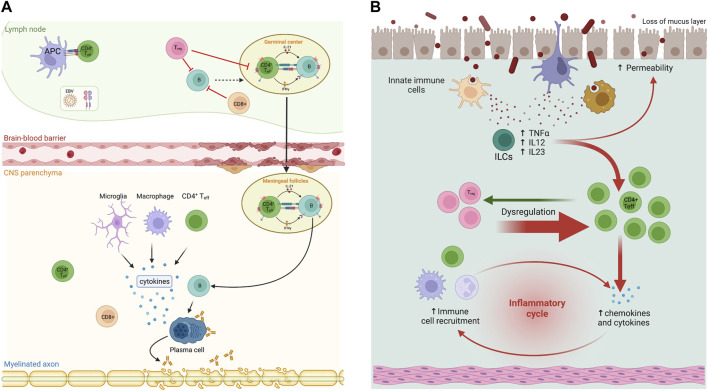
FIGURE 1.
Immunopathogenesis in multiple sclerosis (MS) and inflammatory bowel diseases (IBD). (A) In MS patients, B and T cells interact in the periphery and central nervous system (CNS) to contribute to pathogenesis. In secondary lymphoid organs, EBV-infected B cells escape suppression by CD8+ and T regulatory (Treg) cells. Activated B cells in germinal centres interact with follicular T cells (Th) and differentiate into pathogenic memory B cells. These B cells activate Th effector cells (Th1 and Th17) that in turn infiltrate the CNS through the distinct expression of CXCR3, CCR6, and/or VLA4, as well as pro-inflammatory cytokines. In the CNS, T and B cells reunite in follicle-like structures resulting in clonal expansion. Plasma cells derived from B cell differentiation produce potential harmful antibodies. Cytotoxicity derived from CD8+ cells and clonal antibodies expand inflammation and produce demyelination. (B) Generally, Th17 and Treg cells modulate the proliferation of each other to maintain balance in GI mucosa. Th17 cells that release IL-17 are a strong pro-inflammatory factor, while Treg cells play a critical role in preserving immune homeostasis and establishing inflammation in response to foreign or non-pathogenic antigens such as commensal bacteria. Failure of Treg cell function can lead to IBD. A recently described cell type, innate lymphoid cells (ILCs) also provide host protective immunity in mucosal tissues, although mononuclear phagocytes have an important role in the activation of pathogenic ILCs. Modified and made with Biorender.