Abstract
Ovarian torsion in the third trimester of pregnancy is a rare but potentially dangerous non-obstetric complication for both mother and fetus and presents a diagnostic and therapeutic challenge for the treating physicians. A 39-year-old woman (gravida 2, para 1) presented at 7 weeks of gestation. Asymptomatic bilateral small ovarian cysts were diagnosed at the initial presentation. Progesterone was intramuscularly administered every 2 weeks after 28 weeks of gestation because of uterine cervical length shortening. Sudden onset of right lateral abdominal pain was reported at 33 weeks and 2 days of gestation. Emergency laparoendoscopic single-site (LESS) surgery was performed through the umbilicus under strong suspicion of right adnexal torsion with ovarian cyst, as indicated by magnetic resonance imaging a day after admission. Isolated right ovarian torsion without fallopian tube involvement was identified under laparoscopic view. The contents of the right ovarian cyst were aspirated after confirming resumption of color tone of the right ovary after detorsion. Then, the right adnexal tissue was grasped through the umbilicus, followed by a successful ovarian cystectomy under direct vision. Tocolysis was postoperatively attempted by intravenous ritodorine hydrochloride and magnesium sulfate administration, which was continued through to 36 weeks and 4 days of gestation, because of increased uterine contraction frequency. The next day, spontaneous labor occurred, followed by the vaginal delivery of a healthy 2108-g female infant. The postnatal course was uneventful. Transumbilical LESS-assisted extracorporeal ovarian cystectomy is a feasible and minimally invasive option for ovarian torsion management in the third trimester of pregnancy.
Keywords: Extracorporeal ovarian cystectomy, Laparoendoscopic single-site surgery, Ovarian torsion, The third trimester
Highlights
-
•
Ovarian torsion management in the third trimester of pregnancy is challenging.
-
•
Magnetic resonance imaging is a feasible modality to diagnose ovarian torsion in advanced gestation.
-
•
LESS surgery is a feasible option to manage ovarian torsion in advanced gestation.
1. Introduction
Acute abdominal events during pregnancy present a diagnostic and therapeutic challenge [[1], [2], [3], [4], [5]]. The feasibility and safety of laparoscopic surgery for obstetric and non-obstetric disorders in any trimester of pregnancy are well established [2], but reports on laparoscopic management of adnexal torsion in the third trimester remain limited [[6], [7], [8], [9]].
Gasless laparoendoscopic single-site (LESS) assisted extracorporeal ovarian cystectomy is a procedure in which an ovarian cyst is visualized and extracorporealized through the umbilicus under laparoscopic guidance, followed by cystectomy under direct vision in a similar manner to a laparotomic procedure [10].
Herein, a case is presented of ovarian torsion at 33 weeks of gestation with a favorable pregnancy outcome after successful management by LESS-assisted extracorporeal ovarian cystectomy.
2. Case Presentation
A 39-year-old woman (gravida 2, para 1) presented at 7 weeks of gestation. Her obstetrical history was significant, with previous premature delivery due to cervical incompetency at 36 weeks of gestation. Asymptomatic bilateral ovarian cysts were identified at the initial examination, 23 mm in diameter on the right (Fig. 1A) and 37 and 21 mm in diameter on the left (Fig. 1B), in addition to a viable fetus in the uterine cavity, and observation followed.
Fig. 1.
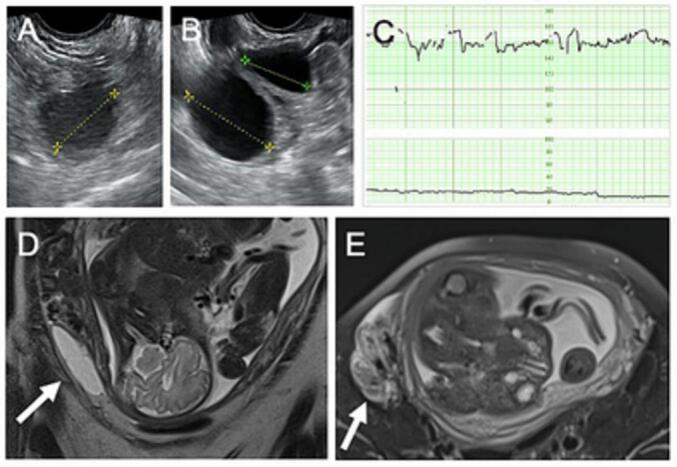
(A) Ultrasonographic findings of the right adnexal cyst, 23 mm in diameter, at 7 weeks of gestation. (B) Ultrasonographic findings of left adnexal cysts, 37 and 21 mm in diameter, at 7 weeks of gestation. (C) A cardiotocogram showing a reassuring fetal heart rate pattern without uterine contraction at initial evaluation. (D) Coronal T2-weighed magnetic resonance image showing a right adnexal cystic mass measuring 69 × 21 mm (arrow) at 33 weeks and 2 days of gestation. (E) Axial T2-weighed magnetic resonance image showing an unusual structure suggesting the presence of a torted pedicle (arrow) at 33 weeks and 2 days of gestation.
The patient was seen for the sudden onset of right lateral abdominal pain and was admitted for observation at 33 weeks and 2 days of gestation. Cardiotocography revealed reassuring fetal heart rate patterns without uterine contraction (Fig. 1C). Ultrasonographic examination did not produce a definitive diagnosis.
The next day, magnetic resonance imaging (MRI) revealed an elongated and compressed cystic structure measuring 69 × 21 mm (Fig. 1D, arrow), probably of right ovarian origin, along with a concomitant unusual structure indicating the presence of a torted pedicle (Fig. 1E, arrow).
Emergency surgery was planned under strong suspicion of torsion of the right adnexal cystic lesion. After she had been presented with the surgical options, the patient opted for LESS surgery through the umbilicus (Fig. 2A, arrowhead) [11] with potential need for laparotomic conversion rather than traditional laparotomy with midline vertical incision (Fig. 2B, arrowhead), considering anticipated limited surgical view due to the enlarged gravid uterus. Furthermore, she was informed of the possible need for elongation of the surgical wound above the navel and concomitant cesarean section if the surgical view to approach the right adnexal mass (Fig. 2A, arrow, and 2B, arrow) could not be secured even in the case of laparotomy.
Fig. 2.
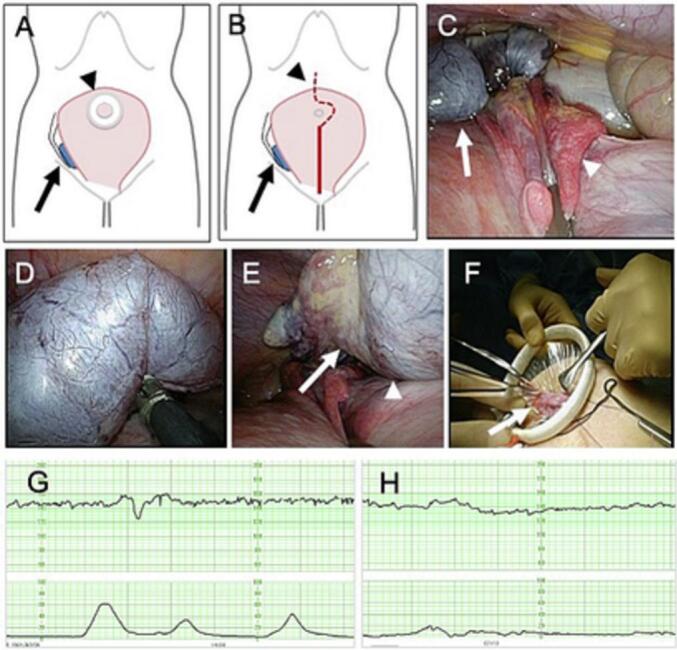
(A) Schematic view showing the relationship between right adnexal mass (arrow) and umbilical working port with Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA) (arrowhead) under the setting of laparoendoscopic single-site surgery. (B) Schematic view showing the relationship between right adnexal mass (arrow) and midline vertical abdominal incision (arrowhead) under the setting of laparotomy. (C) Laparoscopic view showing isolated right ovarian torsion (arrow) without fallopian tube involvement (arrowhead). (D) Laparoscopic view showing untwisting of isolated right ovarian torsion. (E) Laparoscopic view showing resumption of blood flow of right ovary (arrow) after untwisting of isolated right ovarian torsion (arrowhead). (F) Exteriorization of right ovarian cyst (arrow) after cystic content aspiration, followed by extracorporeal cystectomy under direct vision. (G) A cardiotocogram showing a reassuring fetal heart rate pattern with uterine contraction postoperatively. (H) A cardiotocogram showing a reassuring fetal heart rate pattern with decreased uterine contraction after tocolysis by intravenous ritodorine hydrochloride and magnesium sulfate administration.
Identifying the mass lesion was difficult due to the limited working space in the deep right lower abdomen between the enlarged gravid uterus and abdominal wall under laparoscopic view. The operating table was therefore tilted 20° upward to the right to obtain a better right-sided surgical field around the enlarged gravid uterus [7]. Isolated right ovarian torsion (Fig. 2C, arrow) without fallopian tube involvement (Fig. 2C, arrowhead) was identified with gentle compression of the enlarged uterus, followed by successful detorsion of the right ovary (Fig. 2D).
The contents of the right ovarian cyst were aspirated (Fig. 2E, arrowhead) after confirming the resumption of color tone of the right ovary (Fig. 2E, arrow) after detorsion. The right adnexal tissue (Fig. 2F, arrow) was grasped and extracorporealized through the umbilicus, followed by a successful ovarian cystectomy similar to laparotomy. The surgical duration was 38 min, with a minimum estimated amount of intraoperative bleeding. The pathological diagnosis was mucinous cystadenoma.
The frequency of uterine contraction increased postoperatively (Fig. 2G). Tocolysis was attempted by intravenous administration of ritodorine hydrochloride and magnesium sulfate to reduce uterine contraction (Fig. 2H), which was terminated at 36 weeks and 4 days of gestation. Thereafter, spontaneous labor pains began, followed by uneventful vaginal delivery at 36 weeks and 5 days of gestation of a healthy 2108-g female infant, who was admitted to the growing care unit because of low birth weight and preterm delivery. The postnatal course was uneventful except for the occurrence of retained placenta, which was conservatively managed.
3. Discussion
Adnexal masses are more frequently found in pregnant women than in the age-matched general population because of the higher incidence of corpus luteum cyst detection by routine ultrasound workup in early pregnancy [12]. Adnexal masses of 6–8 cm are more prone to torsion than are masses of other sizes [12,13]. Furthermore, pregnancy is one of the potential risk factors for adnexal torsion [14], which is most frequently seen in the first and early second trimesters.
One of the main reasons for the increase in adnexal torsion in early gestation is the presence of a corpus luteum cyst, which tends to torsion, or otherwise spontaneously regresses as the pregnancy progresses into the second trimester [[12], [13], [14]]. Therefore, decisions regarding expectant or surgical management of adnexal masses, especially those discovered in early pregnancy, should be balanced by the risk of torsion, the likelihood of spontaneous resolution, concerns about malignancy, and the risk of surgery [[12], [13], [14]]. Accordingly, careful observation was chosen in the current case, early in gestation, since the bilateral cystic adnexal masses were small and asymptomatic.
A wide range of obstetrical as well as non-obstetrical disorders needs to be included for the differential diagnosis when acute abdominal events occur in pregnant women [[13], [14], [15]]. Ultrasound is a feasible modality for the diagnosis of adnexal mass during pregnancy, especially early in gestation, because of its accuracy, safety, and availability. However, an enlarged uterus may limit its diagnostic capability, especially at advanced gestational ages [14]. Consequently, MRI is currently considered a feasible second-line imaging option when the results from ultrasound are inconclusive or nondiagnostic in pregnant women with acute abdominal symptoms [14].
Representative magnetic resonance images of ovarian torsion are now well documented [14]. These include the heterogeneous appearance of the ovary with or without enlargement, dilatation, and tortuous appearance of the ovarian vascular pedicle, fallopian tube thickening, and uterine deviation toward torsion.
Narrowing the preoperative diagnosis to ovarian torsion was extremely useful when the surgical intervention was decided in the current case, because images to indicate potential twisting of the vascular pedicle with the right adnexal cystic mass were obtained by MRI.
Early operative intervention is desirable even for pregnant women manifesting acute abdominal symptoms, irrespective of gestational age, unless diagnosis by imaging study negates its need [16].
Laparoscopic surgery can be performed in an equally safe manner as an open procedure even during pregnancy [2], although the potential advantages and disadvantages have been debated for many years [17]. The benefits of laparoscopic management over laparotomy during pregnancy include reduced adhesion formation, less postoperative ileus, less postoperative pain, shorter hospital stays, and earlier return to usual daily activities [16].
LESS surgery, in which surgical manipulation is performed through a single incision in the umbilical region, has been introduced to provide further benefits of the laparoscopic approach to adnexal disease in pregnant women [7,11,16,18].
Potential advantages of LESS surgery over conventional multiport laparoscopy include avoiding the risk of injury due to improper penetration of the enlarged uterus during insertion of an insufflation needle or trocar because the working port is created in the umbilicus by an open method under direct observation instead of closed puncture. Additionally, reducing the number of ports can minimize abdominal wall trauma [7,11,16,18].
Conversely, the major disadvantage of LESS surgery is that adjusting the intracorporeal spacing of the surgical instruments is usually difficult due to a lack of triangulation because multiple instruments need to be inserted through the single umbilical port [10]. Thus, elaborate surgeries, such as cystectomy, would be more difficult because of the limited surgical space, although simple laparoscopic procedures, such as salpingectomy, or cyst aspiration and detorsion, could be performed even in women at advanced stages of pregnancy (Table 1) [10].
Table 1.
Summary of previously reported cases of adnexal disorders successfully managed by laparoscopic surgery in the third trimester (n = 9).
| Variables | Results |
|---|---|
| Maternal age (years; median [range]) | 32 (28–39) |
| Parity (number; %) | 8 (100)⁎ |
| Primipara | 3 (37.5) |
| Multipara | 5 (62.5) |
| Estimated gestational age at surgery (weeks; median [range]) | 32 (28–38) |
| Laterality (number; %) | |
| Right | 7 (75) |
| Left | 2 (25) |
| Laparoscopic surgical procedure (number; %) | |
| Salpingectomy | 3 (33.3) |
| Ovarian cyst aspiration after detorsion | 2 (22.2) |
| Ovarian cystectomy after detorsion | 3 (33.3) |
| The drainage of cyst contents and untwisting of the fallopian tube | 1 (11.1) |
| Securing of the surgical view (number; %) | |
| Pneumoperitoneum | 7 (75) |
| Gasless | 2 (25)⁎⁎ |
| Surgical diagnosis (number; %) | |
| Isolated torsion of the fallopian tube | 4 (44.4) |
| Ovarian torsion with ovarian cyst | 4 (44.4) |
| Adnexal torsion with ovarian cyst | 1 (11.1) |
| The estimated gestational age at delivery (weeks; number [%]) | |
| 36 | 1 (11.1) |
| 38 | 3 (33.3) |
| 39 | 3 (33.3) |
| 40 | 1 (11.1) |
| The full term⁎⁎⁎ | 1 (11.1) |
| The mode of delivery (number; %) | |
| Vaginal delivery | 7 (77.8) |
| Vacuum extraction delivery | 1 (11.1) |
| Cesarean section⁎⁎⁎⁎ | 1 (11.1) |
LESS-assisted extracorporeal cystectomy is worth a try, as conversion to multiport laparoscopy or laparotomy remains an option [10]. The chance of success in cystectomy by LESS surgery increases if target tissues can be extracorporealized under laparoscopic guidance, as in the current case.
Carbon dioxide pneumoperitoneum is widely used to achieve an appropriate laparoscopic surgical view when performing laparoscopic management of adnexal masses in pregnant women (Table 1). However, the increased intrabdominal pressure caused by pneumoperitoneum may decrease the venous return to the maternal heart and may disturb the perfusion of uteroplacental circulation even when performed under relatively low insufflation pressure [19]. Furthermore, maternal absorption of carbon dioxide gas could induce fetal acidosis [19].
LESS surgery without pneumoperitoneum is a feasible alternative for the laparoscopic management of adnexal torsion in women of advanced gestational age [7] because gasless laparoscopy can avoid the potential risks associated with carbon dioxide insufflation [19].
Adnexal surgery in advanced gestation can generally result in favorable outcomes for pregnant women and fetuses (Table 1) when managed cooperatively in a facility with appropriate obstetrical, anesthetic, and neonatal support.
4. Conclusion
Transumbilical LESS-assisted extracorporeal ovarian cystectomy is a feasible and minimally invasive option for the management of ovarian torsion in the third trimester of pregnancy.
Acknowledgments
Contributors
Akihiro Takeda contributed to performing the surgery, conception of the case report, acquiring and interpreting the data, drafting the manuscript, undertaking the literature review and revising the article critically for important intellectual content.
Shotaro Hayashi contributed to perinatal care and surgical management of the patient.
Both authors read and approved the final submitted manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient consent
Written informed consent was obtained from the patient for publication of this case report.
Provenance and peer review
This case report was not commissioned and was peer reviewed.
Acknowledgments
Acknowledgments
The manuscript was edited for proper English, grammar, punctuation, spelling, and overall style by native English-speaking editors at Enago (https://www.enago.jp).
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Upadhyay A., Stanten S., Kazantsev G., Horoupian R., A. Stanten Laparoscopic management of a nonobstetric emergency in the third trimester of pregnancy. Surg. Endosc. 2007;21(8):1344–1348. doi: 10.1007/s00464-006-9104-9. [DOI] [PubMed] [Google Scholar]
- 2.Pearl J.P., Price R.R., Tonkin A.E., Richardson W.S., D. Stefanidis SAGES guidelines for the use of laparoscopy during pregnancy. Surg. Endosc. 2017;31(10):3767–3782. doi: 10.1007/s00464-017-5637-3. [DOI] [PubMed] [Google Scholar]
- 3.Guterman S., Mandelbrot L., Keita H., Bretagnol F., Calabrese D., S. Msika Laparoscopy in the second and third trimesters of pregnancy for abdominal surgical emergencies. J. Gynecol. Obstet. Hum. Reprod. 2017;46(5):417–422. doi: 10.1016/j.jogoh.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Weiner E., Mizrachi Y., Keidar R., Kerner R., Golan A., R. Sagiv Laparoscopic surgery performed in advanced pregnancy compared to early pregnancy. Arch. Gynecol. Obstet. 2015;292(5):1063–1068. doi: 10.1007/s00404-015-3744-8. [DOI] [PubMed] [Google Scholar]
- 5.Didar H., Najafiarab H., Keyvanfar A., Hajikhani B., Ghotbi E., S.N. Kazemi Adnexal torsion in pregnancy: a systematic review of case reports and case series. Am. J. Emerg. Med. 2023;65:43–52. doi: 10.1016/j.ajem.2022.12.026. [DOI] [PubMed] [Google Scholar]
- 6.Jo J.Y., Cho I.A., Shin J.K., Lee S.A., W.J. Choi Laparoscopic surgery for fallopian tube torsion due to benign tumour in the third trimester of pregnancy: a case report and literature review. J. Obstet. Gynaecol. 2022;42(7):2566–2572. doi: 10.1080/01443615.2022.2107421. [DOI] [PubMed] [Google Scholar]
- 7.Takeda A., Kitami K., M. Shibata Magnetic resonance imaging and gasless laparoendoscopic single-site surgery for the diagnosis and management of isolated tubal torsion with a paratubal cyst at 31 weeks of gestation: A case report and literature review. J. Obstet. Gynaecol. Res. 2020;46(8):1450–1455. doi: 10.1111/jog.14252. [DOI] [PubMed] [Google Scholar]
- 8.Cohen S.B., Watad H., Shapira M., Goldenberg M., R. Mashiach Urgent laparoscopic surgeries during the third trimester of pregnancy: a case series. J. Minim. Invasive Gynecol. 2020;27(4):909–914. doi: 10.1016/j.jmig.2019.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Duncan R.P., M.M. Shah Laparoscopic salpingectomy for isolated fallopian tube torsion in the third trimester. Case Rep. Obstet. Gynecol. 2012;2012 doi: 10.1155/2012/239352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takeda A., Imoto S., Mori M., Nakano T., H. Nakamura Isobaric laparoendoscopic single-site assisted extracorporeal cystectomy in treatment of selected adnexal tumors: initial experience and technique. J. Minim. Invasive Gynecol. 2010;17(6):766–770. doi: 10.1016/j.jmig.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Takeda A., Imoto S., H. Nakamura Gasless laparoendoscopic single-site surgery for management of adnexal masses during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;180:28–34. doi: 10.1016/j.ejogrb.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Yen C.F., Lin S.L., Murk W., Wang C.J., Lee C.L., Soong Y.K., A. Arici Risk analysis of torsion and malignancy for adnexal masses during pregnancy. Fertil. Steril. 2009;91(5):1895–1902. doi: 10.1016/j.fertnstert.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Cathcart A.M., Nezhat F.R., Emerson J., Pejovic T., Nezhat C.H., C.R. Nezhat Adnexal masses during pregnancy: diagnosis, treatment, and prognosis. Am. J. Obstet. Gynecol. 2022 Nov 19;S0002-9378(22) doi: 10.1016/j.ajog.2022.11.1291. 02179-2. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka Y., Tsuboyama T., Yamamoto K., Terai Y., Ohmichi M., Y. Narumi A case of torsion of a normal ovary in the third trimester of pregnancy: MRI findings with emphasis on asymmetry in the diameter of the ovarian veins. Radiol. Case Rep. 2019;14(3):324–327. doi: 10.1016/j.radcr.2018.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lapides A., Ma W., McKinney C., L. Chuang Laparoscopically treated ovarian torsion in a 32-week pregnancy: a case report. Case Rep. Womens Health. 2023 Mar 15;37 doi: 10.1016/j.crwh.2023.e00496. (e00496) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dursun P., Gülümser C., Cağlar M., Araz C., Zeyneloğlu H., A. Haberal Laparoendoscopic single-site surgery for acute adnexal pathology during pregnancy: preliminary experience. J. Matern. Fetal Neonatal Med. 2013;26(13):1282–1286. doi: 10.3109/14767058.2013.783799. [DOI] [PubMed] [Google Scholar]
- 17.Shigemi D., Aso S., Matsui H., Fushimi K., H. Yasunaga Safety of laparoscopic surgery for benign diseases during pregnancy: a nationwide retrospective cohort study. J. Minim. Invasive Gynecol. 2019 Mar-Apr;26(3):501–506. doi: 10.1016/j.jmig.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Han L., Wan Q., Chen Y., A. Zheng Single-port laparoscopic surgery for adnexal mass removal during pregnancy: the initial experience of a single institute. Front. Med. (Lausanne) 2021;8 doi: 10.3389/fmed.2021.800180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sesti F., Pietropolli A., Sesti F.F., E. Piccione Gasless laparoscopic surgery during pregnancy: evaluation of its role and usefulness. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;170(1):8–12. doi: 10.1016/j.ejogrb.2013.04.012. [DOI] [PubMed] [Google Scholar]


