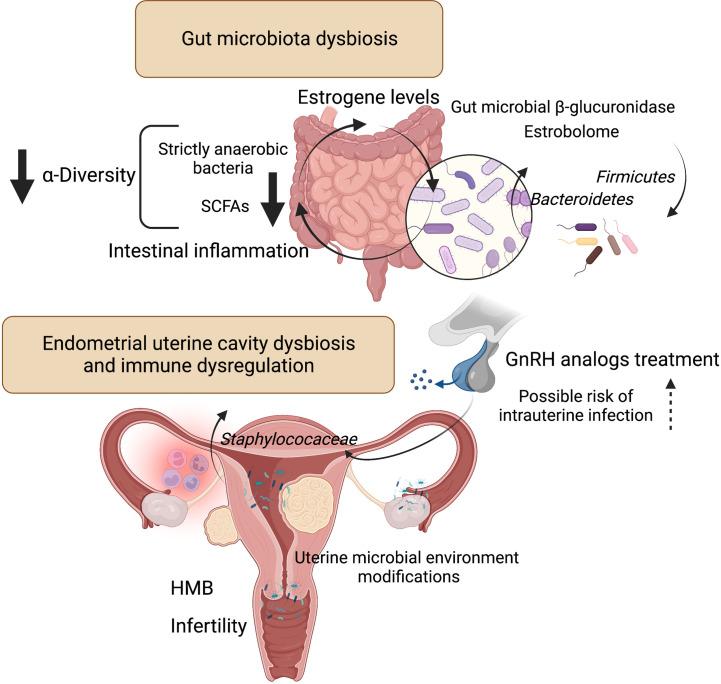
Figure 2.
Influence of microbiota on estrogen metabolism and endometrial uterine cavity dysbiosis in patients with uterine fibroids and possible role of GnRH analogs treatment. Liver-conjugated estrogens excreted in the bile into the gastrointestinal tract could be deconjugated by intestinal bacteria that produce ß-glucosidase enzymes involved in estrogen deconjugation. This leads to their absorption into the bloodstream and allows them to bind to estrogen receptors. However, the relationship is a bidirectional - the gut microflora can also be affected by estrogen. The experimental evidence for the key role of gut bacteria in estrogen metabolism was observed decades ago. The estrobolome is defined as the gene repertoire of intestinal microflora with products capable to metabolize estrogens. By influencing and modulating the intestinal and hepatic circulation of estrogens, the estrobolome affects the excretion and circulation of estrogens. Numerous evidence indicates that dysbiosis of intestinal bacteria increases the chance of intestinal inflammation. This is particularly related to a decrease in strictly anaerobic bacteria and a simultaneous increase in facultative anaerobes such as Escherichia coli and Klebsiella. And SCFAs, produced mainly by strict anaerobes, have anti-inflammatory effects. According to one study (Khan et al., 2016), intrauterine higher colonization by Staphylococaceae was revealed in a group of control patients who used GnRH analogs. Patients with fibroids after GnRH treatment had the highest staphylococcal levels compared to other groups. Figure 2 created with BioRender.com. Heavy menstrual bleeding (HMB); gonadotropin-releasing hormone (GnRH); short-chain fatty acids (SCFAs).