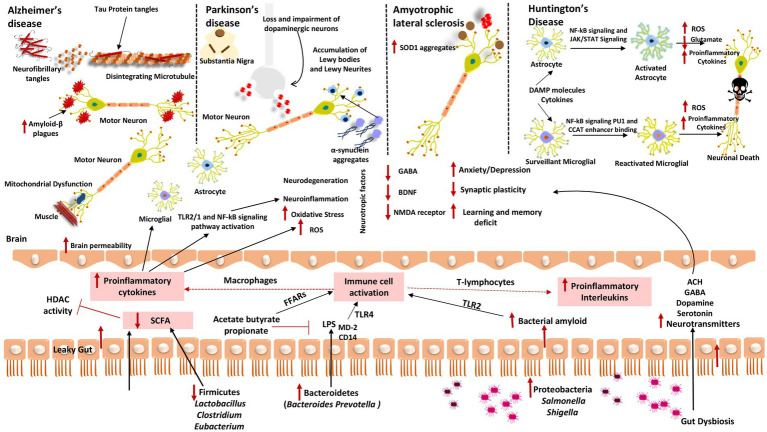
Figure 2.
Gut dysbiosis mechanisms underlying several neurodegenerative diseases (A) Alzheimer’s disease; (B) Parkinson’s disease; (C) Amyotrophic lateral sclerosis; and (D) Huntington’s disease. When fewer healthy microbes are around to create SCFAs like Firmicutes and Actinobacteria, HDAC activity and LPS-induced inflammation cannot be inhibited. Contrarily, gut microorganisms like Bacteroidetes have a high excretion rate of LPS, which stimulates the TLR4 receptor by interacting with CD14 and MD-2 proteins and results in an inflammatory process. Additionally, proteobacteria produce a lot of bacterial amyloids like curli peptide, which binds to TLR2 to activate macrophages and cause them to release pro-inflammatory cytokines like TNF-α, IL-6, and IL-1β. Additionally, T-lymphocyte activation causes Th17 cells to produce pro-inflammatory interleukins like IL-17A and IL-22. These cytokines can cross the BBB, boost ROS production, and encourage oxidative stress, which results in neuroinflammation and neurodegeneration. These cytokines also stimulate the transcription of pro-inflammatory miRNAs, activate neuroinflammatory mediators, and inhibit microglial cell phagocytosis, which promotes the progression of neurodegenerative diseases. These cytokines also initiate TLR2/1 and NF-kB signal transduction pathways in microglia and astrocytes.