Summary:
The integrated plastic surgery residency match has risen to be the most competitive specialty in the 2022 match. This reality has prompted medical students to reach a high level of personal achievements, including pursuing research fellowships to boost research productivity. The competitive nature of this specialty has highlighted several barriers for applicants, such as those from groups underrepresented in surgery, of lower socioeconomic backgrounds, or without a home program. In recent years, there have been several changes to the match that stand to attenuate disparities among applicants, such as the transition to virtual interviews and the shift of the United States Medical Licensing Examination Step 1 score to pass-fail. The introduction of the Plastic Surgery Common Application and standardized letters of recommendation has altered the application process for the plastic surgery match. Given these recent trends, evaluating the current landscape and looking toward future directions for the integrated plastic surgery match becomes necessary. Understanding these changes will not only benefit medical students by giving them a transparent look into the match process but also provide a framework for other specialties to follow to increase accessibility to their specific specialty.
Takeaways
Question: How are recent changes to the integrated plastic surgery match affecting those involved?
Findings: With the transition of USMLE Step 1 to pass-fail scoring, integrated plastic surgery programs will increasingly emphasize research productivity and applicant familiarity. The Plastic Surgery Common Application's introduction appears to decrease costs for applicants while improving the recommendation letter upload process for writers. There is still debate over whether these changes will improve equity in the match.
Meaning: This article looks at recent changes in the match, which will provide transparency to medical students, while also providing a framework for other competitive specialties looking to increase accessibility into their fields.
INTRODUCTION
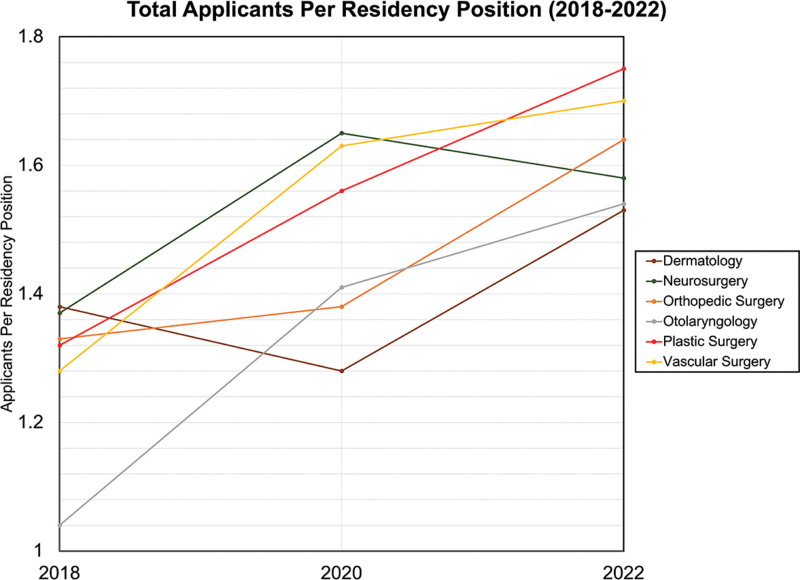
An increasing number of qualified applicants participate in the residency match every year. In 2021, the number of applicants reached 42,508, an all-time high.1 Unfortunately, the number of residency positions has not grown proportionally, leading to decreased match rates across specialties. Competitive specialties, such as plastic surgery, have fewer positions available in the match than medical doctor (MD) seniors—residency applicants who are in their last year of medical school at a U.S. MD granting institution—who prefer each specialty (Fig. 1).2–5
Fig. 1.
A graph that shows the total applicants per residency position for multiple specialties (2018–2022).2–4
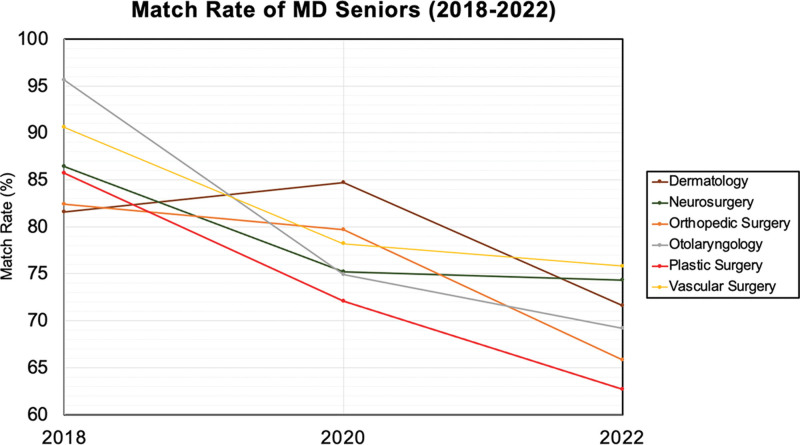
Integrated plastic surgery residency was the most competitive specialty in the 2022 match, with an applicant match rate of around 55%. The match rate for MD seniors has dropped by 23%, from 85.7% in 2018 to 62.7% in 2022. This is the most significant decrease in match rate reported by National Resident Matching Program data (Fig. 2). Additionally, applicant achievement, particularly research productivity, has grown tremendously. To improve their chances in the match, many applicants utilize financially burdensome options, such as research fellowships, multiple away rotations, and submitting applications to numerous residency programs nationwide, making integrated plastic surgery one of the costliest medical specialties.6–8
Fig. 2.
A graph that shows the match rate of MD seniors for multiple specialties (2018–2022).2–4
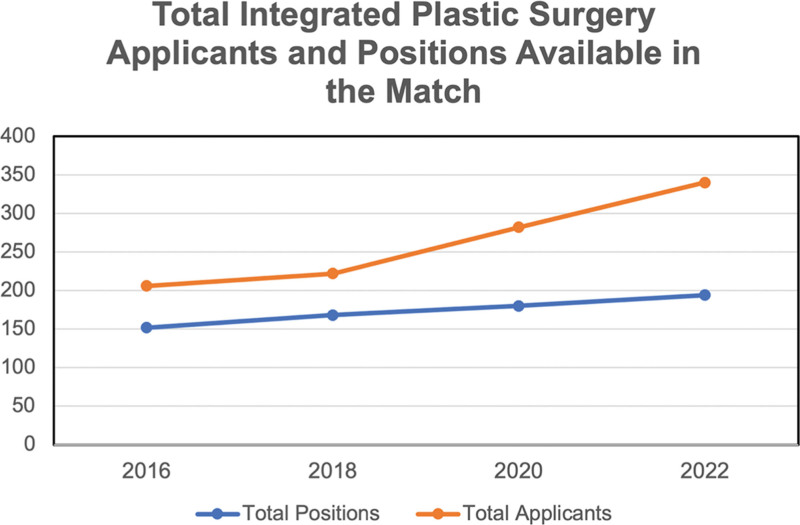
Overall, the volume of applicants applying, coupled with the increasing applicant academic success, without a proportional increase in positions available, makes the integrated plastic surgery match process both costly and risky (Fig. 3). Recent changes, such as the transition to virtual interviews after the COVID-19 pandemic, the Plastic Surgery Common Application (PSCA) introduction, and the looming shift to a pass-fail (P/F) United States Medical Licensing Examination (USMLE) Step 1 score, have altered the overall selection process for applicants and residency program selection committees. This review will examine the integrated plastic surgery match’s current landscape and future directions.
Fig. 3.
A graph that shows the number of applicants and positions available in the integrated plastic surgery match (2016–2022).2–4
TRANSITION TO PASS/FAIL USMLE STEP 1 SCORES
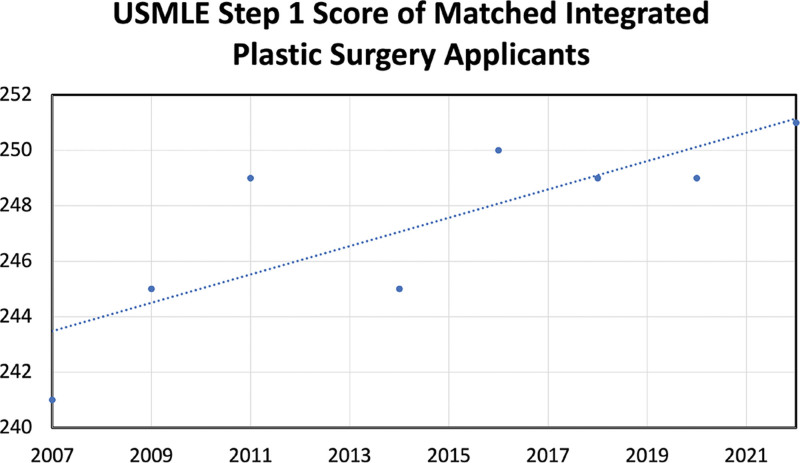
Historically, USMLE scores have been utilized as a quick metric to differentiate applicants in the match.9,10 Many programs require a “cutoff score” for a holistic application review.11,12 Step 1 scores have been positively associated with the total number of interview invites and match rates for the integrated plastic surgery applicant.13,14 Matched applicants’ Step 1 scores have trended upward for the past few years, supporting the increased academic achievement of the applicant pool (Fig. 4).1 Overall, current literature overwhelmingly endorses the importance of Step 1 scores for success in the match.
Fig. 4.
A graph that shows the average USMLE Step 1 score of matched integrated plastic surgery residents with a linear growth trendline (2007–2022).1
In 2020, the National Board of Medical Examiners and the Federation of State Medical Boards revealed that the Step 1 examination results would no longer have a visible score. Test takers would receive a P/F mark beginning in 2022.15 The transition was made because the three-digit scoring system was suggested to augment disparities for disadvantaged and underrepresented groups.16 Furthermore, they argued that a P/F scoring system would improve the overall wellness of all medical students.16,17
While the effects of this modification are to be determined, some have proposed other metrics, replacing Step 1 as the primary objective metric for resident selection.18–20 Many students may utilize their Step 2CK as a preselection system of measurement for their future specialty options as they did for Step 1 in the past.21
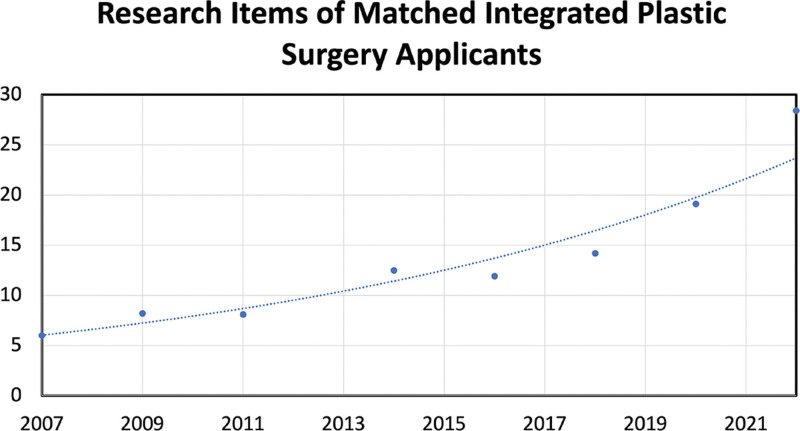
Even with a scored Step 1 examination, research productivity has been increasingly emphasized in the integrated plastic surgery match. In the past 10 years, the number of abstracts, presentations, and publications of the matched integrated plastic surgery applicant has grown exponentially (Fig. 5).1 With the transition to a P/F Step 1 examination, this trend is expected to continue, with many prospective applicants opting to complete research fellowships to demonstrate their interest in the field and capacity for research. A survey of integrated plastic surgery applicants indicated that most applicants complete research fellowships to strengthen their applications to the match.7 With increased pressure to produce research, the intent of many applicants may shift away from pursuing projects that are slower to publish, such as those in the basic sciences, in favor of those that are easier or quicker to publish.22
Fig. 5.
A graph that shows the number of research items for matched integrated plastic surgery applicants with an exponential growth trend line (2007–2022).1
However, an increased emphasis on research productivity is not without its pitfalls. Applicants without a home program in the top 40 of National Institutes of Health funding are clearly disadvantaged in research opportunities.23,24 Furthermore, most integrated plastic surgery programs are at well-funded institutions, making this a compounding disadvantage for these applicants who lack both a home program and research prospects.25 While not all substantially impactful articles require funding, available financial support increases opportunities and capacity to publish.26
Many applicants who complete research fellowships are not funded, causing an accumulation of interest on student loan debt.27 This endeavor not only adds a year of medical school but is also financially costly, disadvantaging students from lower socioeconomic backgrounds. Transitioning to a P/F Step 1 pushes many integrated plastic surgery applicants toward pursuing a research fellowship. This change may exacerbate disparities for those from disadvantaged backgrounds rather than reducing inequalities as initially intended.
THE INTRODUCTION OF THE PLASTIC SURGERY COMMON APPLICATION
The Electronic Residency Application Service (ERAS) was introduced over 20 years ago by the Association of American Medical Colleges as a computerized system intended to streamline the United States residency application process.28 Before ERAS, many programs utilized their distinct application form only provided to applicants who requested the document.29 Due to the effort required to apply to an individual program, most applicants only applied to around a dozen programs.30 Since then, however, the average number of applications per applicant has skyrocketed alongside the average cost per application. An integrated plastic surgery applicant applying to 90 programs through ERAS will pay over $2000.31 To cover these costs, 33.8% of applicants obtained supplemental funding, while 30.7% of applicants admitted to utilizing supplementary income. Numerous groups have described the process as a Prisoner’s Dilemma of game theory, where applying to as many programs as possible becomes the main tactic in the application process. At the same time, match rates remain relatively stagnant.32–34
The PSCA was introduced as a potential cost-free alternative to ERAS for plastic surgery residency applicants (Table 1). The creators of the PSCA claimed that their service was superior to ERAS by limiting the number of experiences and research items in the application, making each application more concise and focused.35 The program was initially piloted for the 2020–2021 match cycle. All 86 integrated plastic surgery programs were invited to partake in the pilot, 20 of which agreed to participate. These 20 programs accepted applications through ERAS and PSCA. In a follow-up survey, applicants and reviewers believed that the PSCA could be a legitimate alternative to the status quo, citing cost-effectiveness as a major benefit over ERAS.36
Table 1.
Side-by-Side Comparison of the PSCA versus ERAS
| PSCA | ERAS | |
|---|---|---|
| Cost | Free of cost | Costly |
| Letter upload process | Streamlined process for academic plastic surgery letter writers | Letter writers must upload after email request |
| Output | Concise output | Lengthy output |
| Signaling | Program signaling | No program signaling |
| Application sorting | No formal application sorting mechanism | Applications can be sorted by examination scores |
| Personal statement and letter assignment | Only one personal statement and four uploaded letters of recommendation max that are visible to every program that applicant applied to | Allows for program-specific assignment of letters of recommendation and personal statements |
| Specialty-specific customization | Specialty customization with short answer questions | No specialty customization |
| Timeline | Timeline flexibility | Uniform application timeline |
| Familiarity | Medical school administrators are relatively unfamiliar with the system | More familiarity and visibility with medical school support administrators |
| Listing of accomplishments and activities | Applicants are limited in the number of activities, research items, and accomplishments they can list | Allows applicants to list all activities, research items, and accomplishments |
| Logistics | Technical difficulties in earlier versions | Relatively few technical issues |
The PSCA 2.0 was introduced for the 2021–2022 application cycle, intended for use as a side-by-side comparison with ERAS.37 Only 17 programs participated in the second version of the PSCA. For the following 2022–2023 cycle, almost every program utilized the PSCA in some fashion, with 58 programs using both ERAS and PSCA, 22 programs using PSCA only, and five programs that solely used ERAS.38 To our knowledge, this was the first instance of an outside electronic application service overtaking ERAS in terms of use for any medical specialty in the United States.
The 2022–2023 PSCA application also introduced signaling, a process where applicants could “signal” a total of five programs that they were especially interested in. Other specialties have successfully used signaling in the past, citing that signaling allowed programs to get the most out of limited interview dates and availability in the match.39–41 Otolaryngology residency has implemented signaling, which increased interview offers relative to programs that did not signal.42 Overall, the addition of signaling in the plastic surgery residency match has been viewed as an improvement to the application process; however, the number of signals for each specialty and how programs consider applicants they received signals from still need to be researched further.
INTERACTIONS with APPLICANTS: AWAY ROTATIONS, STANDARDIZED LETTERS OF RECOMMENDATION, AND VIRTUAL INTERVIEWS
The shift from narrative letters of recommendation (LORs) to standardized LORs has gained traction over the last few decades, beginning with emergency medicine adopting this method, followed by otolaryngology and plastic surgery. LORs are instrumental in an applicant’s success with matching, often ranked as programs’ most crucial subjective factor in deciding on applicants to interview.43 Program directors endorse familiarity with the author of the letter as being extremely valuable, and a survey found that “what LORs say” and “who says it’‘ are among the most critical factors when evaluating an applicant.12,44 However, research has shown that LORs are imprecise and fall short of stratifying applicants.45 Narrative LORs are susceptible to racial bias, gender bias, and score inflation.46–48 While the latter component is more challenging to navigate, the former can be made more equitable and permit a consistent evaluation of students.
Because LORs serve as an endorsement of an applicant and are critical to a successful match, a standardized form can save the letter writer time while ensuring that critical components are not withheld. The standardized plastic surgery residency recommendation form diverges from the narrative LOR by providing a scale with previously determined applicant attributes, granting an objective review of each applicant. A scale that brings forth the same vital components of an applicant’s qualifications dramatically reduces the chance of bias and stands to eliminate hyperboles that may influence a solely narrative LOR. This method can also bring the applicant’s performance to the surface rather than allowing the letter writer’s reputation to impact the applicant’s evaluation significantly.
The COVID-19 pandemic has significantly impacted the plastic surgery match process with limitations on the number of away rotations in the 2022 match cycle and the adoption of virtual interviews, ultimately resulting in a significant increase in home institution match rates. Geographic bias has historically played a significant role in the match, with many applicants matching at their home program or a nearby regional program.49 In 2019, 14.61% matched at their home institutions versus 25.12% in 2021.50–52 However, the 2022 match cycle resulted in home institution match rates similar to previous non-COVID-19-affected years.50,53 Therefore, the return of away rotations without a corresponding return to in-person interviews highlights the significance of away rotations for students matching to external programs. Furthermore, the National Resident Matching Program program director Survey results rank “audition elective/rotation in program director’s department” and “prior personal knowledge of applicant” among the highest factors when considering whom to rank.43
While reassuring applicants of the importance of away rotations, these data can also serve as a barrier for students from socioeconomically disadvantaged backgrounds where cost is a hindering factor. A survey found that applicants spent 9.2 weeks on away rotations, and the average cost of away rotations was $3591 per applicant. This same survey also found that an away rotator filled 27% of postgraduate year 1 positions, and an additional 17% were filled by a home medical student.54 These realities can hinder financially disadvantaged students and dissuade them from pursuing a plastic surgery residency, especially considering the documented importance of away rotations in a successful match.
A positive shift can thus be appreciated with the transition from in-person to virtual interviews when considering cost as a limiting factor for applicants. The financial burden of residency interviews on medical students is well documented; in an electronic survey of U.S. allopathic seniors, 64% of respondents reported spending at least $2500, while 13% spent $7500 or more.55 Furthermore, this study showed that specialty competitiveness was predictive of higher interview costs. Plastic surgery was ranked among the most competitive specialties, with 24.7% of applicants turning down interviews for financial reasons. Another survey found that the average student spent $3500 on interviews and that 63% stated that cost was a limiting factor in accepting interviews.56,57 A retrospective analysis demonstrated that the average savings for plastic surgery residency applicants were estimated to be over $9000.8,58
An encouraging finding from a study among program directors and candidates who participated in the Complex General Surgical Oncology 2020 fellowship recruitment was that virtual interviews are favored by faculty, possibly due to their convenience, and 60% of program directors agreed or strongly agreed that it allowed for an accurate representation of the candidate.59,60 Another study evaluating virtual fellowship interviews specifically found that most applicants and program directors felt that virtual interviews were not a hindrance to matching at the top of their rank list.61 This finding agrees with Menhaji’s study, which found that over 50% of female pelvic medicine and reconstructive surgery fellowship program directors would likely continue the virtual interview format.62
Although virtual interviews are a practical option that reduces applicant costs and paves the way for a more equitable match, program directors have reported weaknesses of virtual interviews.63 Among these is a decrease in the ability of interviewers to connect with residents and an inability to assess the applicant’s interaction with administrative staff and faculty, which hinder the program’s ability to determine if the applicant is a “good fit” for the program.64 Furthermore, a survey of program directors found that 75% disagree or strongly disagree that virtual interviews made it easier to assess an applicant’s fit with the program.65 There can also be discrepancies observed among program directors and candidates, as only 50% of candidates agreed or strongly agreed that the video interview allowed for an accurate representation of the interviewer, and only 39% agreed or strongly agreed that it allowed for a precise representation of the program.59,66 Importantly, virtual interviews are not immune from all inequities. These include but are not limited to the applicant having a designated, distraction-free environment for the interview and a high-quality internet service.
Despite the weaknesses and limitations of virtual interviews, they hold the potential to significantly reduce the financial barriers applicants face, especially as away rotations become of utmost importance to a successful match. A commonality of LORs and away rotations is that they stand to introduce the applicants to the program, therefore establishing them as familiar personalities. Research has shown that although virtual interviews fall short of painting a complete picture of an applicant, program directors will likely continue them, and it can be assumed that this is the new landscape for applicants.
DISCUSSION AND FUTURE DIRECTIONS
Recent changes to the integrated plastic surgery match process intend to reduce inequities between applicants and increase the efficacy of the application process. With a decreased emphasis on Step 1 scores, medical schools may reduce the preclinical portion of the curriculum and increase clinical experiences. This trend toward increased longitudinal clinical experiences has occurred throughout medical schools worldwide.67 Medical schools that still use a traditional curriculum may need to consider whether their students appropriately utilize time in medical school. An increased emphasis on clinical curriculum could better prepare students for the Step 2CK examination and future clinical practice.
Early mentorship at outside institutions with plastic surgery residency programs is essential for students without a home plastic surgery program. Studies have shown that proximity to a plastic surgery residency program correlates with the number of mentoring relationships for mentors and mentees.68–70 Recent educational opportunities, such as the “Prepped” Sub-Internship Preparatory Program, the American Society of Plastic Surgeons Roadmaps Program, and the Plastic Surgery Diversity, Equity, and Inclusion Mentorship Program, are all new initiatives aimed at addressing disparities and improving equity for those pursuing a career in plastic surgery.46 Currently, the Plastic Surgery Diversity, Equity, and Inclusion Mentorship Program is only offered by several plastic surgery residency programs on the west coast. The introduction of similar nationwide programs could further improve equity in the plastic surgery match nationwide.
The PSCA—an alternative to ERAS—appears to be gaining momentum in terms of utilization by plastic surgery residency programs. Programs should investigate a complete transition to the PSCA from ERAS due to the difference in cost, specialty-specific improvements, and flexibility. PSCA includes a search function for familiar letter writers and a standardized letter format for plastic surgery built into the system. While there were some technical issues with the earlier versions of the program, the latest version appears to have had no problems to our knowledge. Within the PSCA, students were given five signals, each intended to signal interest in different programs. The ideal number of signals for applicants and their resulting advantage in gaining interview invites need to be researched further.
The authors recommend that other medical specialties investigate and potentially follow some of the changes made by plastic surgery programs to improve the residency application process. By creating a system like the PSCA, specialties can reduce barriers for applicants, simplify the process for all involved, and include specialty-specific actions, which could aid in applicant selection. While this transition would require a momentous effort, the benefits outweigh the costs, particularly in increasingly competitive specialties.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENT
Research is ethical and does not include specific data on animal or human subjects. All data used are available and accessible to the public.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.National Resident Matching Program, Match Data & Report Archives. National Resident Matching Program, Washington, DC. Available at https://www.nrmp.org/match-data-analytics/archives/. Accessed December 12, 2022. [Google Scholar]
- 2.National resident matching program, charting outcomes in the match: senior students of U.S. Medical Schools, 2020. Available at https://www.nrmp.org/wp-content/uploads/2021/08/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf. Accessed December 12, 2022.
- 3.National Resident Matching Program, charting outcomes in the match: U.S. Allopathic Seniors, 2018. Available at https://www.nrmp.org/wp-content/uploads/2021/07/Charting-Outcomes-in-the-Match-2018_Seniors-1.pdf. Accessed December 12, 2022.
- 4.National Resident Matching Program, charting outcomes in the match: Senior Students of U.S. Medical Schools. Available at https://www.nrmp.org/wp-content/uploads/2022/07/Charting-Outcomes-MD-Seniors-2022_Final.pdf. Accessed December 12, 2022.
- 5.Asserson DB, Sarac BA, Janis JE. A 5-Year analysis of the integrated plastic surgery residency match: the most competitive specialty? J Surg Res. 2022;277:303–309. [DOI] [PubMed] [Google Scholar]
- 6.Oladeji LO, Raley JA, Smith S, et al. Behind the match process: is there any financial difference lurking below the specialty of choice? Am Surg. 2016;82:1163–1168. [PubMed] [Google Scholar]
- 7.Mehta K, Sinno S, Thanik V, et al. Matching into integrated plastic surgery: the value of research fellowships. Plast Reconstr Surg. 2019;143:640–645. [DOI] [PubMed] [Google Scholar]
- 8.Sarac BA, Rangwani SM, Schoenbrunner AR, et al. The cost of applying to integrated plastic surgery residency. Plast Reconstr Surg Glob Open. 2021;9:e3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang F, Rudnicki PA, Prince NH, et al. An evaluation of plastic surgery resident selection factors. J Surg Educ. 2015;72:8–15. [DOI] [PubMed] [Google Scholar]
- 10.Green M, Jones P, Thomas JX, Jr. Selection criteria for residency: results of a national program directors survey. Acad Med. 2009;84:362–367. [DOI] [PubMed] [Google Scholar]
- 11.Schultz KP, Shih L, Davis MJ, et al. integrated plastic surgery applicant review: important factors and selection criteria. Plast Reconstr Surg Glob Open. 2020;8:e2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janis JE, Hatef DA. Resident selection protocols in plastic surgery: a national survey of plastic surgery program directors. Plast Reconstr Surg. 2008;122:1929–1939. [DOI] [PubMed] [Google Scholar]
- 13.LaGrasso JR, Kennedy DA, Hoehn JG, et al. Selection criteria for the integrated model of plastic surgery residency. Plast Reconstr Surg. 2008;121:121e–125e. [DOI] [PubMed] [Google Scholar]
- 14.Sarac BA, Janis JE. Matching into plastic surgery: insights into the data. Plast Reconstr Surg Glob Open. 2022;10:e4323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Medical Licensing Examination. USMLE Step 1 Transition to Pass/Fail Only Score Reporting. 20221. Available at https://www.usmle.org/usmle-step-1-transition-passfail-onlyscore-reporting. Accessed December 12, 2022. [Google Scholar]
- 16.McDade W, Vela MB, Sánchez JP. Anticipating the Impact of the USMLE Step 1 Pass/Fail scoring decision on underrepresented-in-medicine students. Acad Med. 2020;95:1318–1321. [DOI] [PubMed] [Google Scholar]
- 17.Bloodgood RA, Short JG, Jackson JM, et al. A change to pass/fail grading in the first two years at one medical school results in improved psychological well-being. Acad Med. 2009;84:655–662. [DOI] [PubMed] [Google Scholar]
- 18.Lin LO, Makhoul AT, Hackenberger PN, et al. Implications of pass/fail step 1 scoring: plastic surgery program director and applicant perspective. Plast Reconstr Surg Glob Open. 2020;8:e3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asaad M, Drolet BC, Janis JE, et al. Applicant familiarity becomes most important evaluation factor in USMLE step I conversion to pass/fail: a survey of plastic surgery program directors. J Surg Educ. 2021;78:1406–1412. [DOI] [PubMed] [Google Scholar]
- 20.Raborn LN, Janis JE. Current views on the new United States medical licensing examination step 1 pass/fail format: a review of the literature. J Surg Res. 2022;274:31–45. [DOI] [PubMed] [Google Scholar]
- 21.Sergesketter AR, Shammas RL, Langdell HC, et al. Predicting academic performance during plastic surgery residency: can step 2 scores reliably replace step 1? J Surg Educ. 2022;79:828–836. [DOI] [PubMed] [Google Scholar]
- 22.Jinka SKA, Janis JE. Publication times and integrated plastic surgery applicant planning. Plast Reconstr Surg Glob Open. 2021;9:e4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryan EM, Geelan-Hansen KR, Nelson KL, et al. Examining the otolaryngology match and relationships between publications and institutional rankings. OTO Open. 2020;4:2473974x–20932497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keane CA, Akhter MF, Sarac BA, et al. Characteristics of successful integrated plastic surgery applicants from US allopathic medical schools without a home integrated program. J Surg Educ. 2022;79:551–557. [DOI] [PubMed] [Google Scholar]
- 25.Keane CA, Akhter MF, Sarac BA, et al. integrated plastic surgery programs have been implemented at top grant-receiving institutions. Plast Reconstr Surg Glob Open. 2021;9:e3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Asserson DB, Janis JE. Majority of most-cited articles in top plastic surgery journals do not receive funding. Aesthet Surg J. 2021;41:NP935–NP938. [DOI] [PubMed] [Google Scholar]
- 27.Mellia JA, Mauch JT, Broach RB, et al. Moving the goalposts: inequity concerns regarding research years and the integrated plastic surgery match. Plast Reconstr Surg. 2021;148:1086e–1087e. [DOI] [PubMed] [Google Scholar]
- 28.Mandel LP, Spadoni LR, Hewitson LA, et al. One residency’s experience with the electronic residency application service. Fam Med. 1997;29:209–212. [PubMed] [Google Scholar]
- 29.Taylor CA, Mayhew HE, Weinstein L. Residency directors’ responses to the concept of a proposed electronic residency application service. Acad Med. 1994;69:138–142. [DOI] [PubMed] [Google Scholar]
- 30.Carmody JB, Rosman IS, Carlson JC. Application fever: reviewing the causes, costs, and cures for residency application inflation. Cureus. 2021;13:e13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Association of American Medical Colleges. Fees for ERAS residency applications. 2022. Available at https://students-residents.aamc.org/applying-residencies-eras/fees-eras-residency-applications. Accessed December 13, 2022. [Google Scholar]
- 32.Berger JS, Cioletti A. Viewpoint from 2 graduate medical education deans application overload in the residency match process. J Grad Med Educ. 2016;8:317–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weissbart SJ, Kim SJ, Feinn RS, et al. Relationship between the number of residency applications and the yearly match rate: time to start thinking about an application limit? J Grad Med Educ. 2015;7:81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molina-Burbano F, Yao A, Burish NM. The plastic surgery prisoner’s dilemma: the relationship between applications and match rate. Plast Reconstr Surg Glob Open. 2018;6(7S):e154. [Google Scholar]
- 35.Jackson KR, Makhoul AT, Janis JE, et al. The plastic surgery common application: improving efficiency and reducing inequity in the application process. Plast Reconstr Surg Glob Open. 2022;10:e4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elmer NA, Veeramani A, Bustos VP, et al. Perspectives on the plastic surgery common application (PSCA): a survey of 2021-2022 integrated plastic surgery applicants. Plast Reconstr Surg Glob Open. 2023;11:e4766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Plastic surgery Common Application 2021-2022. Available at: https://psca.smapply.io/. Accessed December 12, 2022.
- 38.Applying to plastic surgery. American Council of Academic Plastic Surgeons. 2022. Available at https://acaplasticsurgeons.org/PSCA/. Accessed December 13, 2022.
- 39.Chang CWD, Throne MC, Malekzadeh S, et al. Two-year interview and match outcomes of otolaryngology preference signaling. Otolaryngol Head Neck Surg. 1312;2022:194599822112. [DOI] [PubMed] [Google Scholar]
- 40.Fantasia J, Elsamra S, Thavaseelan S. Improving the match: use of preference signaling to optimize the urology match interview process. Urology. 2021;154:57–61. [DOI] [PubMed] [Google Scholar]
- 41.Mun F, Suresh KV, Li PT, et al. Preference signaling for orthopaedic surgery applicants: a survey of residency program directors. J Am Acad Orthop Surg. 2022;30:1140–1145. [DOI] [PubMed] [Google Scholar]
- 42.Pletcher SD, Chang CWD, Thorne MC, et al. The otolaryngology residency program preference signaling experience. Acad Med. 2022;97:664–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National resident matching program, data release and research committee: results of the 2021 NRMP program director survey. National Resident Matching Program, Washington, DC. 2021. Available at https://www.nrmp.org/wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf. Accessed December 13, 2022. [Google Scholar]
- 44.Shultz K, Mahabir RC, Song J, et al. Evaluation of the current perspectives on letters of recommendation for residency applicants among plastic surgery program directors. Plast Surg Int. 2012;2012:728981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fortune JB. The content and value of letters of recommendation in the resident candidate evaluative process. Curr Surg. 2002;59:79–83. [DOI] [PubMed] [Google Scholar]
- 46.Reghunathan M, Crowley JS, Segal R, et al. Plastic surgery diversity, equity, and inclusion (DEI) mentorship program and workshop: a single institution’s experience. Plast Reconstr Surg. 2022;151:226–229. [DOI] [PubMed] [Google Scholar]
- 47.Grimm LJ, Redmond RA, Campbell JC, et al. Gender and racial bias in radiology residency letters of recommendation. J Am Coll Radiol. 2020;17:64–71. [DOI] [PubMed] [Google Scholar]
- 48.Trix F, Psenka C. Exploring the color of glass: letters of recommendation for female and male medical faculty. Discourse and Society. 2003;14:191–220. [Google Scholar]
- 49.Nagarkar PA, Janis JE. Eliminating geographic bias improves match results: an analysis of program preferences and their impact on rank lists and results. Plast Reconstr Surg. 2018;142:82e–88e. [DOI] [PubMed] [Google Scholar]
- 50.Kebede S, Marxen T, Om A, et al. COVID-19 and the integrated plastic surgery match: an update on match trends by applicant location. Plast Reconstr Surg Glob Open. 2022;10:e4527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Antezana LA, Rode M, Muro-Cardenas J, et al. Home sweet home: the integrated plastic surgery residency match during the COVID-19 pandemic. Plast Reconstr Surg. 2022;150:492e–494e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarac BA, Janis JE. Virtual interviews in plastic surgery. Plast Reconstr Surg Glob Open. 2021;9:e3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nagarkar PA, Janis JE. Unintended bias and unintended consequences: geographic bias in the plastic surgery residency match. Plast Reconstr Surg Glob Open. 2022;10:e4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Drolet BC, Brower JP, Lifchez SD, et al. Away rotations and matching in integrated plastic surgery residency: applicant and program director perspectives. Plast Reconstr Surg. 2016;137:1337–1343. [DOI] [PubMed] [Google Scholar]
- 55.Fogel HA, Liskutin TE, Wu K, et al. The economic burden of residency interviews on applicants. Iowa Orthop J. 2018;38:9–15. [PMC free article] [PubMed] [Google Scholar]
- 56.Walling A, Nilsen K, Callaway P, et al. Student expenses in residency interviewing. Kans J Med. 2017. 30;10:1–15. [PMC free article] [PubMed] [Google Scholar]
- 57.Shen AH, Shiah E, Sarac BA, et al. Plastic surgery residency applicants’ perceptions of a virtual interview cycle. Plast Reconstr Surg. 2022;150:930–939. [DOI] [PubMed] [Google Scholar]
- 58.Gordon AM, Sarac BA, Drolet BC, et al. Total costs of applying to integrated plastic surgery: geographic considerations, projections, and future implications. Plast Reconstr Surg Glob Open. 2021;9:e4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hill MV, Ross EA, Crawford D, et al. Program and candidate experience with virtual interviews for the 2020 complex general surgical oncology interview season during the COVID pandemic. Am J Surg. 2021;222:99–103. [DOI] [PubMed] [Google Scholar]
- 60.Sarac BA, Janis JE. Perspectives of virtual residency interviews in plastic surgery: results following 1 year of training. Plast Reconstr Surg Glob Open. 2023;11:e4746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robinson KA, Shin B, Gangadharan SP. A comparison between in-person and virtual fellowship interviews during the COVID-19 pandemic. J Surg Educ. 2021;78:1175–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Menhaji K, Gaigbe-Togbe BH, Hardart A, et al. Virtual interviews during COVID-19: perspectives of female pelvic medicine and reconstructive surgery program directors. Female Pelvic Med Reconstr Surg. 2021;27:575–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sarac BA, Shen AH, Nassar AH, et al. Virtual interviews for the integrated plastic surgery residency match: the program director perspective. Plast Reconstr Surg Glob Open. 2021;9:e3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Relke N, Soleas E, Lui CJ. Internal medicine residents’ and program directors’ perception of virtual interviews during COVID-19: a national survey. Can Med Educ J. 2022;13:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rajesh A, Asaad M, Elmorsi R, et al. The virtual interview experience for MATCH 2021: a pilot survey of general surgery residency program directors. Am Surg. 8555;2021:3134821103. [DOI] [PubMed] [Google Scholar]
- 66.Hemal K, Sarac BA, Boyd CJ, et al. Applicant preferences for virtual interviews: insights from the 2020-21 integrated plastic surgery application cycle. Plast Reconstr Surg Glob Open. 2021;9:e3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Norris TE, Schaad DC, DeWitt D, et al. ; Consortium of Longitudinal Integrated Clerkships. Longitudinal integrated clerkships for medical students: an innovation adopted by medical schools in Australia, Canada, South Africa, and the United States. Acad Med. 2009;84:902–907. [DOI] [PubMed] [Google Scholar]
- 68.Barker JC, Rendon J, Janis JE. Medical student mentorship in plastic surgery: the mentee’s perspective. Plast Reconstr Surg. 2016;137:1934–1942. [DOI] [PubMed] [Google Scholar]
- 69.Janis JE, Barker JC. Medical student mentorship in plastic surgery: the mentor’s perspective. Plast Reconstr Surg. 2016;138:925e–935e. [DOI] [PubMed] [Google Scholar]
- 70.Raborn LN, Janis JE. Overcoming the impact of COVID-19 on surgical mentorship: a scoping review of long-distance mentorship in surgery. J Surg Educ. 2021;78:1948–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]