Figure 1.
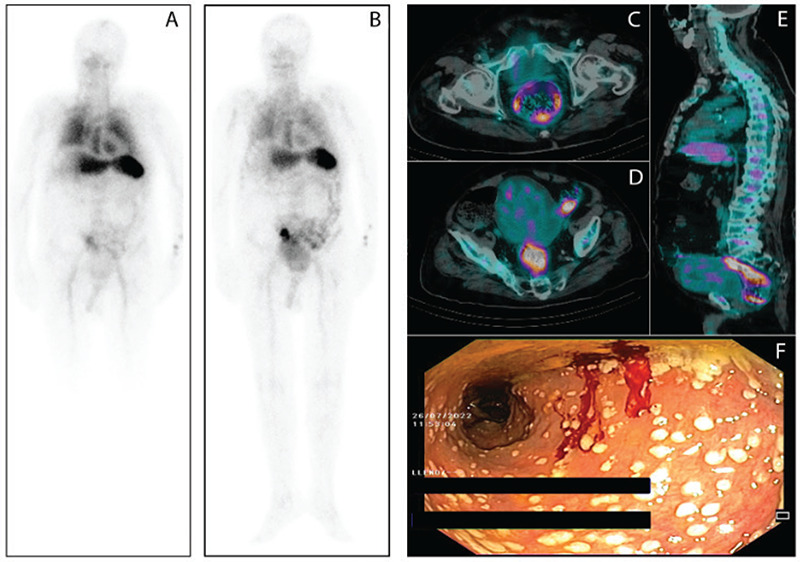
An 88-year-old man with a 1-month daily fever >38.5 °C and hyporexia. All other systems were reviewed and were negative. The patient had a past medical history of arterial hypertension and type 2 diabetes mellitus. There were no remarkable findings in the physical examination for a body temperature of 38.9 °C. At admission, the laboratory findings were as follows: hemoglobin, 9.8 gr/dL; white blood cell count, 18,840/mm3; erythrocyte sedimentation rate, 103 mm/h; C-reactive protein, 215 mg/L; and procalcitonin, 1.38 ng/mL. Blood and urine cultures, viral serology, immunological profile, abdominal ultrasound, chest radiology, and echocardiogram were negative. Technetium-99m (Tc-99m)-hexamethylpropylene amine oxime (HMPAO)-labeled leukocytes single-photon emission computed tomography/computed tomography (SPECT/CT) was requested to identify the location of a probable occult infection. Planar images of the whole body were obtained after 30 min (A) and 3 h postinjection with thoraco abdomino pelvic SPECT/CT at 3 hours post injection. Planar images of the whole body at 3 h post-injection of Tc-99m-HMPAO-labeled leukocytes revealed increased uptake in the rectum and sigmoid colon (B). SPECT/CT fusion images showed pathological Tc-99m-HMPAO-labeled leukocytes uptake in the walls of the rectum, sigmoid, and descending colon (C, D, E). In view of the previous findings, colonoscopy was performed revealing multiple white-grey small plaques with mild erythema of the surrounding mucosa along the rectosigmoid and descending colon (F). These lesions were suggestive of pseudomembranous colitis, so rectal samples for microbiological studies and mucosal biopsies were taken. Polymerase chain reaction assays detected toxinogenic Clostridium difficile in the clinical isolates. Histological examination showed isolated focuses of ulceration and crypts with reactive changes and focal atrophy, neutrophil infiltration, and hyalinization of the lamina propriam. The patient was treated with oral vancomycin with subsequent cessation of fever and improvement of laboratory parameters. Fever of unknown origin (FUO) represents a complex diagnostic challenge due to the wide range of causes that could cause it including neoplastic, infectious, rheumatic/inflammatory, and miscellaneous disorders. This entity is defined by three criteria: 1) body temperature ≥38.3 °C, 2) minimum duration of 3 weeks, and 3) etiology unidentified despite an extended work-up (1). There are several nuclear medicine techniques that are valuable tools for guiding etiologic diagnosis in the setting of FUO (2). One of these is Tc-99m-HMPAO labeled leukocyte scintigraphy, which is a diagnosis method that allows in most cases the localization and evaluation of the extension of an occult infection (3,4). The usual clinical picture of pseudomembranous colitis includes diarrhea (the most common symptom), abdominal pain, fever, and elevated white blood cell counts. The absence of diarrhea is very infrequent in this setting, making its diagnosis difficult. Some unusual presentation forms include fulminant colitis, toxic megacolon, perforation, and intestinal pseudo-obstruction (5). This paper illustrated an uncommon case of pseudomembranous colitis presenting as FUO in which Tc-99m-HMPAO-labeled leukocytes were the key to achieving the diagnosis.
