Abstract
More than 20 years have elapsed since the September 11, 2001 (9/11) terrorist attacks on the World Trade Center (WTC), Pentagon and at Shanksville, PA. Many persons continue to suffer a variety of physical and mental health conditions following their exposures to a mixture of incompletely characterized toxicants and psychological stressors at the terrorist attack sites. Primary care and specialized clinicians should ask patients who may have been present at any of the 9/11 sites about their 9/11 exposures, especially patients with cancer, respiratory symptoms, chronic rhinosinusitis, gastroesophageal reflux disease, psychiatric symptoms, and substance use disorders. Clinicians, especially those in the NY metropolitan area, should know how to evaluate, diagnose, and treat patients with conditions that could be associated with exposure to the 9/11 attacks and its aftermath. As such, this issue of Archives contains a series of updates to clinical best practices relevant to medical conditions whose treatment is covered by the WTC Health Program. This first paper in the 14-part series describes the purpose of this series, defines the WTC Health Program and its beneficiaries, and explains how relevant Clinical Practice Guidelines were identified. This paper also reminds readers that because physical and mental health conditions are often intertwined, a coordinated approach to care usually works best and referral to health centers affiliated with the WTC Health Program may be necessary, since all such Centers offer multidisciplinary care.
Keywords: 9/11, adults, chemical exposure, chemical mixtures, clinical practice guideline, exposure, occupational diseases, quality, respiratory diseases, September 11, workers, World Trade Center
Introduction
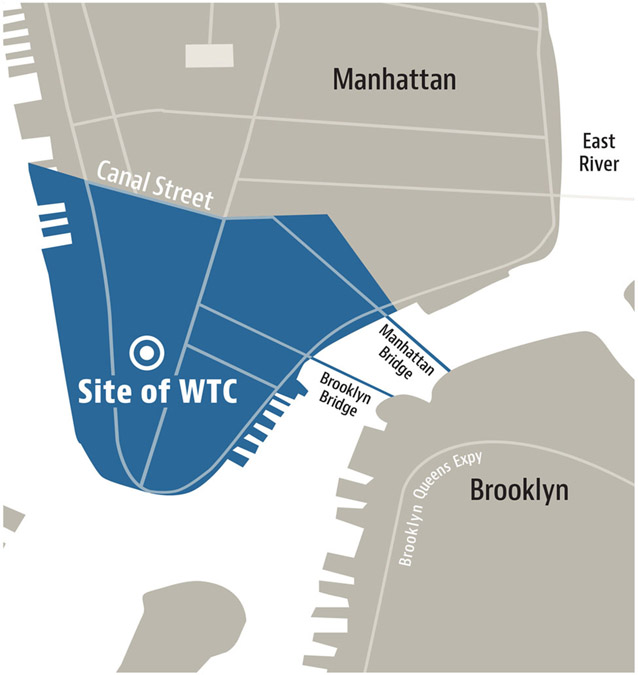
The attacks on September 11, 2001 (9/11) caused almost 3,000 deaths in the immediate aftermath, and potentially adversely affected the health of hundreds of thousands of responders (ie, those involved in the search, rescue, recovery, service restoration and cleanup efforts following the attacks in New York City [NYC][Figure 1], the Pentagon and in Shanksville, PA), and survivors (ie, local building occupants, residents, passersby, workers, and students attending schools in the NYC disaster area [Figure 2]). In NYC, these attacks were estimated to expose nearly a half million people to debris, dust, smoke, and fumes1,2 that have never been completely characterized.3,4 In addition, many individuals who were present at or near the disaster sites were exposed to disturbing and psychologically traumatizing scenes and events. Epidemiologic studies conducted after September 11, 2001, among responders and survivors showed that these persons may be at increased risk for some aerodigestive and other physical and mental health conditions, including post-traumatic stress disorder (PTSD) and major depressive disorder (MDD), and certain types of cancer.5 In the future, additional health conditions may be found to be associated with 9/11 exposures.6 A list of medical conditions covered by the WTC Health Program is available at www.cdc.gov/wtc/conditions.html.
Figure 1.
New York City (NYC) response area used to determine enrollment eligibility for responders to the 9/11 attacks — World Trade Center (WTC) Health Program. Note that the response area also includes WTC-related locations not shown, such as certain barge loading piers and the Staten Island Landfill, and vehicle maintenance areas. Responders are persons who were involved in rescue, response, recovery, clean-up, and related support activities after the September 11, 2001 terrorist attacks.
Source: Azofeifa et al.14
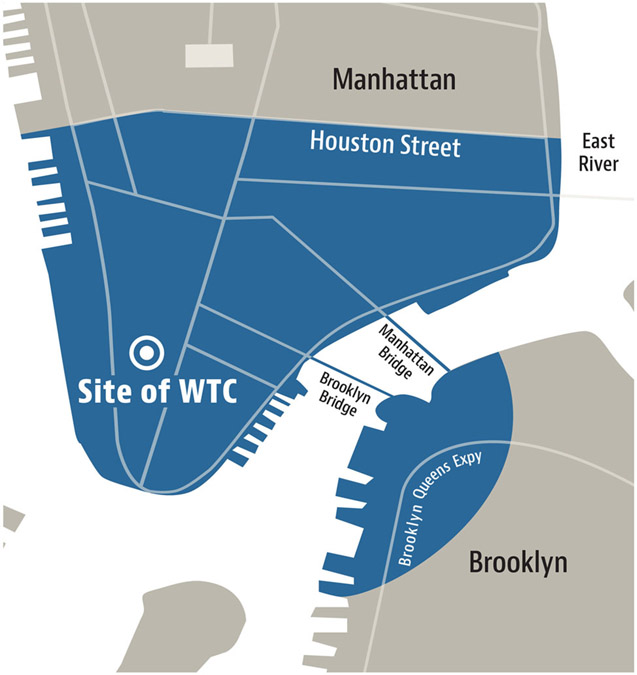
Figure 2.
New York City (NYC) disaster area used to determine enrollment eligibility for survivors of the 9/11 attacks — World Trade Center (WTC) Health Program. The NYC disaster area for the WTC Health Program is defined as the area in Manhattan south of Houston Street and any block in Brooklyn wholly or partially contained within a 1.5-mile radius of the former WTC complex. Survivors are defined as persons who were present in the dust or dust cloud on 9/11 or who worked, lived, or attended school, child care centers, or adult day care centers in the NYC disaster area.
Source: Azofeifa et al.14
Because many persons exposed to the 9/11 terrorist attacks may have health problems caused by—or made worse by—exposure to the attacks and their aftermath, primary care clinicians need to know how to identify, evaluate, treat, and, if necessary, refer these persons for multidisciplinary care. Clinicians should be attuned to patients who may have been present at any of the 9/11 sites, especially patients with cancer, respiratory symptoms, rhinosinusitis, gastroesophageal reflux disease, psychiatric symptoms or illness, and substance use disorders. For these patients, primary care providers should ask about their 9/11 exposures (eg, duration and intensity of dust exposure, psychologically traumatic experiences, and economic and social losses [eg, job and housing loss]). Because many individuals moved from the NYC area after 9/11, it is incumbent upon clinicians across the country to inquire as to whether their patients have had exposure to the 9/11 attacks.
This issue of Archives of Environmental and Occupational Health comprises a series of papers on various WTC-related conditions written by various members of a voluntary Work Group. The Work Group was assembled in April 2021 to update a set of Clinical Guidelines for WTC-related health conditions originally created by the NYC Department of Health and Mental Hygiene (NYC DOHMH) and last revised in 2008.7 The Work Group consisted of clinicians affiliated with the WTC Health Program. They were employed either by WTC Clinical Centers of Excellence (CCEs), the Nationwide Provider Network (NPN), the WTC Health Registry of the NYC DOHMH, or the National Institute for Occupational Safety and Health (NIOSH). The Work Group met fortnightly through September 2022, where each of the papers in this series was discussed and any Work Group member concerns were addressed.
The purpose of this series of papers is to promote the practice of high quality, evidence-based medicine when evaluating, diagnosing and treating persons with WTC-related exposures. The best practices provided in these papers are targeted to adults, including adults who were exposed as children.
9/11 Exposures
The 9/11 terrorist attacks represent an unprecedented large-scale acute and chronic environmental disaster. The burning and collapse of the WTC and neighboring buildings released a complex but incompletely characterized mixture of irritant dust, smoke, and gaseous materials. Pulverized concrete, glass, plastic, paper, and wood produced alkaline dust. The dust cloud also contained heavy metals, asbestos, and other carcinogenic substances. In addition, smoke released from the fires that burned over the next 13 weeks contained hazardous and carcinogenic substances.8 Environmental test results showed that the composition of dust and smoke released into the air and deposited on indoor and outdoor surfaces varied by date and location. Chemical tests suggest that because dust was protected from moisture in indoor environments, it retained its alkalinity to a greater extent than outdoor dust which was exposed to rain.4,9
During the 9/11 attacks and the subsequent months, responders and survivors were also subjected to disturbing psychological stressors. Responders were often exposed to many hours of strenuous work and hazardous working conditions,10 including sometimes handling human remains. As for survivors in southern Manhattan and western Brooklyn (ie, the New York City disaster area [Figure 2]), these persons were often displaced from their homes, jobs and schools, experienced economic hardship and were exposed to frequent reminders of 9/11-related death and destruction.
Individual exposure to contaminants is determined by duration and intensity of exposure, including location, roles and activities performed by the person, cleanup methods, and use of appropriate personal protective equipment. Health effects related to a particular exposure may also vary depending on a person’s underlying medical conditions and individual susceptibility. Unfortunately, there are little individual-level objective data on the exposures experienced after the 9/11 attacks. Instead, exposure data for specific responders and survivors are self-reported, including dates worked and location (eg, worked at Ground Zero [ie, the six-story pile of smoking WTC building rubble that burned intermittently for more than three months], immersed in the dust cloud on 9/11, lived or worked in a heavily dust-contaminated area). Additional information on assessing duration and intensity of 9/11 exposures is available.11 Self-reported exposure data have been successfully used to identify a biological gradient (ie, increased disease frequency with increasing levels of 9/11 exposure, eg, see 12) There is no proven accepted toxicant exposure biomarker that could serve as a surrogate for self-reported exposure.
The World Trade Center Health Program
To address the need to recognize and treat the various illnesses arising from the 9/11 terrorist attacks, medical care for responders and survivors commenced almost immediately and was provided by local public health officials, major medical centers, and community health programs.13 However, during the first decade post 9/11, funding for this medical care was limited and intermittent.14 This changed on January 3, 2011, when President Obama signed into law the James Zadroga 9/11 Health and Compensation Act of 2010, which established the World Trade Center (WTC) Health Program.
The World Trade Center (WTC) Health Program (https://www.cdc.gov/wtc/) is a limited benefits health plan that provides health care at no out-of-pocket cost for certified WTC-related health conditions to over 117,000 responders and survivors located in the New York (NY) metropolitan area and across the country in 434 out of 435 Congressional Districts. For those in the NY metropolitan area, health surveillance and medical care are provided at eight Clinical Centers of Excellence (CCE) locations. The Nationwide Provider Network (NPN) provides care for members who live outside the NY metropolitan area. These CCEs are health centers and the NPN is a third-party administrator under contract with the WTC Health Program. The CCEs and NPN use an integrated and multidisciplinary approach to provide a broad suite of health services. Health care is provided by medical and mental health professionals with training and experience in various specialties, including occupational and environmental medicine, with focused and/or substantial experience in the multidisciplinary evaluation, diagnosis, and treatment of WTC-related health conditions.
Program-associated health care providers
For treatment to be covered by the Program, it must be obtained from a WTC Health Program affiliated provider. Affiliated providers are health care providers who are associated with a CCE or NPN and are authorized to provide Program-covered care.
Each CCE has established a health care provider network to serve all Program members assigned to the CCE. Some affiliated providers work directly for the CCE or the medical institution that hosts the CCE. Other affiliated providers are contracted by the CCE to provide medical and/or mental health services to members of the CCE.
The NPN is a network of affiliated providers that are located all over the United States to serve Program members who reside outside of the NY metropolitan area. Providers interested in learning more about becoming a WTC Health Program affiliated provider can call the WTC Health Program Call Center at 1-888-982-4748.
Contact information for the CCEs and NPN is available at https://www.cdc.gov/wtc/clinics.html.
Eligibility to receive program benefits
The WTC Health Program is authorized by the James Zadroga 9/11 Health and Compensation Act (2010; https://www.govinfo.gov/app/details/PLAW-111publ347/summary%20?) and its Reauthorization (2015; http://uscode.house.gov/view.xhtml?req=granuleid%3AUSC-prelim-title42-chapter6A-subchapter31&edition=prelim) to provide benefits to these categories of individuals:
Responders
Workers or volunteers who provided rescue, recovery, debris cleanup, and related support services on or in the aftermath of the September 11, 2001, attacks for certain amounts of time during the period between September 11, 2001, and July 31, 2002. There are four types of responders: Fire Department of the City of New York (FDNY) Responders; NYC General Responders (including New York City Police Department staff); Pentagon Responders; and Shanksville, PA Responders. Figure 1 provides the geographic boundaries that define Program enrollment eligibility for FDNY and NYC responders (ie, the NYC response area).
WTC Survivors
These persons meet one or more of the following criteria: individuals who were present in the New York City Disaster Area (ie, lower Manhattan below Houston Street and Western Brooklyn) in the dust or dust cloud on September 11, 2001; who worked, resided, or attended school, childcare, or adult daycare in the NYC Disaster Area from September 11, 2001, to July 31, 2002; who were eligible for certain residential grants or whose place of employment was eligible for certain grants following the September 11, 2001, attacks. Figure 2 provides the geographic boundaries that define Program enrollment eligibility for survivors.
As a limited health care benefits program, the WTC Health Program provides the following services to members, which by law vary depending on whether the member is a responder or a survivor:
Enrolled Responders receive:
A comprehensive initial health evaluation performed at a CCE or NPN clinic. During this evaluation, potential WTC-related health conditions are sought and evaluated to determine whether 9/11 exposures were substantially likely to have been a significant factor in aggravating, contributing to, or causing that health condition. If a CCE/NPN-affiliated physician attests that this requirement is met, then the condition is eligible for program certification as a WTC-related health condition (when a condition is certified, its treatment is covered by the WTC Health Program for responders, and for survivors the treatment benefit is coordinated with other health insurance);
Annual comprehensive health monitoring and surveillance examinations performed at a CCE or NPN clinic;
Medical and mental health treatment for certified WTC-related health conditions;
Cancer screening tests (that are rated “Grade A” or “Grade B” by the U.S. Preventive Services Task Force (USPSTF); and
Benefits counseling services.
Screening-Eligible Survivors (ie, an individual who meets the WTC Survivor eligibility criteria and who has symptoms of a WTC-related health condition). Upon enrollment in the Program, a Screening-Eligible Survivor is eligible for:
A one-time comprehensive initial health evaluation performed at a CCE or NPN clinic that is almost identical to the one received by enrolled responders. If the initial health evaluation does not result in any certifications and the Survivor later feels a new health problem may be WTC-related, he or she can pay out-of-pocket or use their primary health insurance for an additional health evaluation by a CCE/NPN doctor.
Certified-Eligible Survivors (ie, a Survivor with a certified WTC-related health condition) receive:
Annual comprehensive health monitoring exams performed at a CCE or NPN clinic;
Medical and mental health treatment for certified WTC-related health conditions;
Cancer screening tests (that are rated “Grade A” or “Grade B” by the U.S. Preventive Services Task Force (USPSTF);
Benefits counseling services;
Note that with respect to the payment of treatment services, certified-eligible survivors receive coordination of care, ie, they are required to obtain primary health insurance that includes both medical and pharmacy coverage. In general, the primary health insurance plan is billed first, and the WTCHP is the last payor.
It is important to note that the cohorts followed by the CCEs and NPN are open, ie, individuals can join at any time, if they meet eligibility criteria. Also, there may be financial compensation associated with some of the certified physical health diagnoses, which is available through the September 11 Victim Compensation Fund, administered by the US Department of Justice (https://www.vcf.gov/). Additional information on eligibility and enrollment benefits is available in the Program’s Administrative Manual, which can be found at https://www.cdc.gov/wtc/ppm.html.
Promoting high quality health care
Recognizing the needs of the busy clinician, the goal for each paper in this series is to be brief while communicating vital medical care information to the general medical and public health community. Each paper is authored by health care professionals, most of whom are affiliated with the WTC Health Program and who have many years of experience treating and/or conducting research studies in this population. Each paper generally provides links to the one or two most relevant Clinical Practice Guidelines (CPGs) that address the featured condition. In addition to the CPG Web links and/or bibliographic citations, each paper provides concise background information on the condition, including research findings from WTC-exposed populations, briefly summarizes key diagnostic and treatment information extracted from selected CPGs, and finally, explains where WTC Health Program diagnostic and treatment coverage information can be found. Further information on research conducted on WTC-related diseases is available from the Web sites provided in Table 1.
Table 1.
Organizations and websites that provide updated WTC research.
| Organization | Website |
|---|---|
| National Institute for Occupational Safety and Health (NIOSH) WTC research compendium | https://wwwn.cdc.gov/ResearchGateway/Publications/CompendiumArchive |
| WTC Health Registry. Peer-reviewed scientific publications, annual reports, and technical reports | https://www1.nyc.gov/site/911health/researchers/published-research-publications.page |
Identifying Clinical Practice Guidelines (CPGs)
Most of the CPGs found in the papers in this series were identified in the ECRI (Emergency Care Research Institute) Guidelines Trust (https://guidelines.ecri.org/). ECRI is an independent not-for-profit organization that was created in 1968. The ECRI Guidelines Trust was initiated in 2018, essentially filling the former role of the National Guideline Clearinghouse before it was defunded in 2018.15 The ECRI Guidelines Trust, as the National Guideline Clearinghouse previously did, provides a compendium of CPGs that meet prespecified inclusion criteria. The ECRI Guidelines Trust inclusion criteria for CPGs are:
Less than 5 years old, available on the Internet (regardless of fee requirements for access), and available in English;
Includes recommendation statements providing patient care guidance;
Produced by a medical specialty association, professional medical society, or other relevant CPG development organization;
- Based on a verifiable systematic review of evidence, including
- Search strategy (databases used; search terms used; time-period covered by search);
- Study selection (total number of documents found; number that met inclusion criteria; summary of inclusion criteria)
- Evidence analysis (evidence tables OR GRADE tables OR a narrative synthesis of evidence). GRADE (Grading of Recommendations, Assessment, Development and Evaluations) is a transparent framework for developing Clinical Practice Guidelines.16
For the CPGs identified through the ECRI Guidelines Trust, this series of Archives papers cited only those that were of high quality. We defined high quality as a score of three or higher (out of five) for all items in NEATS (National Guideline Clearinghouse Extent of Adherence to Trustworthy Standards). NEATS is a popular and well-established CPG appraisal tool.17 When ECRI didn’t score a CPG (eg ECRI doesn’t score CPGs when it isn’t granted permission to do so by the CPG developer, nor when it cannot confirm that it was based on a verifiable systematic review of evidence), or when a CPG wasn’t identified through ECRI, those CPGs were scored by two or more members of the Work Group, using NEATS. Only those found to be of high quality are cited in this series of Archives papers.
In general, we found that the number of high quality, recent CPGs is limited. It was unusual to find more than one or two high quality and recent CPGs that addressed a given medical condition. As such, we rarely confronted the situation of choosing from more than two high quality CPGs.
Given that the CPGs cited in the 2008 NYC DOHMH are more than a decade old,7 none are cited in the best practices papers published in this issue of Archives. Some of the CPGs cited by the 2008 Guidelines are periodically updated, and those updated versions are cited in this issue of the Archives. However, for many of the CPGs cited in this issue, earlier versions were not cited in the 2008 guidelines, often because earlier versions of those CPGs didn’t exist in 2008. It is beyond the scope of this series of Archives papers to explain how each CPG was updated. However, for the interested reader, each CPG provides details on how the CPG was updated, since this information is required to classify a CPG as high quality.
In this series of Archives papers, consensus documents are occasionally referenced. Those consensus documents do not include a systematic review but followed all other ECRI criteria for a CPG. As such, consensus documents were not scored. An example of a consensus document is a consensus recommendation from the US Multi-Society Task Force on Colorectal Cancer. That consensus document provides time interval recommendations for when a follow-up screening colonoscopy should occur after a prior colonoscopy.18
Conclusion
The WTC-related papers on clinical best practices found in this issue of the Archives represent an update of the Clinical Guidelines that were last revised in 2008 under the direction of the NYC DOHMH. The purpose of this update is to help ensure that the health care delivered to WTC Health Program members is of high quality. A workgroup to accomplish this task was formed in April 2021 and consists of clinicians affiliated with the WTC Health Program. The format of this series of best practices was designed to be cognizant of the extremely busy clinician. Each paper in the series includes a brief summary of information on the condition, including research findings from WTC-exposed populations, a summary of key diagnostic and treatment information extracted from selected CPG(s), and concludes by explaining where WTC Health Program diagnostic and treatment coverage information can be found.
Acknowledgments
The authors thank the 9/11 rescue, response, recovery and cleanup workers and survivors who participate in the WTC Health Program, and the healthcare professionals dedicated to their care. The authors also sincerely thank Kenneth Rosenman, MD and Nicholas Newman, DO for generously providing technical expertise and review.
Funding
Drs. Calvert, Anderson and Lilly are employees of the US federal government and contributed to this paper as part of their official job duties. Work on this paper was also supported by the Centers for Disease Control and Prevention using the following funding mechanisms: contract 200-2017-93327 (Reibman); contract 200-2017-93427 (Reibman, Rosen); contract 200-2017-93430 (Harrison, Haugen, Werth); contract 75D30121C10118 (Cochran); contract 200-2016-88504 (Cochran); contract 200-2017-93428 (Lowe); contract 200-2017-93432 (Luft); contract 200-2017-93429 (Moline); contract 200-2017-93431 (Udasin); cooperative agreement 2U50/OH009739 (Cone); and, cooperative agreement 5U50/OH009739 (Cone).
Footnotes
Disclosure statement
The authors report there are no competing interests to declare.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). Mention of any company or product does not constitute endorsement by NIOSH/CDC. In addition, citations to websites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these websites. All web addresses referenced in this document were accessible as of the publication date.
Institutional review board (IRB) review
This activity did not involve human subjects and therefore did not require IRB review.
References
- 1.Murphy J, Brackbill RM, Thalji L, Dolan M, Pulliam P, Walker DJ. Measuring and maximizing coverage in the World Trade Center Health Registry. Stat Med. 2007;26(8):1688–1701. doi: 10.1002/sim.2806. [DOI] [PubMed] [Google Scholar]
- 2.Farfel M, DiGrande L, Brackbill R, et al. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health. 2008;85(6):880–909. doi: 10.1007/s11524-008-9317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wallingford KM, Snyder EM. Occupational exposures during the World Trade Center disaster response. Toxicol Ind Health. 2001;17(5-10):247–253. doi: 10.1191/0748233701th112oa. [DOI] [PubMed] [Google Scholar]
- 4.Lippmann M, Cohen MD, Chen LC. Health effects of World Trade Center (WTC) dust: an unprecedented disaster’s inadequate risk management. Crit Rev Toxicol. 2015;45(6):492–530.doi: 10.3109/10408444.2015.1044601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santiago-Colón A, Daniels R, Reissman D, et al. World Trade Center Health Program: first decade of research. IJERPH. 2020;17(19):7290. doi: 10.3390/ijerph17197290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daniels RD, Carreón T, Bilics JA, Reissman DB, Howard J. The World Trade Center Health Program: petitions for adding qualifying health conditions. Am J Ind Med. 2021;64(10):885–892. doi: 10.1002/ajim.23267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedman S, Cone J, Eros-Sarnyai M, et al. Clinical guidelines for adults exposed to the World Trade Center disaster. City Health Information. 2008;27(6):41–54. [Google Scholar]
- 8.NIOSH. 2018. Development of the inventory of 9/11 agents. Washington DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, https://wwwn.cdc.gov/ResearchGateway/Content/pdfs/Development_of_the_Inventory_of_9-11_Agents_20180717.pdf. [Google Scholar]
- 9.Clark R, Meeker G, Plumlee G, et al. 2002. USGS environmental studies of the World Trade Center area, New York City, after September 11, 2001 [US Geological Survey Web site]. http://pubs.usgs.gov/fs/fs-0050-02/fs-050-02_508.pdf. [Google Scholar]
- 10.Landrigan PJ, Lioy PJ, Thurston G, et al. Health and environmental consequences of the World Trade Center disaster. Environ Health Perspect. 2004;112(6): 731–739. doi: 10.1289/ehp.6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NIOSH. 2015. Policy and procedures for certification of physician determinations for aerodigestive and cancer health conditions. Washington DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, https://www.cdc.gov/wtc/pdfs/policies/WTCHPPPCertPhysDetFINAL20Feb2015-508.pdf. [Google Scholar]
- 12.Jordan HT, Osahan S, Li J, et al. Persistent mental and physical health impact of exposure to the September 11, 2001 World Trade Center terrorist attacks. Environ Health. 2019;18(1):12. doi: 10.1186/s12940-019-0449-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). New York City Department of Health response to terrorist attack. MMWR Morb Mortal Wkly Rep. 2001; 50(38):821–822. [PubMed] [Google Scholar]
- 14.Azofeifa A, Martin GR, Santiago-Colón A, Reissman DB, Howard J. World Trade Center Health Program - United States, 2012-2020. MMWR Surveill Summ. 2021;70(4):1–21. doi: 10.15585/mmwr.ss7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerberich A, Spencer S, Ipema H. National guideline clearinghouse is no more: keep calm and search on. Ann Pharmacother. 2019;53(4):434–436. doi: 10.1177/1060028018815852. [DOI] [PubMed] [Google Scholar]
- 16.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jue JJ, Cunningham S, Lohr K, et al. Developing and testing the agency for healthcare research and quality’s National Guideline Clearinghouse Extent of Adherence to Trustworthy Standards (NEATS) instrument. Ann Intern Med. 2019;170(7):480–487. doi: 10.7326/M18-2950 [DOI] [PubMed] [Google Scholar]
- 18.Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US multi-society task force on colorectal cancer. Am J Gastroenterol. 2020;115(3):415–434. doi: 10.14309/ajg.0000000000000544. [DOI] [PMC free article] [PubMed] [Google Scholar]