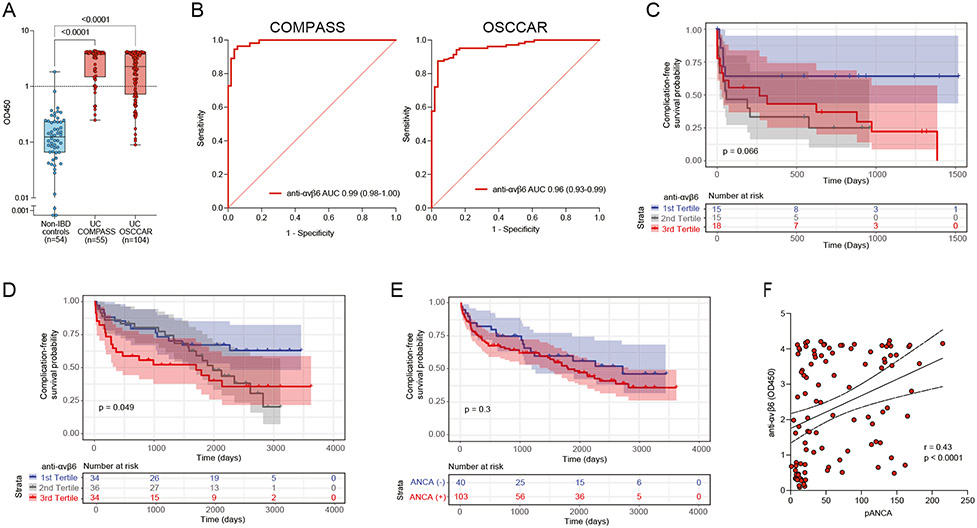
Figure 2.
Anti-αvβ6 autoantibodies in patients with newly diagnosed UC and their association with adverse disease-related outcomes. (A) Anti-αvβ6 autoantibody absorbance values (OD450) determined by means of ELISA in non-IBD controls (n = 54, shown in blue), in COMPASS patients with UC (n = 55, shown in red), and in OSCCAR patients with UC (n = 104, shown in red). (B) ROC analysis of anti-αvβ6 autoantibodies in both COMPASS patients with UC (left) and OSCCAR patients with UC (right) compared with the non-IBD controls. (C, D) Kaplan-Meier curve for composite outcome of IBD hospitalization, proximal disease extension, need for surgery, systemic steroid use, and/or requiring new biologic therapy in the COMPASS cohort (C) and OSCCAR cohort (D) stratified by anti-αvβ6 titer tertiles. The blue line represents the first tertile (lowest), the gray line represents the second tertile, and the red line the third (highest) tertile. (E) Kaplan-Meier curve for the same composite outcomes in the OSCCAR cohort stratified according to the presence or absence of pANCA. (F) Spearman correlation between pANCA and anti-αvβ6 titers.