Abstract
Objective
Healthy lifestyle habits are the cornerstone in the management of familial hypercholesterolaemia (FH). Nevertheless, dietary studies on FH-affected populations are scarce. The present study analyses dietary habits, adherence to a Mediterranean diet pattern and physical activity in an adult population with FH and compares them with their non-affected relatives.
Design
Cross-sectional study.
Setting
Data came from SAFEHEART, a nationwide study in Spain.
Participants
Individuals (n 3714) aged ≥18 years with a genetic diagnosis of FH (n2736) and their non-affected relatives (n 978). Food consumption was evaluated using a validated FFQ.
Results
Total energy intake was lower in FH patients v. non-affected relatives (P<0·005). Percentage of energy from fats was also lower in the FH population (35 % in men, 36 % in women) v. those non-affected (38 % in both sexes, P<0·005), due to the lower consumption of saturated fats (12·1 % in FH patients, 13·2 % in non-affected, P<0·005). Consumption of sugars was lower in FH patients v. non-affected relatives (P<0·05). Consumption of vegetables, fish and skimmed milk was higher in the FH population (P<0·005). Patients with FH showed greater adherence to a Mediterranean diet pattern v. non-affected relatives (P<0·005). Active smoking was lower and moderate physical activity was higher in people with FH, especially women (P<0·005).
Conclusions
Adult patients with FH report healthier lifestyles than their non-affected family members. They eat a healthier diet, perform more physical activity and smoke less. However, this patient group’s consumption of saturated fats and sugars still exceeds guidelines.
Keywords: Familial hypercholesterolaemia, Diet, Fatty acids, Mediterranean diet, Physical activity
Familial hypercholesterolaemia (FH) is a genetic disorder characterized by high LDL-cholesterol level and a higher risk of premature atherosclerotic CVD( 1 ). FH is caused by mutations in the LDL receptor gene (LDLR) and, less frequently, in the apolipoprotein B gene (APOB). Although FH highly increases cardiovascular risk, atherosclerotic CVD prevalence varies substantially by cohort and country, even across cases with the same genetic mutation( 2 – 4 ). These findings suggest that environmental, metabolic and genetic factors could explain the differences in the CVD burden of these patients( 5 ). In fact, a recent study of the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) identified BMI increase, tobacco consumption and hypertension as predictive risk factors for the development of CVD in FH patients( 6 ).
At the population level, diet is one of the most important environmental factors affecting LDL-cholesterol level as well as other CVD risk factors( 7 – 9 ). Nevertheless, dietary studies on FH-affected populations are scarce. Studies in children with FH in Norway showed that a dietary protocol focused on reducing saturated fat consumption did impact patients’ lipid profiles favourably( 10 , 11 ). Although most patients with FH will require lipid-lowering therapy for life( 12 – 14 ), main clinical guidelines also include a series of dietary and nutritional recommendations as part of treatment( 12 , 15 , 16 ).
The main objective of the present study was to describe the lifestyle habits, especially diet-related, the degree of adherence to a Mediterranean-type diet and the relationship with CVD among individuals aged ≥18 years with FH and their relatives registered at the SAFEHEART cohort( 17 ).
Methods
Study design and participants
Data came from the SAFEHEART study, the design and methodology of which have been previously described( 17 ). Briefly, SAFEHEART is a prospective, multicentre, nationwide study of a cohort of individuals in Spain with molecular diagnosis of FH and their non-FH affected family members. From January 2004 to January 2016, the study enrolled 4217 participants from 829 families. The local ethics committee of the University Hospital Fundación Jiménez Díaz (Madrid) approved the study and all participants signed informed consents.
Exclusion criteria included: individuals under 18 years of age (n 269); failure to complete a semi-quantitative validated FFQ at inclusion (n 230); and reporting either an excessively high (>14 644 kJ/d (>3500 kcal/d) for women and >17 573 kJ/d (>4200 kcal/d) for men) or an excessively low energy intake (<2092 kJ/d (<500 kcal/d) for women and <3347 kJ/d (<800 kcal/d) for men) to eliminate outliers( 18 ) (n 4). Thus, herein we analysed the data from the remaining 3714 individuals.
Upon entering the study, participants completed a 113-item FFQ, previously validated for this population( 19 ). The FFQ included questions about the consumption of each food during the previous year, specifying the size of the typical portion and consumption frequency (never before or number of times per year, per month, per week or per day). Based on the FFQ data, adherence to the Mediterranean diet (MD) was evaluated with the MEDAS( 20 ) questionnaire, an instrument validated and developed to assess the degree of adherence to a traditional MD pattern in the general population( 21 ).
Study variables
A clinical history and ad hoc questionnaires collected participant demographic and clinical characteristics including age, history of CVD, common CVD risk factors (type 2 diabetes, hypertension, smoking) and level of physical activity. A physical examination included standardized measurement of weight (kg) and height (cm), BMI (kg/m2) and waist circumference (cm). Blood pressure was measured twice in the supine position using an Omron MX3 sphygmomanometer.
Energy and nutrient intakes were estimated using the Spanish official food composition tables( 22 ). Two indices were used to assess fat quality: (i) the energy contribution of the different types of fatty acids according to their degree of saturation, i.e. SFA, MUFA and PUFA; and (ii) the relationship among them, i.e. PUFA:SFA and (PUFA+MUFA):SFA.
Adherence to the MD was evaluated with the fourteen-item MEDAS( 20 ), comprising two items on eating habits, eight items on the consumption frequency of traditional MD foods and four items to assess low consumption levels of non-recommended foods. Each item is scored 0 or 1 for a total score ranging from 0 to 14. A higher score indicates greater adherence to a MD. We defined( 23 ) high adherence as a score ≥9 and moderate adherence as a score ≥7. The MEDAS score was calculated from the FFQ data. However, since the FFQ does not specify the amount of olive oil used just for sofrito (a sauce consisting of tomato, onion and garlic, slow-cooked with olive oil), we cannot know whether participants met or did not meet the fourteenth MEDAS objective of sofrito consumption ≥2/week. Therefore this item was excluded, and the total score was based on a maximum of 13 points. Physical activity was measured with the reduced version of the International Physical Activity Questionnaire (IPAQ)( 24 ).
Statistical analysis
We performed descriptive analyses with the objective of describing the dietary habits of the SAFEHEART cohort and comparing the regular diet of participants with and without FH. Variables were analysed separately by sex. Qualitative variables are described by number of cases and corresponding percentages; normally distributed quantitative variables are described by their means and sd; and non-normally distributed quantitative variables are described with the median and interquartile range. The χ 2 test, Student’s t test for independent data and the Mann–Whitney U test for independent data were used to compare differences across qualitative, normally distributed quantitative and non-normally distributed quantitative data, respectively. Statistical significance was set at two-sided P<0·05.
Results
Description of the sample
Participant characteristics are shown in Table 1. Of the 3714 individuals, 2736 (73·6 %) had molecular confirmation of FH and 978 were non-affected family members (negative genetic study; control group). Over half (54 %) were women and the mean age was 45·1 (sd 15·6) years. The majority of patients were on lipid-lowering treatment at study entry. Mean BMI was 26·9 (sd 4·1) kg/m2 in men and 25·8 (sd 5·3) kg/m2 in women (P<0·005). Over one-third of the entire sample (36·7 %) was overweight and 20·2 % were obese. We did not find differences in BMI and prevalence of overweight or obesity between participants with and without FH. Prevalence of hypertension and type 2 diabetes was 14·7 and 4·0 %, respectively, without differences by FH status. More men than women were current smokers (32·1 and 24·8 %, respectively; P<0·005) and more controls than FH patients smoked (33·8 and 26·3 %, respectively; P<0·005). Patients with FH and a history of CVD reported the lowest rate of tobacco consumption (12·9 %).
Table 1.
Baseline characteristics of adults in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by sex and diagnosis of familial hypercholesterolaemia (FH)
| Men (n 1708; 46 %) | Women (n 2006; 54 %) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| FH (+) | FH (−) | FH (+) | FH (−) | ||||||
| n, mean or median | %, sd or IQR | n, mean or median | %, sd or IQR | n, mean or median | %, sd or IQR | n, mean or median | %, sd or IQR | P † (men v. women) | |
| n | 1253 | 33·7 | 455 | 12·3 | 1483 | 39·9 | 523 | 14·1 | <0·005 |
| Age (years) | 44·8 | 15·0 | 41·9** | 15·2 | 46·9 | 15·9 | 43·5** | 16·1 | <0·005 |
| BMI (kg/m2) | 26·6 | 4·4 | 27·0 | 4·1 | 25·5 | 5·3 | 25·9 | 5·3 | <0·005 |
| Waist circumference (cm) | 93·1 | 12·2 | 92·0 | 13·4 | 81·9 | 13·8 | 81·1 | 13·9 | <0·005 |
| Systolic aortic pressure (mmHg) | 129·4 | 17·0 | 129·8 | 17·6 | 125·7 | 21·6 | 123·1* | 19·3 | <0·005 |
| Diastolic aortic pressure (mmHg) | 76·8 | 10·5 | 77·9 | 11·1 | 75·5 | 10·9 | 76·1 | 11·0 | <0·005 |
| Total cholesterol (mg/dl) | 245·0 | 66·9 | 202·9** | 41·4 | 252·9 | 65·3 | 211·4** | 44·2 | <0·005 |
| TAG (mg/dl) | 91 | 69–127 | 92 | 69–130 | 77 | 60–107 | 84* | 61–117 | <0·005 |
| HDL-cholesterol (mg/dl) | 45·1 | 11·0 | 49·3** | 11·0 | 54·1 | 12·7 | 59·1** | 13·7 | <0·005 |
| LDL-cholesterol (mg/dl) | 178·1 | 62·4 | 131·4** | 36·8 | 180·7 | 61·0 | 132·9** | 38·1 | 0·19 |
| Serum glucose (mg/dl) | 88·2 | 15·7 | 90·6* | 20·2 | 85·2 | 15·1 | 86·3 | 15·7 | <0·005 |
| Overweight‡ | 562 | 44·8 | 206 | 45·2 | 440 | 29·6 | 155 | 29·6 | <0·005 |
| Obesity§ | 261 | 20·8 | 96 | 21·1 | 285 | 19·2 | 102 | 19·5 | <0·005 |
| High blood pressure | 169 | 13·5 | 68 | 14·9 | 237 | 15·9 | 73 | 14·0 | 0·18 |
| Type 2 diabetes mellitus | 61 | 4·5 | 22 | 4·3 | 55 | 3·5 | 24 | 4·2 | 0·13 |
| Previous atherosclerotic CVD | 244 | 19·4 | 36** | 7·9 | 121 | 8·1 | 11** | 2·1 | <0·005 |
| Family history of early atherosclerotic CVD║ | 416 | 37·1 | 140 | 33·2 | 555 | 41·7 | 164** | 33·2 | <0·05 |
| Active tobacco smoker | 373 | 29·7 | 176** | 38·6 | 345 | 23·2 | 154* | 29·5 | <0·005 |
| Former smoker | 399 | 31·8 | 103** | 22·6 | 277 | 18·6 | 86* | 16·4 | <0·005 |
| Low-intensity physical activity¶ | 229 | 18·2 | 101 | 22·2 | 334 | 22·4 | 156** | 29·8 | <0·005 |
| Moderate-intensity physical activity¶ | 659 | 52·5 | 223 | 49·0 | 963 | 64·7 | 290** | 55·4 | <0·005 |
| Vigorous-intensity physical activity¶ | 365 | 29·1 | 131 | 28·7 | 190 | 12·7 | 77** | 14·7 | <0·005 |
Values are mean and sd, median and interquartile range (IQR), or n and %.
Significant difference by diagnosis of FH: *P<0·05, **P<0·005.
Statistical significance set at P<0·05.
Defined as BMI=25·0–29·9 kg/m2.
Defined BMI≥30·0 kg/m2.
Family history of atherosclerotic CVD before age 60 years.
Measured with the reduced version of the International Physical Activity Questionnaire (IPAQ)( 24 ).
A history of CVD was reported by 19·4 % of men with FH and 7·9 % without FH (P<0·005). Similarly, 8·1 and 2·1 % of women with and without FH had a history of CVD, respectively (P<0·005).
Physical activity
More women (62·3 %) reported moderate physical activity compared with men (51·6 %; P<0·005); further, women with FH were more likely to report moderate physical activity than those in the control group (P<0·005). Within the FH group, a higher proportion of patients who had already suffered CVD reported performing moderate physical activity than those with no CVD history (64·4 v. 58·4 %, respectively; P<0·05; data not shown).
Consumption of energy and nutrients
Table 2 shows the average consumption of macro- and micronutrients by sex and FH diagnosis. The mean daily energy intake was 8401 (sd 1966) kJ (2008 (sd 470) kcal), being higher in men and in non-FH individuals (P<0·005). Carbohydrates accounted for 43·0 % of energy, fats for 37·0 % and proteins for 18·1 %.
Table 2.
Baseline nutrient intake of adults in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by sex and diagnosis of familial hypercholesterolaemia (FH)
| Men (n 1708; 46 %) | Women (n 2006; 54 %) | P ‡ (men v. women) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| FH (+) | FH (–) | FH (+) | FH (–) | ||||||
| Nutrient† | Mean or median | sd or IQR | Mean or median | sd or IQR | Mean or median | sd or IQR | Mean or median | sd or IQR | |
| Energy (kJ/d) | 8573·4 | 1994·9 | 9127·8** | 2103·3 | 8127·0 | 1863·1 | 8522·4** | 1928·4 | <0·005 |
| Energy (kcal/d) | 2049·1 | 476·8 | 2181·6** | 502·7 | 1942·4 | 445·3 | 2036·9** | 460·9 | <0·005 |
| Carbohydrates (E%) | 42·5 | 6·8 | 41·1** | 6·3 | 43·3 | 6·7 | 42·3** | 6·6 | <0·005 |
| Sugars (g/d) | 104·5 | 34·8 | 106·7 | 34·9 | 102·1 | 31·9 | 105·9* | 31·9 | 0·06 |
| Fibre (g/d) | 30·7 | 8·4 | 29·7* | 7·8 | 31·8 | 8·3 | 31·7 | 8·0 | <0·005 |
| Fibre (g/4184 kJ (1000 kcal)) | 15·3 | 3·9 | 13·9** | 3·5 | 17·0 | 4·1 | 15·9** | 4·0 | <0·005 |
| Protein (E%) | 17·6 | 2·7 | 17·2* | 2·7 | 18·8 | 2·8 | 18·2** | 2·8 | <0·005 |
| Animal protein (g/d) | 60·1 | 17·6 | 63·6** | 18·1 | 61·3 | 17·7 | 63·7* | 18·9 | 0·14 |
| Vegetable protein (g/d) | 29·0 | 8·4 | 29·1 | 8·4 | 27·9 | 8·2 | 28·5 | 8·1 | <0·005 |
| Fat (E%) | 35·7 | 6·4 | 38·0** | 5·8 | 36·1 | 6·3 | 38·0** | 6·4 | 0·25 |
| Cholesterol (mg/d) | 224·3 | 76·9 | 262·8** | 85·8 | 207·9 | 70·0 | 237·2** | 84·9 | <0·005 |
| MUFA (E%) | 20·3 | 3·9 | 20·7 | 3·5 | 20·9 | 4·1 | 21·2 | 3·8 | <0·005 |
| PUFA (E%) | 8·0 | 1·4 | 8·0 | 1·4 | 8·3 | 1·4 | 8·2 | 1·7 | <0·005 |
| SFA (E%) | 12·1 | 2·2 | 13·3** | 2·3 | 12·1 | 2·1 | 13·1** | 2·2 | 0·30 |
| Trans-fatty acids (g/d) | 0·8 | 0·6 | 1·2** | 0·7 | 0·7 | 0·5 | 0·9** | 0·7 | <0·005 |
| Trans-fatty acids (E%) | 0·36 | 0·2 | 0·47** | 0·2 | 0·30 | 0·2 | 0·39** | 0·2 | <0·005 |
| MUFA:SFA (E%) | 1·70 | 0·3 | 1·57** | 0·2 | 1·70 | 0·3 | 1·64** | 0·3 | <0·005 |
| PUFA:SFA (E%) | 0·67 | 0·1 | 0·61** | 0·1 | 0·70 | 0·1 | 0·64** | 0·1 | <0·005 |
| (MUFA+PUFA):SFA (E%) | 2·38 | 0·4 | 2·19** | 0·4 | 2·42 | 0·4 | 2·29** | 0·4 | <0·005 |
| n-3 Fatty acids (g/d) | 1·64 | 0·1 | 1·62 | 0·6 | 1·60 | 0·6 | 1·58 | 0·5 | 0·20 |
| Alcohol (E%) | 3·0 | 0·8–5·8 | 2·0 | 0·8–5·0 | 0·5 | 0·0–2·0 | 0·5 | 0·0–2·0 | <0·005 |
| K (mg/d) | 3602·1 | 994·2 | 3572·6 | 975·9 | 3713·9 | 966·5 | 3762·2 | 991·2 | <0·005 |
| Na§ (mg/d) | 1978·9 | 703·0 | 2087·0** | 710·0 | 1872·2 | 701·4 | 1980·5** | 737·6 | <0·005 |
E%, percentage of energy.
Values are mean and sd, or median and interquartile range (IQR).
Energy intakes exceeding Willett’s limits have been excluded( 18 ).
Significant difference by diagnosis of FH: *P<0·05, **P<0·005.
The dietary evaluation was carried out using a validated FFQ (113-item).
Statistical significance set at P<0·05.
Na from food excluding salt.
In both sexes, the percentage of energy derived from complex carbohydrates and proteins was higher in patients with FH than the control group (P<0·005), whereas the percentage of energy derived from fats was higher in the control group (P<0·005). Table 3 shows the average consumption of macronutrients and fatty acids by CVD history and FH diagnosis. In both the FH group and the non-FH affected group, the percentage of energy from fats was higher in individuals without a history of CVD (P<0·005); the consumption of SFA followed a similar pattern (P<0·005).
Table 3.
Baseline nutrient intake of adults in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by previous atherosclerotic CVD (ASCVD) and diagnosis of familial hypercholesterolaemia (FH)
| Patients with FH (n 2736) | Non-affected relatives (n 978) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| With ASCVD (n 365) | Without ASCVD (n 2371) | With ASCVD (n 47) | Without ASCVD (n 931) | |||||||
| Nutrient† | Mean | sd | Mean | sd | P ‡ | Mean | sd | Mean | sd | P ‡ |
| Energy (kJ/d) | 8040·8 | 1876·5 | 8289·8 | 1930·1 | <0·05 | 8584·3 | 1862·7 | 8815·3 | 2041·8 | 0·45 |
| Energy (kcal/d) | 1921·8 | 448·5 | 1981·3 | 461·3 | <0·05 | 2051·7 | 445·2 | 2106·9 | 488·0 | 0·45 |
| Carbohydrates (E%) | 43·9 | 6·9 | 42·9 | 6·8 | <0·05 | 43·7 | 8·1 | 41·7 | 6·5 | <0·05 |
| Sugars (g/d) | 103·8 | 36·6 | 103·1 | 32·8 | 0·70 | 104·3 | 38·0 | 106·4 | 33·0 | 0·67 |
| Fibre (g/4184 kJ (1000 kcal)) | 17·7 | 4·5 | 16·0 | 4·1 | <0·005 | 17·1 | 4·3 | 14·9 | 3·9 | <0·005 |
| Protein (E%) | 18·1 | 3·0 | 18·3 | 2·9 | 0·23 | 18·4 | 3·2 | 17·7 | 2·8 | 0·15 |
| Fat (E%) | 34·4 | 6·6 | 36·2 | 6·3 | <0·005 | 34·7 | 6·8 | 38·2 | 6·0 | <0·005 |
| Cholesterol (mg/d) | 196·3 | 68·4 | 218·4 | 74·1 | <0·005 | 225·0 | 81·7 | 250·4 | 86·4 | <0·05 |
| MUFA (E%) | 20·3 | 4·3 | 20·7 | 4·0 | 0·08 | 19·4 | 4·0 | 21·1 | 3·7 | <0·005 |
| PUFA (E%) | 8·1 | 1·6 | 8·2 | 1·4 | <0·05 | 7·7 | 1·6 | 8·2 | 1·6 | <0·05 |
| SFA (E%) | 11·4 | 2·2 | 12·3 | 2·2 | <0·005 | 12·0 | 3·0 | 13·3 | 2·2 | <0·005 |
| Trans-fatty acids (g/d) | 0·6 | 0·6 | 0·8 | 0·6 | <0·005 | 0·8 | 0·8 | 1·1 | 0·8 | <0·05 |
| Trans-fatty acids (E%) | 0·30 | 0·2 | 0·30 | 0·2 | <0·005 | 0·34 | 0·3 | 0·44 | 0·3 | <0·05 |
| MUFA:SFA (E%) | 1·80 | 0·3 | 1·70 | 0·3 | <0·005 | 1·70 | 0·4 | 1·60 | 0·3 | 0·16 |
| PUFA:SFA (E%) | 0·70 | 0·2 | 0·70 | 0·1 | <0·005 | 0·67 | 0·2 | 0·63 | 0·1 | 0·07 |
| (MUFA+PUFA):SFA (E%) | 2·50 | 0·4 | 2·40 | 0·4 | <0·005 | 2·34 | 0·5 | 2·24 | 0·4 | 0·08 |
| n-3 Fatty acids (g/d) | 1·70 | 0·7 | 1·60 | 0·6 | 0·32 | 1·80 | 0·8 | 1·60 | 0·6 | <0·05 |
Values are mean and sd.
Energy intakes exceeding Willett’s limits have been excluded( 18 ).
The dietary evaluation was carried out using a validated FFQ (113-item).
Statistical significance set at P<0·05.
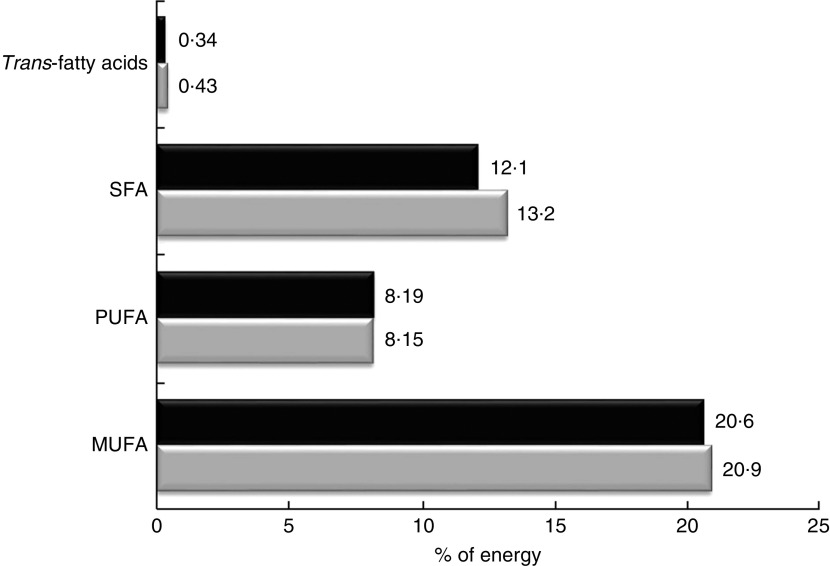
Regarding the quality of the fat consumed (Fig. 1), MUFA represented 20·7 %, SFA 12·4 % and PUFA 8·2 % of energy from fats. The intake of SFA was higher in the control group for both sexes (P<0·005), but no significant differences were detected in the energy derived from MUFA and PUFA between FH patients and controls. The percentage of energy from trans-fatty acids was low (0·3–0·4 %). The relationship between unsaturated and saturated fatty acids (PUFA:SFA and (PUFA+MUFA):SFA) was significantly higher in women (P<0·005) as well as in FH patients (P<0·005). The consumption of cholesterol was higher in non-FH affected participants (P<0·005). None of the groups reported a mean cholesterol intake exceeding 300 mg/d (nutritional objectives for the Spanish population( 25 )). The cohort’s overall consumption of n-3 fatty acids was 1·62 g/d with no substantial differences across groups.
Fig. 1.
Percentage of energy from fatty acids in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by diagnosis of familial hypercholesterolaemia (FH):  , patients aged ≥18 years with a genetic diagnosis of FH (n 2736);
, patients aged ≥18 years with a genetic diagnosis of FH (n 2736);
 , non-affected relatives (n 978)
, non-affected relatives (n 978)
The mean consumption of total fibre was 31·1 (sd 8·3) g/d. When expressing this as an intake per 4184 kJ (1000 kcal), we detected a higher consumption in FH patients across sexes (P<0·005). The consumption of sugars was lower in FH patients compared with their non-affected relatives (P<0·05).
Food consumption
Table 4 shows the average food consumption by sex and FH diagnosis. Cereal consumption was significantly higher in men than women. However, there were no differences between FH patients and controls. Regarding the total consumption of milk products, there were no differences between participants with and without FH. However, more FH patients reported consuming skimmed milk products than non-FH participants (P<0·005).
Table 4.
Baseline food and food group intakes of adults in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by sex and diagnosis of familial hypercholesterolemia (FH)
| Men (n 1708; 46 %) | Women (n 2006; 54 %) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| FH (+) | FH (−) | FH (+) | FH (−) | ||||||
| Food or food group† (g/d) | Median or mean | IQR or sd | Median or mean | IQR or sd | Median or mean | IQR or sd | Median or mean | IQR or sd | P ‡ (men v. women) |
| Cereals | 134 | 102–175 | 133 | 101–172 | 127 | 94–165 | 131 | 97–164 | <0·005 |
| Pastry | 10 | 4–24 | 19** | 7–40 | 9 | 3–22 | 14** | 5–27 | <0·005 |
| Sugar and honey | 5 | 1–10 | 5 | 1·4–10 | 5 | 0·16–10 | 5 | 0·4–10 | <0·005 |
| Milk and dairy products | 330 | 233–474 | 340 | 232–471 | 382 | 264–530 | 380 | 264–539 | <0·005 |
| Skimmed dairy | 125 | 0–253 | 0** | 0–125 | 208 | 35–400 | 102** | 0–253 | <0·005 |
| Dairy products, not skimmed | 71 | 0–218 | 200** | 35–325 | 28 | 0–200 | 142** | 1–325 | <0·005 |
| Cheese | 16 | 7–30 | 20** | 8–40 | 21 | 8–38 | 22 | 8–42 | <0·005 |
| Meat and meat products | 137 | 100–180 | 156** | 114–202 | 125 | 94–163 | 139** | 106–183 | <0·005 |
| Red meat | 41 | 22–60 | 52** | 29–74 | 37 | 18–55 | 38** | 21–58 | <0·005 |
| White meat | 56 | 38–77 | 56 | 40–78 | 57 | 41–78 | 59 | 41–82 | 0·06 |
| Sausages and other meat products | 28 | 15–50 | 37** | 21–60 | 24 | 13–43 | 28** | 15–50 | <0·005 |
| Eggs | 17 | 8–25 | 17** | 17–25 | 17 | 8–24 | 17** | 17–25 | 0·17 |
| Fish and shellfish | 56 | 37–81 | 50** | 35–76 | 61 | 38–92 | 57** | 37–79 | <0·005 |
| White fish | 18 | 18–37 | 18 | 18–37 | 37 | 18–55 | 37* | 18–55 | <0·005 |
| Oily fish | 18 | 18–37 | 18** | 8–37 | 18 | 18–37 | 18** | 8–37 | 0·21 |
| Oils and fats | 27 | 18–35 | 27 | 18–36 | 28 | 21–37 | 29 | 21–38 | <0·005 |
| Olive oil | 23 | 16–31 | 22 | 15–32 | 25 | 17–33 | 25 | 18–35 | <0·005 |
| Butter and margarine | 1·12 | 2·6 | 1·49** | 3·1 | 1·47 | 3·0 | 1·67** | 3·1 | <0·005 |
| Vegetables | 231 | 149–339 | 213** | 130–299 | 285 | 195–385 | 270* | 177–368 | <0·005 |
| Legumes | 14 | 14–28 | 14 | 14–28 | 14 | 14–28 | 14* | 14–28 | 0·16 |
| Potatoes | 43 | 21–64 | 43 | 21–68 | 42 | 21–64 | 42 | 21–64 | <0·05 |
| Fruits | 250 | 138–402 | 220 | 123–359 | 296 | 179–457 | 297 | 167–443 | <0·005 |
| Nuts | 5 | 1·6–14 | 5 | 1–14 | 3 | 0·5–10 | 3 | 0·8–10 | <0·005 |
| Ready-to-eat-meals | 8 | 2–22 | 12** | 4–32 | 5 | 0·5–16 | 6* | 1–17 | <0·05 |
| Coffee | 50 | 16–100 | 50* | 7–100 | 50 | 21–100 | 50 | 14–100 | 0·11 |
| Sugary drinks | 57 | 13–163 | 70** | 13–200 | 28 | 2–86 | 35** | 6–142 | <0·005 |
| Beer and wine | 107 | 31–250 | 107 | 27–250 | 18 | 0–100 | 18 | 0–78 | <0·005 |
| Distilled beverages | 1·6 | 0–7 | 2* | 0–7 | 0 | 0–0·8 | 0 | 0–1·6 | <0·005 |
Values are median and interquartile range (IQR), or mean and sd.
Energy intakes exceeding Willett’s limits have been excluded( 18 ).
Significant difference by diagnosis of FH: *P<0·05, **P<0·005.
The dietary evaluation was carried out using a validated FFQ (113-item).
Statistical significance set at P<0·05.
Regarding the sources of animal protein, a higher consumption of red meats, sausages and processed meats was observed in the controls of both sexes than their FH-affected counterparts (P<0·005). The average total fish consumption was high (57 g/d) including that of blue fish; patients with FH reported a higher total fish intake than controls (67·1 and 60·4 g/d, respectively; P<0·005).
Regarding vegetables, participants reported an average consumption of 250 g/d, with patients’ intake being higher. In terms of fruit intake, the average amount reported was 272 g/d which is equivalent to about two medium pieces of fruit.
In terms of beverages, we detected a significantly higher consumption of sugary soft drinks in non-FH affected individuals regardless of sex than among FH patients (117·1 and 91·9 g/d, respectively; P<0·005). In the case of alcoholic beverages, both fermented and distilled, consumption was higher in men than in women (P<0·005).
Adherence to the Mediterranean diet
Based on the MEDAS( 20 ) questionnaire, we observed that over 90 % of the individuals met the MD recommendation regarding the use of olive oil as the main culinary fat, as well as for a low consumption of animal fat. In addition, over half of the sample consumed more than 3 servings fish/week and consumed sugary soft drinks <1 time/d. However, fewer than 30 % of the participants reported the minimum daily recommended intake of vegetables and fruits.
The mean MEDAS score (out of 13 points) of the entire cohort was 6·14 points (95 % CI 6·1, 6·2), with higher means achieved by FH patients regardless of sex than controls (P<0·005). However, only 10·1 % of the total sample reported a high adherence to the MD pattern (score ≥9 points) and 31·8 % reported a moderate adherence (score ≥7 points), with women and FH patients scoring higher than their counterparts (Table 5).
Table 5.
Score of Mediterranean Diet Adherence Screener (MEDAS)( 23 ) and degree of adherence to the Mediterranean diet of adults in the SAFEHEART study (Spanish Familial Hypercholesterolemia Cohort Study) by sex and diagnosis of familial hypercholesterolemia (FH)
| Men (n 1708; 46 %) | Women (n 2006; 54 %) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| FH (+) | FH (−) | FH (+) | FH (−) | ||||||
| MEDAS score† | Mean or n | sd or % | Mean or n | sd or % | Mean or n | sd or % | Mean or n | sd or % | P ‡ (men v. women) |
| MEDAS score | 6·1 | 1·8 | 5·3** | 1·8 | 6·4 | 1·7 | 5·9** | 1·8 | <0·005 |
| MEDAS score excluding wine | 5·8 | 1·7 | 5·1** | 1·7 | 6·3 | 1·7 | 5·9** | 1·7 | <0·005 |
| MEDAS score ≥7 | 399 | 31·8 | 94** | 20·6 | 530 | 35·7 | 160** | 30·5 | <0·005 |
| MEDAS score ≥9 | 128 | 10·2 | 27** | 5·9 | 186 | 12·5 | 37** | 7·0 | <0·005 |
Values are mean and sd, or n and %.
Significant difference by diagnosis of FH: **P<0·005.
Score range: 0–13. MEDAS 14th objective was excluded (sofrito consumption ≥2/week)
Statistical significance set at P<0·05.
Given the lack of consensus regarding alcoholic beverages being recommended for cardiovascular prevention, the total score was recalculated after eliminating item 8 (wine consumption of ≥7 glasses/week). The new average score (now out of 12 points) was still significantly higher for FH patients than controls for both sexes.
Discussion
The present study shows that adults with FH have healthier dietary habits and a greater adherence to the MD compared with their non-FH relatives. They also smoke less, especially those individuals with history of CVD, and are more likely to be physically active. To the best of our knowledge, the present study is the first that analyses the nutritional characteristics, MD adherence and other lifestyles in a large population of adults with FH.
The relationships between diet, CVD and death are topics of major public health importance, and subjects of great controversy. In European and North American countries, the most enduring and consistent dietary advice is to restrict SFA, by replacing animal fats with vegetable oils( 26 ). It has been shown in the PREDIMED study that a MD supplemented with extra-virgin olive oil or nuts is associated with a reduction in the incidence of cardiovascular events and death in a high-risk primary prevention population in Spain, explained in part by the intake of MUFA and PUFA( 7 ). One of the inclusion criteria in the PREDIMED study was an LDL-cholesterol level >160 mg/dl and therefore it is possible that some few cases of FH were included in the study; however, there are no specific results available regarding this population.
A key index of diet quality is the energy profile that was more balanced in patients with FH than in their non-FH relatives. Energy intake and BMI were significantly lower in FH patients. In addition, the prevalence of overweight and obesity in this population was slightly lower than in the Spanish general population (39·3 % of overweight and 21·6 % of obesity)( 27 ).
Patients reported a lower energy intake from total and saturated fat due to a lower intake of whole milk, red meat, sausages and precooked foods. In the current study, fats accounted for 37 % of energy. The PURE study reported that total fat intake in quintile 5 (33·3–38·3 % of energy) was associated with a lower risk of total mortality and there was no association with CVD( 9 ). Initial PURE study findings challenge conventional diet–disease tenets that are largely based on observational associations in European and North American populations, adding to the uncertainty about what constitutes a healthy diet( 9 ).
It is well known that the quality of fat consumed affects the plasma lipid profile( 28 ) and other cardiovascular risk factors; thus, it is important to know the fatty acid distribution in this specific population with high cardiovascular risk. In the SAFEHEART cohort, the quality of fat reported reaches the recommended MUFA intake (≥20 % of energy) and in parameters like (PUFA+MUFA):SFA≥2 and PUFA:SFA≥0·5( 25 ). This is in part due to the high intake of olive oil, the main source of fat in the Mediterranean diet, and of n-3 fatty acids. The n-3 intake in this population was 1·62 g/d, explained by a higher consumption of fish compared with the Spanish general population( 29 ).
Unfortunately, SFA intake was over 10 % of energy in patients with FH and in their relatives, even in those cases with CVD. This excess consumption of SFA is similar to that observed in the Spanish general population( 29 , 30 ). On the other hand, cholesterol consumption in both FH and controls was below 300 mg/d, meeting the dietary recommendations( 25 ), in contrast to findings from the general population( 30 ).
Regarding carbohydrate intake, the PURE study showed that an intake over 60 % of energy was associated with an adverse impact on total and non-CVD mortality. In the SAFEHEART cohort, carbohydrates represented 43 % of total energy, a lower consumption compared with the 52·4 % reported in the PURE study for Europe and North America( 9 ). Patients with FH reported a lower consumption of carbohydrates than non-FH relatives and similar to that found in the Spanish general population( 29 ). This is mainly explained by fewer consumption of pastries and sugary soft drinks while eating vegetables, fruits and legumes in amounts close to dietary guidelines.
Overall, FH patients had a healthier dietary pattern than their non-FH relatives in terms of consumption of vegetables, fish, skimmed milk products, red meats, sausages and/or processed meats, butter and margarine. Patients with FH are more aware of cardiovascular risk and, therefore, more receptive to dietary and lifestyle advice. This is likely to be especially true regarding fat and cholesterol intake, lower energy consumption and greater energy expenditure. Further, based on our data, women seemed more likely to heed recommendations regarding physical activity.
A great advantage of using a validated adherence index to a dietary pattern is that it allows to evaluate the quality of the overall diet more than does each individual nutrient and/or food item. Among the many MD adherence indices, MEDAS is the only one validated in a high cardiovascular risk population( 20 ). In our cohort, we found a greater adherence to the MD pattern in patients with FH compared with their non-FH relatives. The level of adherence was moderate (6·14 points) and similar to that described for the general population( 31 ), with the difference that the score used in the current analysis was based in thirteen items v. the usual fourteen items used in other studies, making our score slightly better.
There are no other studies like the present one in other FH populations; therefore, we are very limited in terms of placing our work in the context of the existing literature. However, our results confirm previous data observed in a small group of children with FH reporting a healthier diet compared with non-FH children( 32 ). Regarding our control group (non-FH relatives), our results show that they also follow a healthier diet than the Spanish general population( 29 , 30 ). One may speculate that having a relative with a genetic disorder that severely increases cardiovascular risk has a positive impact on one’s own dietary choices. Additionally, having a family history of CVD may increase awareness of cardiovascular risk in the family and diet-related risk factors for CVD. Although our population has a higher cardiovascular risk and most of them are under lipid-lowering therapy, the addition of a MD may improve or attenuate other classical CVD risk factors and biomarkers that increase cardiovascular risk( 7 – 9 , 28 , 33 ).
Our results should be interpreted within the context of the study’s limitations. First, based on the cross-sectional nature of the study, we are unable to draw any conclusions regarding whether following a better diet would have a positive impact on the CVD burden of FH patients. Second, even validated questionnaires rely on self-reported data, which may be subject to recall error and social desirability bias. The present study also has several strengths. First, it is the largest population-based study of individuals with a molecular diagnosis of FH assessing nutritional intake with a comprehensive and validated dietary questionnaire. Second, individuals included in the SAFEHEART study are representative of FH patients residing in a Southern European Mediterranean country, a population that is severely understudied. Since the sample comes from the entire Spanish territory, the sample design reduces the selection bias. Third, individuals of the control group were part of the same families of patients with FH, so it can be argued that detecting significant differences would be harder given the proximity and raised awareness of CVD risk factors among these relatives. Thus, our comparison results could be considered conservative and we would expect larger differences if our FH population were to be compared with the general Spanish population.
Conclusions
Adult patients with FH report better lifestyles, mainly a healthier diet in general and a greater adherence to the MD in particular, than their non-FH relatives. As one would hope, patients with FH and a history of CVD report a lower consumption of total fat and SFA, follow dietary recommendations best, and are the least likely to smoke.
Specifically, FH patients stand out for their high consumption of vegetables, olive oil, fish and skimmed milk products, and their low consumption of pastries, sugary sodas and red meats. This dietary pattern translates into a lower consumption of saturated fats and cholesterol. Yet, this patient group’s consumption of saturated fats and sugars still exceeds general recommendations, which shows room for improvement and an opportunity for targeted intervention in future longitudinal studies in our cohort. Despite the high cardiovascular risk associated with FH and the availability of lipid-lowering therapy, a healthy diet and a better distribution of fat intake could be important allies in controlling CVD-related risk factors.
Acknowledgements
Acknowledgements: The authors thank Teresa Pariente for her hard work in managing the familial cascade screening from the beginning of the SAFEHEART study; all the Spanish Familial Hypercholesterolemia Foundation team for assistance in the recruitment and follow-up of participants; and the FH families for their valuable contribution and willingness to participate. Financial support: This work was supported by Fundación Hipercolesterolemia Familiar; the Instituto de Salud Carlos III (ISCIII; grant numbers G03/181 and FIS PI12/01289); and Centro Nacional de Investigación Cardiovascular (CNIC; grant number 08-2008). None of the funding sources played any role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: R.A.-O. and P.M. designed and conducted the research. R.A.-O., P.M., R.A. and N.M. participated in database design and data input. R.A.-O., P.M. and G.Q.-N. analysed the data. R.A.-O., P.M., R.A., N.M., F.F.-J., O.M.-G., J.L.D.-D., D.Z., F.A. and J.A.G.-S. participated in recruitment of patients. R.A.-O., P.M. and J.R.B. wrote the paper. R.A.-O. and P.M. had primary responsibility for final content. P.M. conceived, design and supervised the SAFEHEART study. All authors read and approved the final manuscript. Ethics of human subject participation: This study complies with the Declaration of Helsinki on ethical principles for medical research involving human subjects and was approved by the local ethic committee (number 01/09) of the University Hospital Fundación Jiménez Díaz (Madrid), acting as the sole committee for the study. Written informed consent was obtained from all participants before their inclusion in the study. All data and blood samples were obtained prior to informed consent. Samples were anonymized for further analysis. If the patient was not willing to take part in the study, this did not cause any prejudice as to future treatment or care.
References
- 1. Goldstein JL, Hobbs HH & Brown MS (2001) Familial hypercholesterolemia. In The Metabolic and Molecular Basis of Inherited Disease, vol. II, pp. 2863–2913 [CR Scriver, AL Beaudet, WS Sly et al., editors]. New York: McGraw-Hill. [Google Scholar]
- 2. Alonso R, Mata N, Castillo S et al. (2008) Cardiovascular disease in familial hypercholesterolaemia: influence of low-density lipoprotein receptor mutation type and classic risk factors. Atherosclerosis 200, 315–321. [DOI] [PubMed] [Google Scholar]
- 3. Pimstone SN, Sun XM, du Souich C et al. (1998) Phenotypic variation in heterozygous familial hypercholesterolemia: a comparison of Chinese patients with the same or similar mutations in the LDL receptor gene in China or Canada. Arterioscler Thromb Vasc Biol 18, 309–315. [DOI] [PubMed] [Google Scholar]
- 4. Slimane MN, Lestavel S, Sun X et al. (2001) Fh-Souassi: a founder frameshift mutation in exon 10 of the LDL-receptor gene, associated with a mild phenotype in Tunisian families. Atherosclerosis 154, 557–565. [DOI] [PubMed] [Google Scholar]
- 5. Jansen AC, van Wissen S, Defesche JC et al. (2002) Phenotypic variability in familial hypercholesterolaemia: an update. Curr Opin Lipidol 13, 165–171. [DOI] [PubMed] [Google Scholar]
- 6. Pérez de Isla L, Alonso R, Mata N et al. (2017) Predicting cardiovascular events in familial hypercholesterolemia: the SAFEHEART registry. Circulation 135, 2133–2144. [DOI] [PubMed] [Google Scholar]
- 7. Estruch R, Ros E, Salas-Salvadó J et al. (2018) Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 378, e34. [DOI] [PubMed] [Google Scholar]
- 8. Mente A, de Koning L, Shannon HS et al. (2009) A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169, 659–669. [DOI] [PubMed] [Google Scholar]
- 9. Dehghan M, Mente A, Zhang X et al. (2017) Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 390, 2050–2062. [DOI] [PubMed] [Google Scholar]
- 10. Tonstad S, Leren TP, Sivertsen M et al. (1995) Determinants of lipid levels among children with heterozygous familial hypercholesterolemia in Norway. Arterioscler Thromb Vasc Biol 15, 1009–1014. [DOI] [PubMed] [Google Scholar]
- 11. Torvik K, Narverud I, Ottestad I et al. (2016) Dietary counseling is associated with an improved lipid profile in children with familial hypercholesterolemia. Atherosclerosis 252, 21–27. [DOI] [PubMed] [Google Scholar]
- 12. Mata P, Alonso R, Ruiz A et al. (2015) Diagnóstico y tratamiento de la hipercolesterolemia familiar en España: documento de consenso. Aten Prim 47, 56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mata P, Alonso R & Pérez-Jiménez F (2014) Screening for familial hypercholesterolemia: a model for preventive medicine. Rev Esp Cardiol 67, 685–688 [DOI] [PubMed] [Google Scholar]
- 14. Saltijeral A, Pérez de Isla L, Alonso R et al. (2017) Attainment of LDL cholesterol treatment goals in children and adolescents with familial hypercholesterolemia. The SAFEHEART follow-up registry. Rev Esp Cardiol 70, 444–450. [DOI] [PubMed] [Google Scholar]
- 15. Watts GF, Gidding S, Wierzbicki AS et al. (2014) Integrated guidance on the care of familial hypercholesterolaemia from the International FH Foundation. Int J Cardiol 171, 309–325. [DOI] [PubMed] [Google Scholar]
- 16. Nordestgaard BG, Chapman MJ, Humphries SE et al. (2013) Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J 34, 3478a–3490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mata N, Alonso R, Badimón L et al. (2011) Clinical characteristics and evaluation of LDL-cholesterol treatment of the Spanish Familial Hypercholesterolemia Longitudinal Cohort Study (SAFEHEART). Lipids Health Dis 10, 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Willett W (2012. ) Nutritional Epidemiology , 3rd ed. New York: Oxford University Press. [Google Scholar]
- 19. Vázquez C, Alonso R, Garriga M et al. (2012) Validation of a food frequency questionnaire in Spanish patients with familial hypercholesterolaemia. Nutr Metab Cardiovasc Dis 22, 836–842. [DOI] [PubMed] [Google Scholar]
- 20. Schröder H, Fitó M, Estruch R et al. (2011) A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 141, 1140–1145. [DOI] [PubMed] [Google Scholar]
- 21. Estruch R, Martínez-González MA, Corella D et al. (2006) Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 145, 1–11. [DOI] [PubMed] [Google Scholar]
- 22. Moreiras O, Carbajal A, Cabrera L et al. (2013) Tablas de Composición de Alimentos y Guía de Prácticas. Madrid: Ediciones Pirámide; (Grupo Anaya, SA). [Google Scholar]
- 23. Martínez-González MA, Fernández-Jarne E, Serrano-Martínez M et al. (2004) Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur J Clin Nutr 58, 1550–1552. [DOI] [PubMed] [Google Scholar]
- 24. Rütten A, Ziemainz H, Schena F et al. (2003) Using different physical activity measurements in eight European countries. Results of the European Physical Activity Surveillance System (EUPASS) time series survey. Public Health Nutr 6, 371–376. [DOI] [PubMed] [Google Scholar]
- 25. Serra-Majem L, Aranceta J & SENC Working Group on Nutritional Objectives for the Spanish Population, Spanish Society of Community Nutrition (2001) Nutritional objectives for the Spanish population. Consensus from the Spanish Society of Community Nutrition. Public Health Nutr 4, 1409–1413. [DOI] [PubMed] [Google Scholar]
- 26. Sacks FM, Lichtenstein AH, Wu JHY et al. (2017) Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 136, e1–e23. [DOI] [PubMed] [Google Scholar]
- 27. Aranceta-Bartrina J, Pérez-Rodrigo C, Alberdi-Aresti G et al. (2016) Prevalence of general obesity and abdominal obesity in the Spanish adult population (aged 25–64 years) 2014–2015: the ENPE study. Rev Esp Cardiol 69, 579–587. [DOI] [PubMed] [Google Scholar]
- 28. Mata P, Ordovas JM, Lopez-Miranda J et al. (1994) ApoA-IV phenotype affects diet-induced plasma LDL cholesterol lowering. Arterioscler Thromb 14, 884–891. [DOI] [PubMed] [Google Scholar]
- 29. Ruiz E, Ávila JM, Valero T et al. (2015) Energy intake, profile, and dietary sources in the Spanish population: findings of the ANIBES study. Nutrients 7, 4739–4762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Banegas JR, Graciani A, Guallar-Castillón P et al. (2011) Estudio de Nutrición y Riesgo Cardiovascular en España (ENRICA). Madrid: Departamento de Medicina Preventiva y Salud Pública, Universidad Autónoma de Madrid. [Google Scholar]
- 31. León-Muñoz LM, Guallar-Castillón P, Graciani A et al. (2012) Adherence to the Mediterranean diet pattern has declined in Spanish adults. J Nutr 142, 1843–1850. [DOI] [PubMed] [Google Scholar]
- 32. Molven I, Retterstøl K, Andersen LF et al. (2013) Children and young adults with familial hypercholesterolaemia (FH) have healthier food choices particularly with respect to dietary fat sources compared with non-FH children. J Nutr Sci 2, e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Foscolou A, Georgousopoulou E, Magriplis E et al. (2018) The mediating role of Mediterranean diet on the association between Lp(a) levels and cardiovascular disease risk: a 10-year follow-up of the ATTICA study. Clin Biochem 60, 33–37. [DOI] [PubMed] [Google Scholar]