burnout levels, turnover intention and job satisfaction. Int. Nurs. Rev. 2017;64(1):109–116. doi: 10.1111/inr.12347. [DOI] [PubMed] [Google Scholar]
- 9.Amanullah S., Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel) 2020;8(4) doi: 10.3390/healthcare8040421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mac Giollabhui N., et al. The development of future orientation is associated with faster decline in hopelessness during adolescence. J. Youth Adolesc. 2018;47(10):2129–2142. doi: 10.1007/s10964-017-0803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Häusser J.A., Schulz-Hardt S., Mojzisch A. The active learning hypothesis of the job-demand-control model: an experimental examination. Ergonomics. 2014;57(1):23–33. doi: 10.1080/00140139.2013.854929. [DOI] [PubMed] [Google Scholar]
- 12.Dean R.K., Pollard R.Q., Jr. Application of demand-control theory to sign language interpreting: implications for stress and interpreter training. J. Deaf Stud. Deaf Educ. 2001;6(1):1–14. doi: 10.1093/deafed/6.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Häusser, J., et al., Taylor & Francis Online :: Ten years on: a review of recent research on the Job Demand–Control (-Support) model and psychological well-being - Work. Stress - Volume 24, Issue 1.
- 14.Civilotti C., et al. Hopelessness in police officers and its association with depression and burnout: a pilot study. Int. J. Environ. Res. Publ. Health. 2022;19(9) doi: 10.3390/ijerph19095169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim C.H., Jayathilake K., Meltzer H.Y. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr. Res. 2003;60(1):71–80. doi: 10.1016/s0920-9964(02)00310-9. [DOI] [PubMed] [Google Scholar]
- 16.Karagöl A., Törenli Kaya Z. Healthcare workers' burn-out, hopelessness, fear of COVID-19 and perceived social support levels. Eur. J. Psychiatr. 2022;36(3):200–206. doi: 10.1016/j.ejpsy.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prapanjaroensin A., Patrician P.A., Vance D.E. Conservation of resources theory in nurse burnout and patient safety. J. Adv. Nurs. 2017;73(11):2558–2565. doi: 10.1111/jan.13348. [DOI] [PubMed] [Google Scholar]
- 18.Karampelias V., Karonis D., Psaroudi V. The psycho-emotional impact of COVID-19 on surgical staff working in emergency departments. Eur. J. Trauma Emerg. Surg. 2020;46(4):747–749. doi: 10.1007/s00068-020-01411-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peng J., et al. Career calling and job satisfaction in army officers: a multiple mediating model analysis. Psychol. Rep. 2020;123(6):2459–2478. doi: 10.1177/0033294119862990. [DOI] [PubMed] [Google Scholar]
- 20.Soto-Rubio A., Giménez-Espert M.D.C., Prado-Gascó V. Effect of emotional intelligence and psychosocial risks on burnout, job satisfaction, and nurses' health during the COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2020;17(21) doi: 10.3390/ijerph17217998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang X., et al. Career calling as the mediator and moderator of job demands and job resources for job satisfaction in health workers: a cross-sectional study. Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.856997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaw S.C.K. Hopelessness, helplessness and resilience: the importance of safeguarding our trainees' mental wellbeing during the COVID-19 pandemic. Nurse Educ. Pract. 2020;44 doi: 10.1016/j.nepr.2020.102780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kristof A.L. Person‐organization fit: an integrative review of its conceptualizations, measurement, and implications. Person. Psychol. 2010;49(1):1–49. [Google Scholar]
- 24.Harzer C., Ruch W. When the job is a calling: the role of applying one's signature strengths at work. J. Posit. Psychol. 2012;7(5):362–371. [Google Scholar]
- 25.Allan B.A., Duffy R.D. Examining moderators of signature strengths use and well-being: calling and signature strengths level. J. Happiness Stud. 2014;15(2):323–337. [Google Scholar]
- 26.Chen Y.C., et al. Exploring the relationships among professional quality of life, personal quality of life and resignation in the nursing profession. J. Adv. Nurs. 2021;77(6):2689–2699. doi: 10.1111/jan.14770. [DOI] [PubMed] [Google Scholar]
- 27.Duffy R.D., et al. Calling and life satisfaction: it's not about having it, it's about living it. J. Counsel. Psychol. 2013;60(1):42–52. doi: 10.1037/a0030635. [DOI] [PubMed] [Google Scholar]
- 28.Duarte J., Pinto-Gouveia J., Cruz B. Relationships between nurses' empathy, self-compassion and dimensions of professional quality of life: a cross-sectional study. Int. J. Nurs. Stud. 2016;60:1–11. doi: 10.1016/j.ijnurstu.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Odone A., et al. COVID-19 lockdown impact on lifestyle habits of Italian adults. Acta Biomed. 2020;91(9-s):87–89. doi: 10.23750/abm.v91i9-S.10122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pappa S., et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo Q., et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Molina-Praena J., et al. Levels of burnout and risk factors in medical area nurses: a meta-analytic study. Int. J. Environ. Res. Publ. Health. 2018;15(12) doi: 10.3390/ijerph15122800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kocalevent R.D., et al. Standardization of the Beck hopelessness scale in the general population. J. Ment. Health. 2017;26(6):516–522. doi: 10.1080/09638237.2016.1244717. [DOI] [PubMed] [Google Scholar]
- 34.Zhang W.C., et al. Beck hopelessness scale: psychometric properties among rural Chinese suicide attempters and non-attempters. Death Stud. 2015;39(7):442–446. doi: 10.1080/07481187.2014.970300. [DOI] [PubMed] [Google Scholar]
- 35.Ma Z., et al. Reliability and validity of short Beck Hopelessness Scale in psychological autopsy study among Chinese rural elderly. Int. Psychogeriatr. 2020;32(4):525–531. doi: 10.1017/S1041610219001315. [DOI] [PubMed] [Google Scholar]
- 36.Backman C.L. Occupational balance: exploring the relationships among daily occupations and their influence on well-being. Can. J. Occup. Ther. 2004;71(4):202–209. doi: 10.1177/000841740407100404. [DOI] [PubMed] [Google Scholar]
- 37.Maslach C. Research edition; 1981. Maslach Burnout Inventory. [Google Scholar]
- 38.Yang N., Lu J., Ye J. A novel framework based on the improved job demands-resources (JD-R) model to understand the impact of job characteristics on job burnout from the view of emotion regulation theory. Psychiatr. Danub. 2018;30(1):26–34. doi: 10.24869/psyd.2018.26. [DOI] [PubMed] [Google Scholar]
- 39.Zhang S.E., et al. Contribution of character strengths to psychology stress, sleep quality, and subjective health status in a sample of Chinese nurses. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.631459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pace E.M., et al. Experiences and outcomes of nurses referred to a peer health assistance program: recommendations for nursing management. J. Nurs. Manag. 2020;28(1):35–42. doi: 10.1111/jonm.12874. [DOI] [PubMed] [Google Scholar]
- 41.Chen Y.C., et al. Patient-nurse ratio is related to nurses' intention to leave their job through mediating factors of burnout and job dissatisfaction. Int. J. Environ. Res. Publ. Health. 2019;16(23) doi: 10.3390/ijerph16234801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen R., et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int. J. Ment. Health Nurs. 2021;30(1):102–116. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tarquinio C., et al. EMDR in telemental health counseling for healthcare workers caring for COVID-19 patients: a pilot study. Issues Ment. Health Nurs. 2021;42(1):3–14. doi: 10.1080/01612840.2020.1818014. [DOI] [PubMed] [Google Scholar]
- 44.Karadag E., et al. Attitudes of nurses in Turkey toward care of dying individual and the associated religious and cultural factors. J. Relig. Health. 2019;58(1):303–316. doi: 10.1007/s10943-018-0657-4. [DOI] [PubMed] [Google Scholar]
- 45.Vanhaecht K., et al. COVID-19 is having a destructive impact on health-care workers' mental well-being. Int. J. Qual. Health Care. 2021;33(1) doi: 10.1093/intqhc/mzaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phillips C. Relationships between workload perception, burnout, and intent to leave among medical-surgical nurses. Int. J. Evid. Base. Healthc. 2020;18(2):265–273. doi: 10.1097/XEB.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 47.Zhang S., et al. A cross-sectional study of job burnout, psychological attachment, and the career calling of Chinese doctors. BMC Health Serv. Res. 2020;20(1):193. doi: 10.1186/s12913-020-4996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Suh W.Y., et al. A network analysis of suicidal ideation, depressive symptoms, and subjective well-being in a community population. J. Psychiatr. Res. 2021;142:263–271. doi: 10.1016/j.jpsychires.2021.08.008. [DOI] [PubMed] [Google Scholar]
- 49.Hwang I.T., et al. I can’t see an end in sight.” how the COVID-19 pandemic may influence suicide risk. Crisis. 2022 doi: 10.1027/0227-5910/a000877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chae S.J., Jeong S.M., Chung Y.S. The mediating effect of calling on the relationship between medical school students' academic burnout and empathy. Korean J. Med. Educ. 2017;29(3):165–173. doi: 10.3946/kjme.2017.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Panagioti M., et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern. Med. 2018;178(10):1317–1331. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 52.Guo B., et al. The relationship between achievement motivation and job performance among Chinese physicians: a conditional process analysis. BioMed Res. Int. 2021;2021 doi: 10.1155/2021/6646980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Singh S., et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatr. Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Son C., et al. Effects of COVID-19 on college students' mental health in the United States: interview survey study. J. Med. Internet Res. 2020;22(9) doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dudek K.A., et al. Neurobiology of resilience in depression: immune and vascular insights from human and animal studies. Eur. J. Neurosci. 2021;53(1):183–221. doi: 10.1111/ejn.14547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walton M., Murray E., Christian M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care. 2020;9(3):241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu Y., et al. Job stress, psychological capital, perceived social support, and occupational burnout among hospital nurses. J. Nurs. Scholarsh. 2021;53(4):511–518. doi: 10.1111/jnu.12642. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.