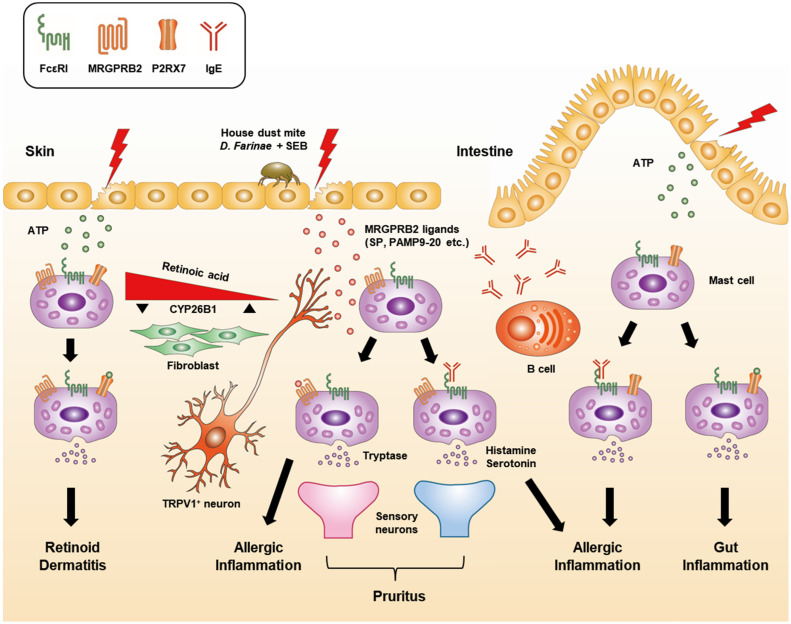
Figure 1.
Inflammatory responses to IgE-dependent and -independent mast cell degranulation in the skin and intestine. FcεRI is constitutively expressed by mast cells in all tissues and plays a central role in allergic responses via its involvement in the IgE-mediated degranulation pathway. Skin mast cells can be distinguished from intestinal mast cells through their expression of MRGPRB2, which recognizes substance P (SP) secreted by transient receptor potential vanilloid type 1 (TRPV1+) neurons. Exposure to the house dust mite Dermatophagoides farinae and staphylococcal enterotoxins B (SEB) induces SP secretion, which activates mast cell degranulation through MRGPRB2 [72]. In addition, the activation of skin mast cells and the subsequent release of histamine and serotonin predominantly through the IgE-mediated degranulation pathway causes pruritus. In contrast, IgE-independent pruritis can be caused by the activation of mast cell degranulation by the MRGPRB2 ligand PAMP9-20 which results in tryptase-skewed secretion [75]. Therefore, MRGPRB2-mediated pruritus does not respond well to anti-histamine treatment. Unlike intestinal mast cells, skin mast cells do not express P2RX7 due to the high level of retinoic acid (RA)-degrading enzyme CYP26B1 in the fibroblasts and the RA concentration in the skin under homeostatic conditions [77]. However, the suppression of CYP26B1 activity or supplementation of excessive RA can induce P2RX7 expression by skin mast cells and trigger inflammatory responses to extracellular ATP produced by external stimuli.