Abstract
Aim
To assess the effects of clinical Pilates exercises (CPE) on the level of pain, functional status, flexibility, static and dynamic endurance of the trunk muscles and quality of life (QoL) in patients with lumbar disc herniation.
Materials & methods
Individuals were divided into two groups: the CPE (6 weeks, three-times a week) group (n = 27) and the control group (n = 27). The clinical outcome measures were the visual analog scale for the evaluation of the pain intensity, Oswestry disability index for functional disability, short form-36 for health related QoL, sit and reach and hand finger floor distance test for the flexibility, side-bridge and sit-ups test for the static and dynamic endurance.
Results
At the end of the 6 weeks the amount of decrease in the level of pain and Oswestry disability index, amount of increase in sit-reach test and hand-finger-to-floor distance, duration of the lateral bridge and sits-ups test and most of the short form-36 sub parameters was significantly higher (p < 0.05) in the CPE group.
Conclusion
CPE was an effective and safe method for symptomatic patients with lumbar disc herniation in reducing the pain level and functional disability and improving flexibility, static and dynamic endurance and partially their QoL.
Clinical Trial Registration: NCT03198273 (ClinicalTrials.gov).
Keywords: disability, endurance, exercise, flexibility, low back pain, quality of life, spine
Tweetable abstract
Study finds clinical Pilates exercise was an effective and safe method for symptomatic patients with lumbar disc herniation in reducing the pain level and functional disability and improving flexibility, static and dynamic endurance and partially their quality of life.
Lumbar disc herniation (LDH), which occurs when intervertebral disc material, including the nucleus, cartilage, fragmented bone, annular tissue or any combination of these is locally displaced beyond the disc space boundaries, causes low back pain. Disc degeneration changes the mechanics of the rest of the spine, possibly negatively affecting the function of the other spinal structures such as muscles and ligaments.
Many studies have been conducted showing a positive correlation between disc degeneration at various levels and multifidus muscle atrophy in the lumbar region [1,2]. In addition to LDH, chronic low back pain (CLBP) has also been reported to cause varying degrees of atrophy of the trunk muscles, especially in the multifidus muscles [3]. The multifidus muscle is important for controlling and stabilizing the lumbar spine in a variety of planes of motion. Atrophy in the multifidus muscle may also affect spinal stability and cause the progression of the pathology and the condition to enter a vicious circle. It has been suggested that lumbar muscle strengthening programs in individuals with LDH can be effective in preventing muscle atrophy and lumbar spinal degeneration [1,2]. In addition, it was demonstrated that the lumbopelvic motor control function had decreased in patients with CLBP and the prevalence of CLBP increased in patients with low lumbopelvic motor control function [4]. As a result of chronic pain, the quality of life (QoL) decreases due to the limitation of activities of daily living and disability [5].
The American College of Physicians’ Clinical Practice Guidelines for patients with CLBP strongly recommends that clinicians and patients should initially select non-pharmacological therapy, such as exercise, tai chi, yoga and motor control exercise [6]. Although mind-body exercises such as yoga, tai chi and motor control exercises are recommended in the treatment of individuals with CLBP, no study has been found in the literature evaluating the effect of clinical Pilates exercises (CPE), another mind-body exercise with core stabilization, on individuals with LDH.
CPE is used to enhance functional activity and core strength as well as stimulate neuromuscular re-education. This exercise model has been used in pain treatment, especially ones caused by mechanical and postural defects, and were found to have beneficial effects on pain level and functionality in individuals suffering from chronic mechanical back pain and chronic non specific low back pain [7–9]. Although the effect of Pilates on individuals with low back pain, which is a common symptom of most pathologies associated with the lumbar region, have been studied before, its effectiveness in a homogeneous subgroup such as LDH have not been investigated. Therefore this study was planned to determine the effects of CPE on pain level, functional status, flexibility, static and dynamic endurance of the trunk muscles and QoL in individuals with LDH and compare them with the control group.
Materials & methods
In this study 54 subjects (30 female, 24 male) were randomized by order of arrival into two groups; CPE and a control group (CON). Individuals between 30–60 years of age, who were diagnosed with LDH (bulging and protrusion according to the American Academy of Orthopaedic Surgeons and International Society for the Study of Lumbar Spine classifications) at one or more levels (L3-L4 / L4-L5 / L5-S1) according to MRI results by an orthopedist and who had low back and leg pain for the last 6 weeks with no mental, auditory or visual problems that would undermine communication were included in the study.
Outcome measurements
Patients’ demographic data, such as age, gender, educational status, BMI and cigarette consumption were recorded. The level and segment of the herniated discs were checked and recorded from the MRI reports. Individuals who were included in the study and whose demographic information were questioned were asked to fill in the visual analogue scale, Oswestry Disability Index and Short form-36 questionnaire forms. Then, finger-to-floor distance, sit-and-reach, side-bridge test and sit-up test exercises were evaluated by the physiotherapist. After the exercise sessions were completed, the assessment procedures were similarly repeated and the physical assessments were reassessed by the same physiotherapist.
Visual analogue scale was used to measure the pain intensity. With this valid and reliable method, the level of pain at rest and during exercise and general pain level were evaluated. Individuals were asked to place a mark on a 10 cm horizontal chart (0 = no pain, 10 = worst pain) that corresponded to their pain.
The Oswestry Disability Index, which is considered the gold standard of low back functional outcome tools, was used to assess functional disability with ten questions about various daily activities [10].
The short form-36 (SF-36), which was used to evaluate health related QoL, is composed of eight multi-item scales, which can assess the physical function, role limitations due to physical problems, bodily pain (BP), general health, energy vitality (V), social functioning (SF), role limitations due to emotional problems and mental health. Points were obtained from each sub scale range between 0 (worst health state) – 100 (best health state) [11].
Finger-to-floor distance and sit-and-reach tests were used to assess spinal mobility and flexibility. Finger-to-floor test has excellent validity, reliability and responsiveness so recommended to be used in clinical practice [12]. In the standing position, the patient was asked to bend forward without bending his knees and touch the ground. The distance between the tips of the 3rd fingers and the floor was measured and the difference was recorded. Sit-and-reach test was used for measuring hamstring and low back flexibility and has a proven validity. Patient sat with legs together and feet placed against the box. Then the patient was asked to bend forward as far as possible with extended arms, without bending their knees and remain still for 1–2 s. The remotest distance that was reached was recorded as cm [13].
Side bridge test evaluates the static endurance of the lateral core muscles. In the side-lying position, the legs were in an extension position and the elbow was flexed to 90 degrees. Participants were asked to lift their hips off the table and stand still on their forearms and toes. The time was stopped when the straight body position could no longer be maintained and the duration was recorded in seconds [14]. To evaluate the dynamic endurance of trunk muscles and muscle strength of trunk flexors, sit-up test was used. Participants were asked to do trunk flexion while their knees were already in flexion position and feet were stable. The number of sit-up repetitions within 30 s was recorded [15].
Intervention
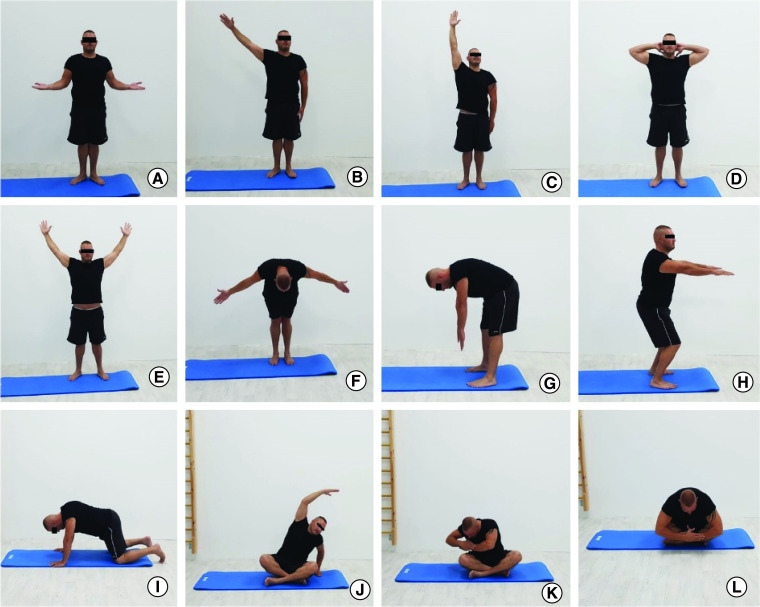
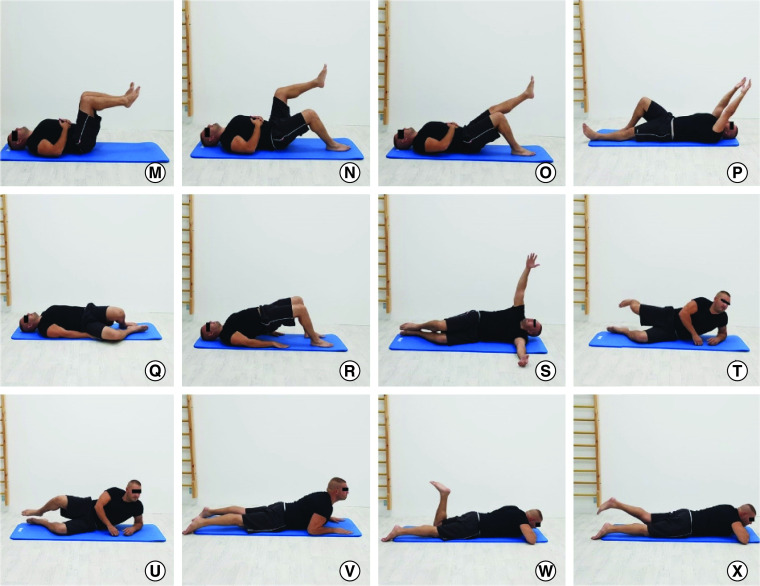
To teach five main areas of focus (breath control, pelvic lumbar region, chest, shoulder positioning, head and neck positioning) a special session was organized for each patient in CPE group. Patients who managed to successfully perform a session of CPE were qualified for group training. The exercises were applied to the patients in the study group 3 days a week for 6 weeks. Exercise sessions were 45–60 min, including a warm-up period, a period in which to perform main exercises and a cool-down period (Table 1). The exercises found in the main exercise phase was progressed at the end of the third week. The control group patients were assessed using the same tests and index and asked to continue their normal daily routines without doing any exercises (Figures 1, 2).
Table 1. . Clinical Pilates exercise program in Figures 1 & 2.
| First session | |
|---|---|
| Teaching five key elements; breath control, pelvic lumbar region, chest, shoulder positioning, head and neck positioning | |
| Warming phase | |
| • Cleopatra (a) • Upper extremity PNF patterns (b) • Toy soldier (c) • Corkscrew (d) |
• Chest stretch (e) • Swinging (f) • Roll down (g) • Mini squat (h) |
| Exercise phase (First 3 weeks): | Exercise phase (second 3 weeks): |
| • Hundreds 1–2 (m) • Scissors 1 (n) • One-leg stretch 1 (o) • Double-leg stretch 1 (p) • Hip twist 1 (q) • Shoulder bridge 1 (r) • Arm openings 1 (s) • Side kick 1 (t) • Clam 1 (u) • Swan dive 1 (v) • One-leg kick (w) • Swimming 1(x) |
• Hundreds 3 • Scissors 2 • One-leg stretch 2 • Double-leg stretch 2 • Hip twist 2 • Shoulder bridge 1 • Arm openings 2 • Side kick 2 • Clam 2 • Swan dive 2 • One-leg kick • Swimming 2 |
| Cooling phase | |
| • Cat stretch (i) • Mermaid (j) • The saw (k) |
• Spine stretch (l) • Chest stretch (e) • Swinging (f) |
Figure 1. . Warming and cooling phase exercises.
Figure 2. . Clinical Pilates Exercise phase training.
Statistical analysis
Data obtained during the study were analyzed with IBM SPSS Statistics V.20.0.0 software. The variables used in the study were indicated by percentage (%), mean ± standard deviation (x ± SD) and number. ANCOVA test was used to compare the pre-test and post-test values of the individuals in the CPE and CON groups. When there was a statistically significant difference between the variables before the training, general linear model analysis was used in the post-training comparisons. The statistical significance level was determined as p < 0.05.
To determine the minimum number of individuals to be included in the study, a power analysis was carried out. Cohen’s effect size was d: 0.8, α: 0.05, β: 0.20. The sample size was calculated as 26 for each group and the total sample size for both groups was 52.
Results
Average age, gender frequency, educational status frequency, BMI and amount of cigarette consumption were found similar (all p > 0.05) (Table 2).
Table 2. . Sociodemographic characteristics of participants.
| Variables | CPE Group, n = 27 | CON Group, n = 27 | p-value† |
|---|---|---|---|
| Age, years, x ± SD | 50.3 ± 6.7 | 50.1 ± 6.5 | 0.910† |
| Gender, n (%) Male Female |
14 (51.9) 13 (48.1) |
10 (37.0) 17 (63.0) |
0.273‡ |
| Educational status, n (%) High School University |
13 (48.1) 14 (51.9) |
16 (59.3) 11 (40.7) |
0.413‡ |
| BMI (kg/m2, x ± SD) |
25.8–2.8 | 25.2–6.5 | 0.528† |
| Smoking, n (%) Yes No |
13–48.1 14–51.9 |
11–40.7 16–59.3 |
0.584‡ |
Mann–Whitney U test.
Chi-square test.
CON: Control; CPE: Clinical Pilates exercise; Standard deviation; x: Mean value.
When the distribution according to the segments was examined in the CPE group (n = 27), it was seen that bulging and protrusion were at the L3-L4 of 14 participants (51.9%), at the L4-L5 of 1 participant (3,7%), at L5-S1 of one participant (3,7%), at L3-L4/L4-L5 of four participants (14,8%), at L4-L5 / L5-S1 of six participants (22.2%) and at L3-L4/L4-L5/L5-S1 of one person (3.7%). In the CON group (n = 27) there were bulging and protrusion at the L3-L4 in 14 participants (51.9%), at the L3-L4/L4-L5 in ten participants (37.0%), at the L4-L5/L5-S1 in two participants (7.4%) at the L3-L4/L4-L5/L5-S1 in one participant (3.7%).
The amount of decrease in the level of pain at rest, general pain and pain during exercise after the treatment of the participants in the CPE group was significantly higher (p < 0.05) (Table 3). Increase in the sit-reach test, hand-finger-to-floor distance, lateral bridge, sits-ups test values and decrease in Oswestry values of the individuals in the CPE group were significantly higher (p < 0.05) (Table 4). No significant difference was found between the groups in the EP sub parameter of the SF-36 (p > 0.05). The amount of increase in physical function, PR, V, mental health, SF, BP and GH scores of the participants in the CPE group were found to be higher (p < 0.05) (Table 5).
Table 3. . Comparison of pain level pre-test and post-test values of individuals.
| Pre-test | Post-test | F | p-value | η2 | ||||
|---|---|---|---|---|---|---|---|---|
| Group | SD | SD | ||||||
| Pain at rest (cm)† | CPE | 2.21 | 1.42 | 0.55 | 0.59 | 32.904 | 0.000 ‡ | 0.392 |
| CON | 1.26 | 1.12 | 1.02 | 1.03 | ||||
| General pain (cm)† | CPE | 3.39 | 1.29 | 1.29 | 0.62 | 26.669 | 0.000 ‡ | 0.343 |
| CON | 2.72 | 0.76 | 2.37 | 0.82 | ||||
| Pain during exercise (cm) | CPE | 4.01 | 1.43 | 1.81 | 1.03 | 10.521 | 0.002 ‡ | 0.171 |
| CON | 3.60 | 0.79 | 3.06 | 1.00 | ||||
There is a difference between the pre-test results.
p < 0.05.
CON: Control; CPE: Clinical Pilates exercise; η2: Eta square (effect size calculation); SD: Standard deviation; x: Mean value.
Table 4. . Comparison of flexibility, endurance and functional status pre-test and post-test values of individuals.
| Pre-test | Post-test | F | p-value | η2 | ||||
|---|---|---|---|---|---|---|---|---|
| Group | SD | SD | ||||||
| Sit-and-reach test (cm) | CPE | -13.56 | 7.90 | -9.59 | 8.34 | 64.746 | 0.000 ‡ | 0.559 |
| CON | -10.33 | 8.11 | -9.93 | 8.03 | ||||
| Finger-floor distance test (cm) | CPE | -13.74 | 9.53 | -9.23 | 9.80 | 89.817 | 0.000 ‡ | 0.642 |
| CON | -11.63 | 8.45 | -11.48 | 8.58 | ||||
| Side-bridge test (s) | CPE | 7.92 | 3.19 | 12.61 | 4.82 | 38.188 | 0.000 ‡ | 0.428 |
| CON | 6.92 | 1.96 | 7.43 | 2.05 | ||||
| Sits-ups test | CPE | 6.96 | 2.79 | 9.52 | 3.00 | 28.830 | 0.000 ‡ | 0.361 |
| CON | 6.26 | 2.31 | 6.63 | 2.19 | ||||
| Oswestry disability index† | CPE | 29.07 | 6.24 | 15.07 | 2.32 | 14.851 | 0.000 ‡ | 0.226 |
| CON | 25.93 | 4.27 | 22.74 | 3.25 | ||||
There is a difference between the pre-test results.
p < 0.05.
CON: Control; CPE: Clinical Pilates exercise; η2: Eta square (effect size calculation); SD: Standard deviation; x: Mean value.
Table 5. . Comparison of quality of life pre-test and post-test values of individuals.
| Pre-test | Post-test | F | p-value | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Group | SD | SD | |||||||
| SF-36 | Physical function† | CPE | 62.59 | 16.95 | 89.26 | 4.94 | 25.512 | 0.000‡ | 0.338 |
| CON | 72.88 | 11.33 | 78.52 | 10.64 | |||||
| Role limitations due to physical problems | CPE | 28.70 | 33.04 | 87.07 | 23.36 | 27.831 | 0.000‡ | 0.358 | |
| CON | 44.44 | 42.37 | 51.92 | 40.57 | |||||
| Role limitations due to emotional problems | CPE | 92.59 | 23.27 | 98.77 | 6.42 | 2.545 | 0.117 | 0.048 | |
| CON | 95.06 | 20.05 | 95.06 | 20.05 | |||||
| Energy vitality† | CPE | 48.52 | 11.16 | 65.96 | 5.83 | 15.603 | 0.000‡ | 0.238 | |
| CON | 55.74 | 8.74 | 61.85 | 7.23 | |||||
| Mental health | CPE | 62.96 | 9.52 | 74.37 | 4.99 | 10.602 | 0.002‡ | 0.172 | |
| CON | 66.07 | 8.76 | 71.56 | 6.69 | |||||
| Social functioning† | CPE | 51.39 | 17.79 | 90.28 | 10.01 | 21.875 | 0.000‡ | 0.300 | |
| CON | 62.96 | 12.25 | 72.69 | 9.83 | |||||
| Bodily pain† | CPE | 42.22 | 16.00 | 81.30 | 10.39 | 28.019 | 0.000‡ | 0.355 | |
| CON | 52.87 | 12.59 | 67.41 | 11.92 | |||||
| General health | CPE | 68.52 | 12.77 | 81.11 | 8.70 | 15.127 | 0.000‡ | 0.229 | |
| CON | 69.81 | 11.72 | 76.11 | 10.59 | |||||
There is a difference between the pre-test results.
p < 0.05.
CON: Control; CPE: Clinical Pilates exercise; η2: Eta square (effect size calculation); SD: Standard deviation; SF-36: Short form-36; x: Mean value.
Discussion
This is the first study in the literature investigating the effect of CPE on individuals with LDH. The results showed that Pilates exercises, which increase core stabilization and motor control, were effective in decreasing the level of pain at rest, general pain and pain during exercise and increasing the flexibility, static and dynamic endurance, functional level and QoL sub parameters except the scores of the role limitations due to emotional problems.
Lumbar low back pain, which can develop for many different reasons, is one of the major symptoms of disc herniation. In this study, it was shown that CPE applied 3 days a week for 6 weeks was effective in reducing the level of pain at rest, general pain and pain during exercise in individuals with LDH. In addition to strengthening, muscle control and core stability, Pilates exercises are mind-body exercise that focuses on flexibility, posture and breathing [16]. CPE may have been able to remove the mind from pain by increasing the individual's body awareness, directing the focus to the quality of movement and keeping it at the moment. Increased motor control and multifidus muscle strength with Pilates exercises, without causing further injury, may account for the reduced pain.
Although many in vitro studies have reported that instability due to mild disc degeneration is associated with increased flexibility, in recent years, there is a common view that there is a tendency toward spinal stiffness with increasing degeneration [17]. To the best of our knowledge, this is the first study to investigate the effects of Pilates exercise on flexibility in individuals with LDH. In our study, it was shown that 6-week CPE is effective in increasing flexibility proven with the improvement in sit and reach and finger and floor tests.
Available evidence suggests that lumbar back pain is associated with decreased strength/endurance, atrophy and fatigue of the lumbar extensor muscles [18]. In patients with CLBP, individualized gradable stabilization exercise lasting 3 weeks has been shown to increase endurance with an increase in active sit-up test and side support test duration [19]. In a study by Bayraktar et al., it was reported that the static endurance of trunk muscles was significantly lower in individuals with LDH compared with healthy subjects. Also, they investigated the effect of an 8-week core stabilization program performed in water and on land on trunk muscle endurance of individuals with LDH. As a result of the study, it was observed that static endurance, which was evaluated by trunk extensor endurance test, trunk flexor endurance test and lateral bridge test, improved [20]. Aiming at lumbar stabilization, CPE is primarily applied to increase neuromuscular control, strength and endurance of the muscles, which are considered central to maintaining dynamic spinal and trunk stability. With the increase in core endurance, musculoskeletal injuries are prevented and functionality is increased by allowing optimal production and control of force and movement to the terminal segment during kinetic chain activity. In this study, the static endurance of the trunk was determined by the side-bridge test and dynamic endurance was determined by using the sit-ups test. As a result of the study, 6-week progressive core stabilization-based CPE was shown to be effective in improving static and dynamic trunk muscle endurance without increasing pain.
CLBP causes restriction of mobility resulting in morphological changes in the lumbar muscles. Reduced muscle strength and endurance have a negative impact on lumbar stability and can lead to functional restrictions. In patients with LDH a moderate-to-high correlation between endurance time and disability [21]. Besides the relationship between chronic pain, strength/endurance and disability, in some individuals with lumbar low back pain, pain and fear of re-injury and faulty beliefs trigger movement avoidance behaviors, causing further pain and disability [22]. Although the level of kinesiophobia or fear avoidance was not evaluated in our study, the decrease in pain level, especially during exercise, might be one of the contributing factors in reducing disability. Another possible cause was increased trunk static and dynamic muscle endurance.
Due to the concomitant psychosocial stress, pain and decrease in vitality and functional status, CLBP was linked to a lower health related QoL [23]. There is some evidence in the literature that Pilates exercises improve health related QoL in individuals with CLBP [24–26]. In a study using the Pilates method, regarding the QoL measured using the SF-36 questionnaire, improvements were observed in functional capacity, pain and vitality domains [25]. Similarly, in our study, physical function, energy-vitality, bodily pain as well as mental health, social functioning, role limitations due to physical problems and general health scores of the participants in the CPE group. As it improves motivation and social cohesiveness, we believe that conducting the exercises in groups is the explanation for the improvement in social functioning. Although, in a study there was a significant improvement in the perception of physical and psychological health of individuals with low back pain who practiced Pilates exercise daily, no improvement was observed in our study in the role limitations due to emotional problems domain [24]. The fact that the exercise program is limited to 6 weeks may be the reason for the lack of improvement in emotional roles. We contend that the effects of CPE on QoL in individuals with LDH may be prominent with longer-term exercises.
This is the first study in the literature investigating the safety and the effect of CPE on individuals with LDH. For this reason, it was not aimed to compare the effectiveness of the control group by applying a different exercise method. We believe that the results obtained from this short-term study will guide future studies. However, the effect of future long-term studies on the outcomes compared with other exercise training should be examined. Since our study was of short duration, the effect of CPE on intervertebral disc structure could not be examined objectively with MRI, so we suggest the use of MRI in future studies.
Conclusion
In the treatment of symptomatic LDH; core stability-based, 6 weeks progressive CPE are safe and effective mind and body exercise methods that can be applied by physiotherapists to reduce pain and disability and to improve flexibility, static and dynamic endurance and QoL.
Summary points.
In the treatment of symptomatic lumbar disc herniation; core stability-based, clinical Pilates exercises are safe and effective mind and body exercise methods that can be applied by physiotherapists.
About 6 weeks progressive and structured clinical Pilates exercises program can be used to reduce pain and disability and to improve flexibility, static and dynamic endurance and quality of life in patients with Lumbar disc herniation.
Footnotes
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by G Taşpınar, E Angın and S Oksuz. The first draft of the manuscript was written by G Taşpınar; and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The study was approved by the Eastern Mediterranean University Scientific Research and Health Ethics Committee (06.03.2017, 2017/39-10). Individuals were asked to sign the informed consent form for participation in the study. This study was recorded on ClinicalTrials.gov (NCT03198273).
Data sharing statement
The authors certify that this manuscript reports original clinical trial data. Deidentified, individual data that underlie the results reported in this article (text, tables, figures and appendices), along with the study protocol and data set will be available indefinitely following publication. Data will be shared with researchers who provide a methodologically sound proposal for individual participant data meta-analysis via request to the corresponding author.
References
Papers of special note have been highlighted as: • of interest
- 1.Liu C, Xue J, Liu J et al. Is there a correlation between upper lumbar disc herniation and multifidus muscle degeneration? A retrospective study of MRI morphology. BMC Musculoskelet. Disord. 22(1), 92 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun D, Liu P, Cheng J, Ma Z, Liu J, Qin T. Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation. BMC Musculoskelet. Disord. 18(1), 167 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamaz M, Kireşi D, Oğuz H, Emlik D, Levendoğlu F. CT measurement of trunk muscle areas in patients with chronic low back pain. Diagn. Interv. Radiol. 13(3), 144–148 (2007). [PubMed] [Google Scholar]
- 4.Jung SH, Hwang UJ, Ahn SH, Kim HA, Kim JH, Kwon OY. Lumbopelvic motor control function between patients with chronic low back pain and healthy controls: a useful distinguishing tool: The STROBE study. Medicine (Baltimore). 99(15), e19621 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kose G, Tastan S, Temiz NC, Sari M, Izci Y. The effect of low back pain on daily activities and sleep quality in patients with lumbar disc herniation: a pilot study. J. Neurosci. Nurs. 51(4), 184–189 (2019). [DOI] [PubMed] [Google Scholar]
- 6.Qaseem A, Wilt TJ, McLean RM et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 166(7), 514–530 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Lin HT, Hung WC, Hung JL, Wu PS, Liaw LJ, Chang JH. Effects of pilates on patients with chronic non-specific low back pain: a systematic review. J. Phys. Ther. Sci. 28(10), 2961–2969 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patti A, Bianco A, Paoli A et al. Effects of Pilates exercise programs in people with chronic low back pain: a systematic review. Medicine (Baltimore). 94(4), e383 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patti A, Bianco A, Paoli A et al. Pain perception and stabilometric parameters in people with chronic low back pain after a pilates exercise program: a randomized controlled trial. Medicine (Baltimore). 95(2), e2414 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yakut E, Düger T, Oksüz C et al. Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine 29(5), 581–585 (2004). [DOI] [PubMed] [Google Scholar]
- 11.Li L, Wang HM, Shen Y. Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J. Epidemiol. Community Health 57(4), 259–263 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch. Phys. Med. Rehabil. 82(11), 1566–1570 (2001). [DOI] [PubMed] [Google Scholar]
- 13.Ayala F, Sainz de Baranda P, De Ste Croix M, Santonja F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys. Ther. Sport 13(4), 219–226 (2012). [DOI] [PubMed] [Google Scholar]
- 14.McGill S, Childs A, Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch. Phys. Med. Rehabil. 80(8), 941–944 (1999). [DOI] [PubMed] [Google Scholar]
- 15.Kato S, Murakami H, Inaki A et al. Innovative exercise device for the abdominal trunk muscles: an early validation study. PLOS ONE 12(2), e0172934 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bayraktar D, Guclu-Gunduz A, Lambeck J, Yazici G, Aykol S, Demirci H. A comparison of water-based and land-based core stability exercises in patients with lumbar disc herniation: a pilot study. Disabil. Rehabil. 38(12), 1163–1171 (2016). [DOI] [PubMed] [Google Scholar]
- 17.Smith K, Smith E. Integrating Pilates-based core strengthening into older adult fitness programs: implications for practice. Top. Geriatr. Rehabil. 21(1), 57–67 (2005). [Google Scholar]
- 18.Galbusera F, van Rijsbergen M, Ito K, Huyghe JM, Brayda-Bruno M, Wilke HJ. Ageing and degenerative changes of the intervertebral disc and their impact on spinal flexibility. Eur. Spine J. 23(3), 324–332 (2014). [DOI] [PubMed] [Google Scholar]
- 19.Steele J, Bruce-Low S, Smith D. A reappraisal of the deconditioning hypothesis in low back pain: review of evidence from a triumvirate of research methods on specific lumbar extensor deconditioning. Curr. Med. Res. Opin. 30(5), 865–911 (2014). [DOI] [PubMed] [Google Scholar]
- 20.Lee HS, Kim DJ, Oh Y, Min K, Ryu JS. The effect of individualized gradable stabilization exercises in patients with chronic low back pain: case-control study. J. Back. Musculoskelet. Rehabil. 29(3), 603–610 (2016). [DOI] [PubMed] [Google Scholar]
- 21.Dedering A, Harms-Ringdahl K, Nèmeth G. Back extensor muscle fatigue in patients with lumbar disc herniation. Eur. Spine J. 15(5), 559–569 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLOS ONE 12(7), e0180788 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agnus Tom A, Rajkumar E, John R, Joshua George A. Determinants of quality of life in individuals with chronic low back pain: a systematic review. Health Psychol. Behav. Med. 10(1), 124–144 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Notarnicola A, Fischetti F, Maccagnano G, Comes R, Tafuri S, Moretti B. Daily pilates exercise or inactivity for patients with low back pain: a clinical prospective observational study. Eur. J. Phys. Rehabil. Med. 50(1), 59–66 (2014). [PubMed] [Google Scholar]
- 25.Natour J, Cazotti L de A, Ribeiro LH, Baptista AS, Jones A. Pilates improves pain, function and quality of life in patients with chronic low back pain: a randomized controlled trial. Clin. Rehabil. 29(1), 59–68 (2015). [DOI] [PubMed] [Google Scholar]
- 26.Yang CY, Tsai YA, Wu PK, Ho SY, Chou CY, Huang SF. Pilates-based core exercise improves health-related quality of life in people living with chronic low back pain: a pilot study. J. Bodyw. Mov. Ther. 27, 294–299 (2021). [DOI] [PubMed] [Google Scholar]